Abstract
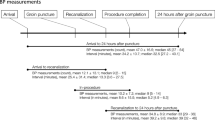
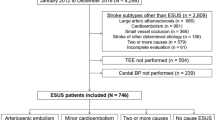
Higher blood pressure variability (BPV) has been proven associated with worse functional outcome after endovascular treatment (EVT). However, this association is not established according to different stroke etiologies. In this study, we compared patients with the two highest proportions of stroke etiologies—cardioembolism (CE) and large-artery atherosclerosis (LAA), aiming to explore appropriate strategies of BP management for different etiologies. We enrolled patients with large vessel occlusion (LVO) in anterior circulation who underwent EVT and achieved successful recanalization retrospectively. 24-h blood pressure (BP) and BPV measured as blood pressure reduction (BPr), standard deviation (SD), coefficient of variation (CV), successive variation (SV), average real variability (ARV) after EVT were collected for systolic blood pressure (SBP) and diastolic blood pressure (DBP). The favorable outcome was defined as functional independence by 90-day modified Rankin Scale (mRS 0–2). In our cohort, higher BPV parameters significantly resulted in 90d functional dependence in CE-LVO patients (SBPSV OR: 1.083, 95%CI = 1.009–1.163; SBPARV OR: 1.121, 95%CI = 1.019–1.233; DBPSD OR: 1.124, 95%CI = 1.007–1.1256; DBPCV OR: 1.078, 95%CI = 1.002–1.161). However, for LAA-LVO patients, no positive results correlated 90d functional dependence with 24-hour BPV. Additionally, 90d functional dependence in CE patients with poor collaterals were significantly dependent on post-procedural BPV (DBPmax OR: 1.044, 95%CI = 1.002–1.087; DBPSD OR: 1.229, 95%CI = 1.022–1.1.479; DBPCV OR: 1.143, 95%CI = 1.009–1.295). Whereas to patients with good collaterals, there did not exist such a correlation. In summary, stroke etiologies should probably be taken into consideration to optimize individualized BP management strategies.

In order to achieve better clinical outcomes for patients with acute ischemic stroke due to large vessel occlusion, stricter blood pressure management should be taken in cardioembolic stroke patients in contrast with large artery atherosclerotic stroke patients after successful endovascular therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data and materials are available upon reasonable request.
References
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–e418.
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Liu D, Nie X, Pan Y, Yan H, Pu Y, Wei Y, et al. Adverse outcomes associated with higher mean blood pressure and greater blood pressure variability immediately after successful embolectomy in those with acute ischemic stroke, and the influence of pretreatment collateral circulation status. J Am Heart Assoc. 2021;10:e019350.
Mistry EA, Sucharew H, Mistry AM, Mehta T, Arora N, Starosciak AK, et al. Blood Pressure after Endovascular Therapy for Ischemic Stroke (BEST): a multicenter prospective cohort study. Stroke. 2019;50:3449–55.
Nisar T, Tofade T, Lebioda K, Abu-Hadid O, Khandelwal P. Association of 24-hour blood pressure parameters post-thrombectomy with functional outcomes according to collateral status. J Neurol Sci. 2022;441:120369.
Chang JY, Jeon SB, Jung C, Gwak DS, Han MK. Postreperfusion blood pressure variability after endovascular thrombectomy affects outcomes in acute ischemic stroke patients with poor collateral circulation. Front Neurol. 2019;10:346.
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 h after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21.
Mistry EA, Mayer SA, Khatri P. Blood pressure management after mechanical thrombectomy for acute ischemic stroke: a survey of the strokenet sites. J Stroke Cerebrovasc Dis. 2018;27:2474–8.
Anadani M, Orabi MY, Alawieh A, Goyal N, Alexandrov AV, Petersen N, et al. Blood pressure and outcome after mechanical thrombectomy with successful revascularization. Stroke. 2019;50:2448–54.
Mazighi M, Richard S, Lapergue B, Sibon I, Gory B, Berge J, et al. Safety and efficacy of intensive blood pressure lowering after successful endovascular therapy in acute ischaemic stroke (BP-TARGET): a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2021;20:265–74.
Yang P, Song L, Zhang Y, Zhang X, Chen X, Li Y, et al. Intensive blood pressure control after endovascular thrombectomy for acute ischaemic stroke (ENCHANTED2/MT): a multicentre, open-label, blinded-endpoint, randomised controlled trial. Lancet. 2022;400:1585–96.
Nam HS, Kim YD, Heo J, Lee H, Jung JW, Choi JK, et al. Intensive vs conventional blood pressure lowering after endovascular thrombectomy in acute ischemic stroke: the OPTIMAL-BP randomized clinical trial. JAMA. 2023;330:832–42.
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368:2355–65.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Eames PJ, Blake MJ, Dawson SL, Panerai RB, Potter JF. Dynamic cerebral autoregulation and beat to beat blood pressure control are impaired in acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2002;72:467–72.
Nour M, Scalzo F, Liebeskind DS. Ischemia-reperfusion injury in stroke. Interv Neurol. 2013;1:185–99.
Manning LS, Rothwell PM, Potter JF, Robinson TG. Prognostic significance of short-term blood pressure variability in acute stroke: systematic review. Stroke. 2015;46:2482–90.
Matusevicius M, Cooray C, Bottai M, Mazya M, Tsivgoulis G, Nunes AP, et al. Blood pressure after endovascular thrombectomy: modeling for outcomes based on recanalization status. Stroke 2020;51:519–25.
Adams HP Jr., Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24:35–41.
Huo X, Sun D, Raynald, Jia B, Tong X, Wang A, et al. Endovascular treatment in acute ischemic stroke with large vessel occlusion according to different stroke subtypes: data from ANGEL-ACT registry. Neurol Ther. 2022;11:151–65.
Guglielmi V, LeCouffe NE, Zinkstok SM, Compagne KCJ, Eker R, Treurniet KM, et al. Collateral circulation and outcome in atherosclerotic versus cardioembolic cerebral large vessel occlusion. Stroke 2019;50:3360–8.
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR. 2009;30:525–31.
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 h after acute ischemic stroke. N Engl J Med. 2008;359:1317–29.
Anadani M, Arthur AS, Alawieh A, Orabi Y, Alexandrov A, Goyal N, et al. Blood pressure reduction and outcome after endovascular therapy with successful reperfusion: a multicenter study. J Neurointerv Surg. 2020;12:932–6.
Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Schächinger H, Langewitz W, Schmieder RE, Rüddel H. Comparison of parameters for assessing blood pressure and heart rate variability from non-invasive twenty-four-hour blood pressure monitoring. J Hypertens Suppl. 1989;7:S81–84.
Hastie CE, Jeemon P, Coleman H, McCallum L, Patel R, Dawson J, et al. Long-term and ultra long-term blood pressure variability during follow-up and mortality in 14,522 patients with hypertension. Hypertension. 2013;62:698–705.
Ko Y, Park JH, Yang MH, Ko SB, Han MK, Oh CW, et al. The significance of blood pressure variability for the development of hemorrhagic transformation in acute ischemic stroke. Stroke. 2010;41:2512–8.
Tiedt S, Wollenweber FA. Response by Tiedt and Wollenweber to letter regarding article, “Stroke etiology modifies the effect of endovascular treatment in acute stroke”. Stroke. 2020;51:e159–e160.
Rebello LC, Bouslama M, Haussen DC, Grossberg JA, Dehkharghani S, Anderson A, et al. Stroke etiology and collaterals: atheroembolic strokes have greater collateral recruitment than cardioembolic strokes. Eur J Neurol. 2017;24:762–7.
Pan YT, Lee JD, Lin YH, Huang YC, Weng HH, Lee M, et al. Comparisons of outcomes in stroke subtypes after intravenous thrombolysis. SpringerPlus. 2016;5:47.
Tu HT, Campbell BC, Christensen S, Desmond PM, De Silva DA, Parsons MW, et al. Worse stroke outcome in atrial fibrillation is explained by more severe hypoperfusion, infarct growth, and hemorrhagic transformation. Int J Stroke: Off J Int Stroke Soc. 2015;10:534–40.
Sun B, Shi Z, Pu J, Yang S, Wang H, Yang D, et al. Effects of mechanical thrombectomy for acute stroke patients with etiology of large artery atherosclerosis. J Neurol Sci. 2019;396:178–83.
Desilles JP, Rouchaud A, Labreuche J, Meseguer E, Laissy JP, Serfaty JM, et al. Blood-brain barrier disruption is associated with increased mortality after endovascular therapy. Neurology. 2013;80:844–51.
Regenhardt RW, Das AS, Stapleton CJ, Chandra RV, Rabinov JD, Patel AB, et al. Blood pressure and penumbral sustenance in stroke from large vessel occlusion. Front Neurol. 2017;8:317.
Desai SM, Jha RM, Linfante I. Collateral circulation augmentation and neuroprotection as adjuvant to mechanical thrombectomy in acute ischemic stroke. Neurology 2021;97:S178–s184.
Berkhemer OA, Jansen IG, Beumer D, Fransen PS, van den Berg LA, Yoo AJ, et al. Collateral status on baseline computed tomographic angiography and intra-arterial treatment effect in patients with proximal anterior circulation stroke. Stroke. 2016;47:768–76.
Jing Z, Shi C, Zhu L, Xiang Y, Chen P, Xiong Z, et al. Chronic cerebral hypoperfusion induces vascular plasticity and hemodynamics but also neuronal degeneration and cognitive impairment. J Cereb Blood Flow Metab. 2015;35:1249–59.
Elstad M, Walløe L, Chon KH, Toska K. Low-frequency fluctuations in heart rate, cardiac output and mean arterial pressure in humans: what are the physiological relationships? J Hypertens. 2011;29:1327–36.
Buchbinder WC, Sugarman H. Arterial blood pressure in cases of auricular fibrillation, measured directly. Arch Intern Med. 1940;66:625–42.
Olbers J, Gille A, Ljungman P, Rosenqvist M, Östergren J, Witt N. High beat-to-beat blood pressure variability in atrial fibrillation compared to sinus rhythm. Blood Press. 2018;27:249–55.
Maïer B, Dargazanli C, Bourcier R, Kyheng M, Labreuche J, Mosimann PJ, et al. Effect of steady and dynamic blood pressure parameters during thrombectomy according to the collateral status. Stroke. 2020;51:1199–206.
Mehndiratta MM, Khan M, Mehndiratta P, Wasay M. Stroke in Asia: geographical variations and temporal trends. J Neurol Neurosurg Psychiatry. 2014;85:1308–12.
Kim BJ, Kim JS. Ischemic stroke subtype classification: an Asian viewpoint. J Stroke. 2014;16:8–17.
Funding
This study was supported by the Natural Science Research Project of the Universities of Anhui Educational Committee (2023AH040256, 2022AH040180, KJ2021A0843), the Scientific Research Fund Project for Talent Introduction of Yijishan Hospital, Wannan Medical College (No. YR202210), the Clinical Medical Research Translational Project (202204295107020017), Anhui Provincial Health Backbone Talent Training Target Project and Anhui Province University Excellent Top Talent Cultivation Project.
Author information
Authors and Affiliations
Contributions
HW, YG, XH, and ZZ contributed to the study concept and design. HW and YG contributed to the draft the manuscript. YJ and XX contributed to the acquisition and analysis of the data. JX and YS contributed to image review. QY contributed to revise the manuscript. XH and ZZ are responsible for the overall content as guarantors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the local ethics committee. Consent to participate was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Guo, Y., Xu, J. et al. Blood pressure variability and outcome in atherosclerosis versus cardioembolism cerebral large vessel occlusion after successful thrombectomy. Hypertens Res 47, 898–909 (2024). https://doi.org/10.1038/s41440-023-01500-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01500-x
Keywords
This article is cited by
-
Salt and seasonal variation research in Asia
Hypertension Research (2024)