Abstract
This case report highlights the successful management, by vitrectomy alone, of a case of chronic phacolytic glaucoma secondary to a dislocated hypermature lens in the vitreous of a patient with ectopia lentis et pupillae (ELP). The features and complications of ELP are discussed.
Similar content being viewed by others
Main
Sir,
We report the successful management of a case of chronic, uncontrolled phacolytic glaucoma secondary to a dislocated hypermature lens in the vitreous of a patient with ectopia lentis et pupillae (ELP). Using vitreo-lensectomy alone, good subsequent medical control of the intraocular pressure (TOP) was permitted.
Case report
A 51-year-old gentleman was first seen in the clinic in 1994 following referral for aphakic contact lenses. Previously, he had been seen elsewhere with ‘congenitally dislocated lenses and an abnormality of the iris’. His visual acuity (VA) at presentation was 6/12 right with +14.50/−2.00×30 and 6/12 left with +14.50/−0.75×180.
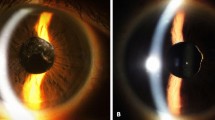
In March 1999 he re-presented complaining of intermittent blurred vision in his left eye. The left VA was 6/12 and corneal epithelial oedema with a raised IOP of 37 mmHg in the left eye was documented. This responded to treatment with guttae (g) timolol 0.5% b.d. and g dorzolamide 2% b.d. Over the following 6 months, the left eye sustained two brief episodes of uveitis, complicated by elevated IOP. The uveitis responded to treatment with g betamethasone q.d.s., but persisting raised IOP required the substitution of g latanoprost o.n. for dorzolamide. He then remained stable until November 2001, when he presented to the eye casualty with acute blurring of vision in the same eye. His left VA was 6/18 and there was corneal epithelial oedema with an IOP of 57 mmHg. There was no evidence of anterior uveitis. Gonioscopy revealed open angles. A diagnosis of ELP was established, complicated by phacolytic glaucoma from a hypermature lens in the vitreous (Figure 1). The IOP responded to intravenous acetazolamide 500 mg stat, oral acetazolamide 250 mg t.d.s., and topical treatment consisting of g timolol 0.5% b.d. and g latanoprost o.n. G dexamethasone 0.1% q.d.s. was also administered. The IOP was normal the next day and the acetazolamide was discontinued. However, 6 days later the IOP measured 46 mmHg in the left despite unchanged topical therapy. It was considered that the only definitive treatment would be to remove the exciting hypermature lens from the vitreous.
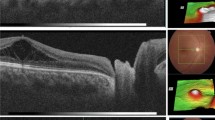
The problem of the ectopic poorly dilating pupil was solved by the use of standard iris hooks, which achieved an excellent view of the fundus. A posterior vitreous detachment was noted during the three-port pars plana vitrectomy, and the very dense hypermature lens was removed using a fragmatome. Heavy liquid was not used and no damage to the retina was seen. The IOP was 20 mmHg 24 h postoperatively, and the pupil returned to its preoperative appearance. At the time of writing this report (3 months postoperatively), the IOP was 21 mmHg with treatment of g timolol 0.25% b.d. and g latanoprost o.n.
Comment
ELP is a rare, inherited, congenital disorder characterised by typical ocular abnormalities but with no systemic manifestations.1,2,3,4,5,6,7 The condition is usually an autosomal recessive trait with variable expression, often with suspected or known consanguinity.1,2,3,4,5,6,7 Isolated cases have been described,4 and one reported pedigree suggested an autosomal dominant pattern of inheritance.6 The typical features of ELP are bilateral ectopia of the lens and the pupil, small poorly dilating oval or slit-like pupils, and iridodonesis. However, because of variable expression, up to 50% of affected individuals may have ectopia lentis alone. The other reported features of ELP are listed in Table 1.1,2,3,4,5,6,7 The pathogenesis remains uncertain, but neuroectodermal, mesodermal, and mechanical defects have all been suggested.4,7
In ELP, as demonstrated in our case, the ectopic lens may cause a variety of problems. Initially, the management issue is one of improving and preserving visual acuity. The ectopic pupil makes the prescribing and fitting of spectacles and contact lenses difficult owing to the oblique visual axis. The lens often becomes cataractous at an early age and a hypermature lens may begin to leak lens protein, leading to uveitis and phacolytic glaucoma. In a case series of 10 patients with ELP, two were reported to suffer from uveitis, two from acute intermittent intraocular hypertensive crises, similar to our case, and seven had raised IOP.6 Eventually, the IOP may become impossible to control medically and it becomes necessary to remove surgically the dislocated cataractous lens.8
Smith et al9 reported the successful surgical management of uncontrolled phacolytic glaucoma caused by a lens in the vitreous in a patient with homocystinuria. However, they carried out a vitreo-lensectomy combined with a trabeculectomy. With vitreo-lensectomy alone, our patient's IOP became controlled with medical therapy within 24 h and has remained so postoperatively.
We propose therefore that in such cases of chronic, uncontrolled phacolytic glaucoma, combined trabeculectomy is not always required, thus eliminating the potential complications of drainage surgery.
References
Townes PL . Ectopia lentis et pupillae. Arch Ophthalmol 1976; 94: 1126–1128.
Luebbers JA, Goldberg MF, Herbst R et al. Iris transillumination and variable expression in ectopia lentis et pupillae. Am J Ophthalmol 1977; 83: 647–656.
Cross HE . Ectopia lentis et pupillae. Am J Ophthalmol 1979; 88(3): 381–384.
Goldberg MF . Clinical manifestations of ectopia lentis et pupillae in 16 patients. Ophthalmology 1988; 95: 1080–1087.
Colley A, Lloyd IC, Ridgway A, Donnai D . Ectopia lentis et pupillae: the genetic aspects and differential diagnosis. J Med Genet 1991; 28: 791–794.
Cruysberg JRM, Pinckers A . Ectopia lentis et pupillae syndrome in three generations. Br J Ophthalmol 1995; 79: 135–138.
Byles DB, Nischal KK, Cheng H . Ectopia lentis et pupillae—a hypothesis revisited. Ophthalmology 1998; 105: 1331–1336.
Nelson LB, Maumenee IH . Ectopia lentis. Surv Ophthalmol 1982; 27(3): 143–160.
Smith GT, Vakalis AN, Brittain GP, Casswell AG . Vitrectomy for phacolytic glaucoma in a patient with homocystinuria. Am J Ophthalmol 1999; 128(6): 762–763.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossiter, J., Morris, A., Etchells, D. et al. Vitrectomy for phacolytic glaucoma in a patient with ectopia lentis et pupillae. Eye 17, 243–244 (2003). https://doi.org/10.1038/sj.eye.6700302
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700302