Abstract
Purpose To investigate the effect on intraocular pressure (IOP) of intraoperative 5-fluorouracil (5-FU) application during primary trabeculectomy in a West African population.
Methods Retrospective case note search of operating theatre records for primary trabeculectomy between 1996 and 2000 in an eye hospital in Lagos, Nigeria. For statistical analysis, patients were divided into group that received intraoperative 5-FU (50 mg/ml for 5 min) and a control group that received no intraoperative antimetabolites. Patients with a follow-up of less than 6 months were excluded. For life-table analysis, only one eye from each patient was included to maintain independent analysis.
Results A total of 154 eyes of 101 patients were included in the study. Average follow-up was 17 ± 2.18 (95% confidence interval) months. No significant difference was found between the groups for age, sex, preoperative medication, and follow-ups. Comparison of survival curves by the log-rank test showed that the probability of maintaining an IOP of 20 mm Hg or less at 18 months was 76% in the 5-FU group and 79% in the controls (P= 0.55). However, the probability of maintaining an IOP 14 mmHg or less was significantly greater in the 5-FU group (64%) than in the controls (39%, P=0 .018). Visual acuity loss of more than two Snellen-chart lines was observed in six eyes (7.9%) of the 5-FU group and in four eyes (5.1%) of the control group and this difference was not significant (P=0.49, Fisher exact test). Complication rates were similar in each group.
Conclusions In this population, intraoperative 5-FU application during trabeculectomy appears to improve probability of maintaining an intraocular pressure of 14 mmHg or less with no additional deleterious effects on the eye.
Similar content being viewed by others
Introduction
Glaucoma is a major cause of blindness in West Africa.1 Data from epidemiological studies in North America suggest that people of West African descent have a higher prevalence of the disease, develop it at a younger age and are more likely to go blind because of glaucomatous optic atrophy.2,3,4,5,6 Treatment of glaucoma is problematic. Presentation is often late in the course of the disease.7,8 Most of the glaucoma medications are not available. If available, the cost of these medications is prohibitive. Moreover, reports of surgical outcomes for glaucoma from this region are few and limited by poor follow-up and inadequate statistical analyses.7,8,9,10,11,12,13 We have previously reported that the probability of achieving an IOP less than 22 and 16 mmHg 5 years after primary nonaugmented trabeculectomy in Nigeria was 71 and 46%, respectively.7
A randomised prospective trial in Ghana, West Africa demonstrated that intraoperative 5-fluorouracil (5-FU) application during trabeculectomy results in lower intraocular pressures (IOP) in the short term.8 The mean follow-up was 10 months in this study. Longer-term data of this beneficial effect of 5-FU are lacking.
We looked at our primary trabeculectomy outcomes since 1996 to see if intraoperative 5-FU application results in a lower IOP when compared to nonaugmented primary trabeculectomy.
Methods
The study resulted from a change in clinical practice in the Maja Eye Hospital, Lagos, Nigeria. Visiting ophthalmologists from the UK perform glaucoma surgery in this centre. Since 1996, one of us (NA) has routinely performed 5-FU-augmented primary trabeculectomies. Other surgeons gradually adopted this practice. This gave us an opportunity to retrospectively examine whether intraoperative 5-FU application during trabeculectomy had any effect on the postoperative IOPs in the short to medium term.
Consecutive patients undergoing primary trabeculectomy between January 1996 and May 2000 were included in the study. Eyes with less than 6 months follow-up were excluded. Two surgeons (NA and VKD) did most of the trabeculectomies (81%). Local doctors saw patients on postoperative visits
Data were collected on standardised forms and included patient details, ocular diagnosis, coexisting ocular pathology, previous ocular surgery, severity of glaucoma damage as adjudged by disc cupping and visual field loss, preoperative IOP, visual acuity, and medications. Operative details and intraoperative complications were noted. The following were recorded for each postoperative visit: visual acuity, IOP, complications, and medications. Subsequent surgery—glaucoma and cataract—was also noted.
Major outcome measures were an IOP reduction of more than 30% from preoperative levels, a permanent decrease in visual acuity of two or less Snellen-chart lines from preoperative levels and:
-
1
IOP 20 mm Hg or less with or without medication.
-
2
IOP less than 14 mmHg or less with or without medication.
Some patients underwent needle revision of filtering blebs with subconjunctival antimetabolite injection for raised IOP because of bleb scarring. These eyes were deemed to have failed. Eyes were censored when they underwent extracapsular cataract extraction because of the unfavourable effect of these procedures on bleb function.
Success rates were summarised by Actuarial Life-table Analyses method. If a patient had bilateral surgery, only the first eye that underwent surgery was analysed by this method, to maintain independent observations.
Comparison of the time to failure of trabeculectomy by the two criteria was done in a univariate fashion, by Kaplan–Meier survival curve analyses and the log-rank test.14
All patients underwent a Cairns-type trabeculectomy with slight modifications in technique.15 A fornix-based conjunctival flap was dissected. 5-FU (50 mg/ml) soaked on surgical sponge was applied between the dissected conjunctiva and sclera for 5 min. The area was then washed with 20 ml of balanced salt solution. This was followed by dissection of a triangular or rectangular scleral flap. The exact dimensions of the scleral flap varied according to surgeon. After the excision of a block of corneo-scleral tissue, a peripheral iridectomy was done and the scleral flap was closed with one to five 10/0 nylon sutures. The conjunctival flap was closed with 10/0 nylon or 8/0 polyglactin sutures. Subconjunctival bethamethasone 1% and an antibiotic were given postoperatively. Patients used a topical steroid–antibiotic combination for at least 4 weeks postoperatively.
Results
A total of 101 patients and 154 eyes were included in the study. No significant difference in age, sex distribution, preoperative IOP, and follow-up period was found between the 5-FU and the control group (Table 1). As they had less than 6 months follow-up 25 eyes (14%) of 18 patients (15%) were excluded.
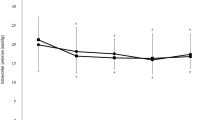
Mean IOP after surgery for the two groups are shown in Table 2. The multiple analysis of variance test (MANOVA, between-group effect) did not show a statistical difference in the pressures between the two groups at any measured interval (Table 2, P>0.05).
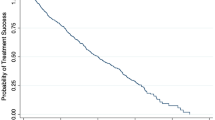
Figures 1 and 2 show the Kaplan–Meier survival curves for probability of maintaining IOP of 20 mmHg or less and an IOP of 14 mmHg or less after trabeculectomy. If an IOP of 20 mmHg or less was defined as success, 76% of the 5-FU group and 79% of the control group were successful at 18 months. Comparison of survival curves did not show any significant difference by the log-rank test (P=0.55). When success was defined as an IOP of 14 mmHg, the probability of success was 64% for the 5-FU group and 39% for the control group at 18 months. This difference was significant by the log-rank test (P=0 .018).
Four eyes (5.1%) of the control group and six eyes (8.9%) lost more than two lines of Snellen-chart visual acuity and this difference was not statistically significant (P=0.49, Fisher exact test). In five eyes, three from the control group and two from the 5-FU group, the cause of visual loss was felt to be progression of the disease to involve central fixation. Other causes for reduction in visual acuity were central retinal vein occlusion in two eyes, diabetic macular oedema and cataract in one eye each from the 5-FU group and branch retinal vein occlusion in one eye from the control group. Snellen visual acuity change for all eyes after surgery is shown in Figure 3.
Medications to lower intraocular pressure were used in 12 eyes (15.7%) of the 5-FU group and 14 eyes (17.9%) of the control group. This difference was not statistically significant (P=0.9, Yates corrected χ2-test). In all these eyes, IOPs were higher than 18 mmHg after surgery despite addition of glaucoma medications.
A total of 18 eyes (11.6%) – eight from the control group and 10 from the 5-FU group—underwent external revision of the filtering bleb with additional subconjunctival 5-FU injections (5 mg). Only four eyes achieved an IOP drop of at least 5 mmHg 3 months or more after the needle revisions. Postneedling data were incomplete in four cases. Five eyes, all from the 5-FU group have subsequently undergone needle revision with subconjunctival injection of mitomycin C (MMC) 0.02 mg. All except one of these eyes had previous needle-revision with subconjunctival 5-FU injections. IOP data from these cases are still incomplete. Two eyes have had repeat glaucoma surgery—trabeculectomy with MMC application.
Complications are shown in Table 3. There were few serious complications in both groups. One eye from the control group showed a delayed leak through a cystic area in the conjunctival bleb, 10 months after trabeculectomy. This was treated by excision of the cystic area and advancement of the conjunctival flap. No case of endophthalmitis and only one case of blebitis that responded to topical and systemic antibiotics was observed.
A total of 14 eyes (9%)—five from the 5 FU and nine from the control group—underwent extracapsular cataract extraction during the follow-up period.
Discussion
It is difficult to conduct a long-term, prospective, randomised control trial in this part of the world. Intraoperative 5-FU application during trabeculectomy is safe, with no additional deleterious side effects. The statistical probability of maintaining an IOP of 14 mmHg or less is significantly higher after a 5-FU-augmented trabeculectomy in this population group. This study was nonrandomised and selection bias, if present, would favour the control group as patients with more severe disease would be more likely to receive 5-FU. Despite that there was a statistically significant difference in favour of the 5-FU group with regard to the proportion of patients achieving IOPs 14 mmHg or less. A recent review article has emphasised the difficulties of glaucoma management in West Africa.16 There are few studies in literature regarding the long-term outcomes of glaucoma surgery in West Africa.8,10,11,12,13. Poor patient follow-up or failure to indicate duration of follow-up is a serious limiting factor in most of these studies. We have previously reported that the probability of achieving an IOP less than 22 and 16 mmHg 5 years after primary trabeculectomy in Nigeria is 71 and 46%, respectively.7 A literature search using Medline revealed only one previous publication comparing standard primary trabeculectomy with intraoperative 5-FU application from West Africa by Egbert et al.9 The follow-up in this study was less than 1 year and it showed that eyes receiving intraoperative 5-FU had significantly lower IOPs. The mean final IOP in the control group was 24.5 and 17.3 mmHg in the 5-FU group. This compares with an average mean IOP of 14 mmHg at 1 year in both the control and 5-FU groups in this study.
Of Egberts' study patients 10% had previous intraocular surgery, while we specifically excluded these patients. Most patients included in our study lived in the largest city in Nigeria where people are more affluent, and public transport better than in rural Ghana. A significant proportion (15%) of our patients with uncomplicated and initially successful surgery had follow-ups less than 6 months and were excluded from the study. The effect of this on the outcomes of our study is difficult to predict.
A recent randomised trial from East Africa shows little difference in the IOPs between the control group and the group receiving intraoperative 5-FU during trabeculectomy. By 2 years, however, the control group was less likely to maintain successful IOP control (less than 22 mmHg) and more likely to require additional IOP lowering measures.17 The reason for choosing IOPs less than 20 and 14 mmHg was to make a comparison with the results reported by Egbert et al—the only randomised prospective trial looking into the effect of 5-FU on trabeculectomy from West Africa.9 The Advanced Glaucoma Intervention Study18 has shown that in advanced glaucoma, irrespective of race, patients with an IOP consistently less than 18 mmHg had the least chance of field progression.18
In advanced glaucoma, it is difficult to predict progression by visual fields. In this study 70% of eyes had advanced glaucomatous optic disc cupping or visual field loss affecting central vision. Equipment for testing visual fields was rather rudimentary and done patchily at best, hence our decision to concentrate on visual acuity. The majority of patients maintained their visual acuity with no difference between the groups.
Trabeculectomy outcomes are generally believed to be worse in patients of African origin. This is because of the more exuberant wound healing observed in these patients.19 Till recently there was very little evidence to support this clinical observation. The Advanced Glaucoma Intervention Study (AGIS Report 9)18,20 has demonstrated that after failure of medical therapy, the chances of failure (IOP more than 18 mmHg and diminution of visual acuity) were slightly higher in black patients as compared to white patients if trabeculectomy was the first intervention. Black patients regardless of treatment group were also on a higher number of medications in this long-term prospective study.
Singh et al,21 in a prospective randomised trial comparing intraoperative 5-FU 50 mg/ml for 5 min and MMC 0.5 mg/ml applied intraoperatively for 3.5 min in patients with glaucoma undergoing trabeculectomy in Ghana, found that 93% of the patients in the MMC group and 73% in the 5-FU group had achieved an IOP of less than 21 mmHg after an average follow-up of 10 months. However, the proportion of eyes with an IOP less than 15 mmHg was not significantly different between the two groups. There was no significant difference between the complication rates of the two groups.21,22 Other reports from Africa suggest higher complication rates, especially of hypotony and endophthalmitis, with MMC application during trabeculectomy.23,24
Despite being retrospective, we believe that this study contributes valuable information regarding outcomes of primary and 5-FU-augmented trabeculectomy.
References
Schwab L, Steinkuller PG . Surgical treatment of open angle glaucoma is preferable to medical management in Africa. Soc Sci Med 1983; 17: 1723–1727.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. Arch Ophthalmol 1991; 109: 1090–1095.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt JC et al. Racial differences in the cause-specific prevelance of blindness in east Baltimore. N Engl J Med 1991; 325: 1412–1417.
Leske MC, Connell AM, Wu SY, Hyman LG, Schachat AP . The Barbados Eye Study. Risk factors for open-angle glaucoma. Arch Ophthalmol 1995; 113: 918–924.
The Advanced Glaucoma Intervention Study (AGIS): 3. Baseline characteristics of black and white patients. Ophthalmology 1998; 105: 1137–1145.
The Glaucoma Laser Trial (GLT): 5. Subgroup differences at enrolment. Glaucoma Laser Trial Research Group. Ophthalmic Surg 1993; 24: 232–240.
Anand N, Mielke C, Dawda VK . Trabulectomy outcomes in advanced glaucoma in Nigeria. Eye 2001; 15: 274–278.
Verrey JD, Foster A, Wormald R, Akuamoa C . Chronic glaucoma in Northern Ghana—A retrospective study of 397 patients. Eye 1990; 4: 115–120.
Egbert PR, William AS, Singh K . A prospective trial of intraoperative fluorouracil during trabeculectomy in a black population. Am J Ophthalmol 1993; 116: 612–616.
Chatterjee S, Ansari MW . Microsurgical trabeculectomy in Ghana. Br J Ophthalmol 1972; 56: 783–787.
Kietzman B . Glaucoma surgery in Nigerian eyes: a five-year study. Ophthalmic Surg 1976; 7: 52–58.
Sandford-Smith JH . The surgical treatment of open-angle glaucoma in Nigerians. Br J Ophthalmol 1978; 62: 283–286.
Thommy CP, Bhar IS . Trabeculectomy in Nigerian patients with open-angle glaucoma. Br J Ophthalmol 1979; 63: 636–642.
Glantz SA . How to analyse survival data. In: Primer of Biostatistics, 4th Ed. McGraw-Hill: New York, 1997; pp 373–402.
Cairns JE . Trabeculectomy: preliminary report of a new technique. Am J Ophthalmol 1968; 66: 673–679.
Budenz DL, Singh K . Glaucoma care in West Africa. J Glaucoma 2001; 10: 348–353.
Yorston D, Khaw PT . A randomised trial of the effect of intraoperative 5-FU on the outcome of trabeculectomy in East Africa. Br J Ophthalmol 2001; 85(9): 1028–1030.
The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Broadway D, Grierson I, Hitchings R . Racial differences in the results of glaucoma filtration surgery: are racial differences in the conjunctival cell profile important? Br J Ophthalmol 1994; 78: 466–475.
The Advanced Glaucoma Intervention Study (AGIS): 9. Comparison of glaucoma outcomes in black and white patients within treatment groups. Am J Ophthalmol 2001; 132: 311–320.
Singh K, Egbert PR, Byrd S, Budenz DL, Williams AS, Decker JH et al. Trabeculectomy with intraoperative 5-fluorouracil vs mitomycin C. Am J Ophthalmol 1997; 123: 48–53.
Singh K, Byrd S, Egbert PR, Budenz D . Risk of hypotony after primary trabeculectomy with antifibrotic agents in a black west African population. J Glaucoma 1998; 7: 82–85.
Mwanza JC, Kabasele PM . Trabeculectomy with and without mitomycin-C in a black African population. Eur J Ophthalmol 2001; 11: 261–263.
Mermoud A, Salmon JF, Murray AND . Trabeculectomy with mitomycin C for refractory glaucoma in blacks. Am J Ophthalmol 1993; 116: 72–78.
Author information
Authors and Affiliations
Corresponding author
Additional information
Institution where work done: Maja Hospital, 33 Moloney Street, Lagos, Nigeria
This paper was presented as a poster at The Royal Congress of Ophthalmologists, Annual Congress, Manchester, 2002
Rights and permissions
About this article
Cite this article
Mielke, C., Dawda, V. & Anand, N. Intraoperative 5-fluorouracil application during primary trabeculectomy in Nigeria: a comparative study. Eye 17, 829–834 (2003). https://doi.org/10.1038/sj.eye.6700492
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700492