Abstract
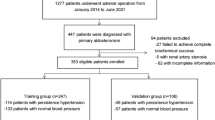
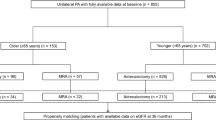
Hypertension cure following adrenalectomy in unilateral primary aldosteronism (PA) remains uncertain. Previous meta-analyses have shown highly variable surgical outcomes. Our study aimed to determine the unknown proportion of complete clinical and biochemical success in tertiary and quaternary referral centers. We conducted a systematic review and meta-analysis of studies reporting surgical outcomes of unilateral PA patients within the Surgical Outcome of PRimary Aldosteronism progNostic mOdels (SOPRANO) study. From 27 publications we identified 32 eligible studies, of which 22 were judged to be at low risk of bias. Eighteen were single-center studies, while fourteen were multi-center studies, with patients recruited from 132 referral centers worldwide. Adrenalectomy was performed on 5887 patients, with 4861 (83%) included in the final analysis. The pooled estimates of complete clinical and biochemical success for all studies were 39% (95% CI: 34–44%) and 99% (95% CI: 96–99%), respectively, similar to that found for studies at low risk of bias. Multivariate meta-regression analyses for all studies and low-bias risk studies revealed that BMI (P < 0.01), recruitment time period (P < 0.01), and hypertension duration (P < 0.05) inversely correlated with complete clinical success, while BMI (P < 0.05) and the number of enrolled centers (P < 0.05) inversely correlated with complete biochemical success. In summary, our findings offer robust estimates of complete clinical and biochemical success rates following adrenalectomy for unilateral PA in tertiary and quaternary referral centers and identify new potential effect modifiers that can help clinicians to inform and counsel patients about post-surgery expectations, guaranteeing effective treatment and ultimately enhancing outcomes.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data used for the work are available from the corresponding author upon reasonable request.
References
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension. 2018;72:658–66.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Marzano L. Primary aldosteronism and coronary-pulmonary artery fistula: coincidence or causal link? A case report and literature review. Arter Hypertens. 2021;25:47–52.
Catena C, Colussi G, Marzano L, Sechi LA. Aldosterone and the heart: from basic research to clinical evidence. Horm Metab Res. 2012;44:181–7.
Marzano L, Colussi G, Sechi LA, Catena C. Adrenalectomy is comparable with medical treatment for reduction of left ventricular mass in primary aldosteronism: meta-analysis of long-term studies. Am J Hypertens. 2015;28:312–8.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J Am Coll Cardiol. 2017;69:1811–20.
Kayser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35.
Douma S, Petidis K, Doumas M, Papaefthimiou P, Triantafyllou A, Kartali N, et al. Prevalence of primary hyperaldosteronism in resistant hypertension: a retrospective observational study. Lancet. 2008;371:1921–6.
Parasiliti-Caprino M, Lopez C, Prencipe N, Lucatello B, Settanni F, Giraudo G, et al. Prevalence of primary aldosteronism and association with cardiovascular complications in patients with resistant and refractory hypertension. J Hypertens. 2020;38:1841–8.
Rossi GP, Bisogni V, Bacca AV, Belfiore A, Cesari M, Concistre A, et al. The 2020 Italian Society of Arterial Hypertension (SIIA) practical guidelines for the management of primary aldosteronism. Int J Cardiol Hypertens. 2020;5:100029.
Vorselaars W, Nell S, Postma EL, Zarnegar R, Drake FT, Duh QY, et al. Clinical outcomes after unilateral adrenalectomy for primary aldosteronism. JAMA Surg. 2019;154:e185842.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Marzano L, Husain-Syed F, Reis T, Ronco C, Zanella M. Assessment of performance of stratum-specific likelihood ratios of the aldosteronoma resolution score for predicting hypertension cure after adrenalectomy for primary aldosteronism: a systematic review and meta-analysis. J Hum Hypertens. 2022; https://doi.org/10.1038/s41371-022-00731-8.
Zhou Y, Zhang M, Ke S, Liu L. Hypertension outcomes of adrenalectomy in patients with primary aldosteronism: a systematic review and meta-analysis. BMC Endocr Disord. 2017;17:61.
Benham JL, Eldoma M, Khokhar B, Roberts DJ, Rabi DM, Kline GA. Proportion of patients with hypertension resolution following adrenalectomy for primary aldosteronism: a systematic review and meta-analysis. J Clin Hypertens. 2016;18:1205–12.
Marzano L, Kazory A, Husain-Syed F, Ronco C. Prognostic models to predict complete resolution of hypertension after adrenalectomy in primary aldosteronism: a systematic review and meta-analysis. Clin Endocrinol. 2023, https://doi.org/10.1111/cen.14918).
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rucker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10:476–83.
Jackson JB D, Baker R. How does the DerSimonian and Laird procedure for random effects meta-analysis compare with its more efficient but harder to compute counterparts? J Stat Plan Inference. 2010;140:961–70.
Tanriver-Ayder E, Faes C, van de Casteele T, McCann SK, Macleod MR. Comparison of commonly used methods in random effects meta-analysis: application to preclinical data in drug discovery research. BMJ Open Sci. 2021;5:e100074.
da Costa BR, Juni P. Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J. 2014;35:3336–45.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions. In. Cochrane handbook for systematic reviews of interventions. Version 6.3. https://training.cochrane.org/handbook/current/chapter-10#section-10-10. Published Version 6.3.). Version 6.3 edn (2022).
Huang-Fu YC, Du YQ, Yu LP, Xu T. [Risk factors of persistent hypertension in primary aldosteronism patients after surgery]. Beijing Da Xue Xue Bao Yi Xue Ban. 2022;54:686–91.
Araujo-Castro M, Paja Fano M, Gonzalez Boillos M, Pla Peris B, Pascual-Corrales E, Garcia Cano AM, et al. Adrenal venous sampling in primary aldosteronism: experience of a Spanish multicentric study (Results from the SPAIN-ALDO Register). Endocrine. 2022; https://doi.org/10.1007/s12020-022-03122-8.
Wang H, Wang F, Zhang Y, Wen J, Dong D, Chang X, et al. Surgical outcomes of aldosterone-producing adenoma on the basis of the histopathological findings. Front Endocrinol (Lausanne). 2021;12:663096.
Rossi GP, Rossitto G, Amar L, Azizi M, Riester A, Reincke M, et al. Clinical outcomes of 1625 patients with primary aldosteronism subtyped with adrenal vein sampling. Hypertension. 2019;74:800–8.
Muth A, Ragnarsson O, Johannsson G, Wangberg B. Systematic review of surgery and outcomes in patients with primary aldosteronism. Br J Surg. 2015;102:307–17.
Morisaki M, Kurihara I, Itoh H, Naruse M, Takeda Y, Katabami T, et al. Predictors of clinical success after surgery for primary aldosteronism in the Japanese nationwide cohort. J Endocr Soc. 2019;3:2012–22.
Kim RM, Lee J, Soh EY. Predictors of resolution of hypertension after adrenalectomy in patients with aldosterone-producing adenoma. J Korean Med Sci. 2010;25:1041–4.
Guo C, Ricchiuti V, Lian BQ, Yao TM, Coutinho P, Romero JR, et al. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation. 2008;117:2253–61.
Caprio M, Feve B, Claes A, Viengchareun S, Lombes M, Zennaro MC. Pivotal role of the mineralocorticoid receptor in corticosteroid-induced adipogenesis. FASEB J. 2007;21:2185–94.
Goodfriend TL, Kelley DE, Goodpaster BH, Winters SJ. Visceral obesity and insulin resistance are associated with plasma aldosterone levels in women. Obes Res. 1999;7:355–62.
Harada E, Mizuno Y, Katoh D, Kashiwagi Y, Morita S, Nakayama Y, et al. Increased urinary aldosterone excretion is associated with subcutaneous not visceral, adipose tissue area in obese individuals: a possible manifestation of dysfunctional subcutaneous adipose tissue. Clin Endocrinol. 2013;79:510–6.
Er LK, Lin MC, Tsai YC, Hsiao JK, Yang CY, Chang CC, et al. Association of visceral adiposity and clinical outcome among patients with aldosterone producing adenoma. BMJ Open Diabetes Res Care. 2020;8:e001153.
Shibayama Y, Wada N, Baba S, Miyano Y, Obara S, Iwasaki R, et al. Relationship between visceral fat and plasma aldosterone concentration in patients with primary aldosteronism. J Endocr Soc. 2018;2:1236–45.
Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217.
Saiki A, Otsuki M, Mukai K, Hayashi R, Shimomura I, Kurihara I, et al. Basal plasma aldosterone concentration predicts therapeutic outcomes in primary aldosteronism. J Endocr Soc. 2020;4:bvaa011.
He XQ, Yang S, Wu JL, Wang DL, Ren W, Cheng QF, et al. A Fisher discriminant model to predict the outcome of postoperative blood pressure in primary aldosteronism. Zhonghua Yi Xue Za Zhi. 2016;96:3379–83.
Worth PJ, Kunio NR, Siegfried I, Sheppard BC, Gilbert EW. Characteristics predicting clinical improvement and cure following laparoscopic adrenalectomy for primary aldosteronism in a large cohort. Am J Surg. 2015;210:702–9.
Dominguez DA, Chatani P, Murphy R, Copeland AR, Chang R, Sadowski SM, et al. Contralateral suppression index does not predict clinical cure in patients undergoing surgery for primary aldosteronism. Ann Surg Oncol. 2021; https://doi.org/10.1245/s10434-021-09692-7.
Aronova A, Gordon BL, Finnerty BM, Zarnegar R, Fahey TJ 3rd. Aldosteronoma resolution score predicts long-term resolution of hypertension. Surgery. 2014;156:1387–92.
Romero-Velez G, Laird AM, Barajas ME, Sierra-Salazar M, Herrera MF, Libutti SK, et al. Outcomes of adrenalectomy and the aldosteronoma resolution score in the black and hispanic population. World J Surg. 2021;45:1475–82.
Fujita N, Hatakeyama S, Yamamoto H, Tobisawa Y, Yoneyama T, Yoneyama T, et al. Implication of aortic calcification on persistent hypertension after laparoscopic adrenalectomy in patients with primary aldosteronism. Int J Urol. 2016;23:412–7.
Loh WJ, Lim DST, Loh LM, Kek PC. Factors associated with resolution of hypertension after adrenalectomy in patients with primary aldosteronism. Endocrinol Metab. 2018;33:355–63.
Namekawa T, Utsumi T, Tanaka T, Kaga M, Nagano H, Kono T, et al. Hypertension cure following laparoscopic adrenalectomy for hyperaldosteronism is not universal: trends over two decades. World J Surg. 2017;41:986–90.
Kaneko H, Umakoshi H, Ogata M, Wada N, Ichijo T, Sakamoto S, et al. Machine learning-based models for predicting clinical outcomes after surgery in unilateral primary aldosteronism. Sci Rep. 2022;12:5781.
Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. 2021;21:189.
Acknowledgements
We thank all principal investigators who have replied to our inquiries and/or provided us with further information or data concerning their publications. Their help enabled us to include as many studies as possible in analysis. We want to thank Hironobu Umakoshi, Hoi-Tik Leung, Jacopo Burrello, Jinbo Hu, Ludwig Pasquier, Marta Araujo-Castro, Shingo Hatakeyama, Takanobu Utsumi, Xiaoqun He, and Yu-chao Huang-Fu.
Author information
Authors and Affiliations
Contributions
Concept and design of the study: LM, CR. Literature research and clinical advice: LM, CR. Acquisition, analyses, or interpretation of data: LM. Manuscript drafting: LM. Critical revision of the manuscript for important intellectual content: LM, CR. Study supervision: LM, CR.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marzano, L., Ronco, C. Clinical and biochemical outcomes after adrenalectomy for primary aldosteronism in tertiary and quaternary referral centers: data from SOPRANO study. Hypertens Res 47, 721–734 (2024). https://doi.org/10.1038/s41440-023-01554-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01554-x