Abstract
Purpose
To evaluate the pattern of ocular and visual complications of head injury.
Method
A prospective study of 225 head-injured patients managed at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. For the purpose of extracting vaisual complications, a Neurosurgeon and an Ophthalmologist examined each patient and appropriate investigations were carried out. Patients with ocular morbidity were analysed for age, sex, cause of injury, admission Glasgow coma score, and associated injuries in addition to findings at ophthalmic and neurosurgical evaluations.
Results
Two major types of ocular and visual complications were observed in 57 (25.3%) of 225 head-injured patients studied. Soft-tissue injury to the globe and adnexae included periorbital ecchymosis, subconjuctival haemorrhage, lid laceration, or rarely globe rupture in 29 patients. Neuro-ophthalmic ocular cranial nerve palsies occurred in 28 patients, while orbital fracture was encountered in two patients. Ocular injuries were multiple in 60% of cases. The patients, comprising 37 male and 20 female subjects, were aged 9 months to 57 years (mean=28 years). Traffic accident was the leading cause of head injuries (84.2%), while fall from height (7%), assault (7%), and gunshot (1.8%) were miscellaneous causes.
Conclusion
Injury to the globe and adnexae and ocular cranial nerve palsies constitute the most common oculovisual complications following head injury in our centre.
Similar content being viewed by others
Introduction
Ocular trauma is the cause of blindness in more than half a million people worldwide and of partial loss of sight in many more, and it is often the leading cause of unilateral loss of vision particularly in developing countries. 1 Head injuries cause the hospitalization of 200–300 persons per 100?000 populations per year,2 and about 25% of these are associated with ocular and visual defects. The role of ocular injuries secondary to head trauma in the causation of blindness has become a subject of immense importance.3
The manifestations of head injury and its numerous other systemic complications are so compelling that damage to the visual system is most likely to be ignored. Often times, when the eye is examined as part of neurological assessment of a patient with head injury, the purpose is mainly to gauge the severity of the head injury itself.3, 4 Since the mechanisms underlining ocular manifestations of head trauma are not fully understood, many hypotheses have been advanced to explain these defects. However, most of these hypotheses have remained untested and unproven.5 With respect to soft-tissue injuries to the globe and adnexae in the anterior segment of the eye, one hypothesis suggested that energy is transferred to these structures from the sturdy frontal bones to the orbit and from the lateral orbital margin to contiguous facial structures during the impact following head injury.6 Disorders of eye movement are thought to result from direct trauma to orbital contents, cranial nerves, and other brain areas.7
In spite of the significance of problems associated with ocular manifestations of head injury, only scanty systematic reviews of the whole spectrum are available in the literature. The aim of this study was to evaluate the pattern and clinical profile of ocular and visual complications in patients hospitalized and managed for head injury at our centre.
Materials and methods
The study comprised a prospective analysis of 225 patients diagnosed as having head injury by the Neurosurgical team on the basis of history, neurological findings, and Glasgow coma scale score8 at admission. They were hospitalized for varying periods between January 2001 and June 2003 at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. All patients were reviewed and followed up by the Ophthalmologist for signs and symptoms of ocular morbidity, which were subsequently analysed. Diagnostic investigations carried out included skull and spine roentgenograms, computed tomographic brain scanning when indicated, gonioscopy, perimetry, diplopia charting, and measurement of intraocular pressure. Visual acuity (VA) in adults was assessed using the Snellen's chart but in children crudely by grading visual fixation and tracking to familiar objects. Findings were transferred into a questionnaire format, which included patients' sociodemographic data, mode of head trauma, and findings at neurological and ophthalmic evaluations.
Ocular and visual complications were grouped into three main classes of abnormalities of the visual system: soft-tissue injuries to the globe and adnexae, neuro-ophthalmic abnormalities, and injuries to the bony orbit and eye. In each patient, the predominant ocular and visual complications were graded according to an arbitrary severity scale into mild, moderate, and severe forms. Mild (Grade 1) ocular complication is restricted to soft-tissue injury to the eye and adnexae without a ruptured globe. The moderate (Grade 2) type is predominantly neuro-ophthalmic with or without soft-tissue injury, while a severe (Grade 3) complication involves rupture of the globe, fractures of the orbit with or without other soft-tissue, and neuro-ophthalmic injuries. Graded ocular and visual complications were then related to age, sex, admission Glasgow coma score (GCS), and mode of injury.
Apart from suture of lacerations, patients were managed according to their respective diagnoses by the neurosurgical and ophthalmologic units. Those who presented with multiple organ involvement were referred to the appropriate specialties in the same hospital.
Results
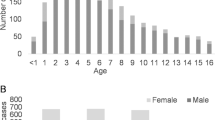
Ocular and visual complications occurred in 57 of 225 (25. 3%) head-injured individuals managed during the period under consideration. They were 37 (64.9%) male and 20 (35.1%) female subjects giving an approximate male to female ratio of 2?:1. At presentation, the youngest and oldest patients were 9 months and 57 years old, respectively, the mean age being 28 years. Ophthalmic complications were least during childhood, peaked at the third decade of life, and thereafter declined (Figure 1). In 19 patients (33.3%), head and ocular injuries were associated with injuries to other organs such as the chest, abdomen, and long bones. Multiple ocular injuries involving both anterior and posterior segments of the eye were encountered in 60% of the patients. The right, left, and both eyes combined were injured in an approximate ratio of 1?:?1?:?4 respectively.
The causes of head injury are itemized in Table 1 and shown in Figure 2. Traffic accidents were the most common cause of ocular disorder (84.2%, 48/57). Fall from height and assault accounted for head and ocular injuries in four patients each (7%), while gunshot injury to the head was responsible in one patient (1.8%) (Table 1). Of the traffic-related accidents, passengers were most frequently affected (75.0%) than pedestrians (19.0%) and cyclists (6.0%) (Figure 2). All the patients who fell from heights (four) and 66.7% of those involved in pedestrian accidents were children aged 15 years or below (Table 2), while all victims of assault (four) and gunshot injury (one) were males (Table 2).
Table 3 shows the ocular and visual complications of head injury observed in 57 cases. They include soft-tissue injuries to the globe and adnexae in 29 patients, neuro-ophthalmic abnormalities in 28 patients, and fracture of the orbit with rupture of the eye in two patients. The most frequent soft-tissue injuries were periorbital ecchyimosis (17 patients), chemosis (20 patients), subconjuctival haemorrhage (21 patients), lid laceration (10 patients), corneoscleral laceration (five patients), retinal haemorrhage (two patients), and commotio retinae (three patients).
The most frequently encountered neuro-ophthalmic manifestation was ocular motor nerve palsy (Table 3), causing motility disorders followed by optic nerve damage responsible for visual loss. Abducens' palsy occurring in eight patients was the most common ocular motor nerve palsy, followed by oculomotor and trochlear nerve palsies, which were encountered in six patients each. Four patients complained of double vision, shortly after discharge from the hospital. Diplopia was secondary to internuclear ophthalmoplegia (one patient), conjugate gaze palsy (one patient), and decompensated binocular skills (two patients). Other commonly affected cranial nerves in this series were the facial (six patients) and auditory (two patients) nerves.
Traumatic damage of the optic nerve produced visual loss in 12 patients (Table 3) ranging from homonymous field loss (two patients) and visual impairment (six) to blindness in one (three) or both eyes (one). Traumatic optic neuropathy was diagnosed in one of the patients with visual impairment. It manifested with loss of best-corrected visual acuity in one eye accompanied by the presence of an ipsilateral afferent pupillary defect (Marcus Gunn pupil). In addition, blindness occurring in a patient who was blind in both eyes was cortical in origin because the fundus was normal and the pupillary responses were intact. Miscellaneous neuro-ophthalmic complications observed were other pupillary abnormalities (12), partial or complete ptosis (10), and lagophthalmos (one).
The globe was ruptured from road traffic accident in two drivers who attempted jumping out of their vehicles during the impact. In both patients, there was concomitant communited fracture of the orbit (Table 3). Both patients died from associated multiple injuries in spite of prompt surgical and nonsurgical interventions. The overall frequency of ocular and visual complications of head injury was age related. Of the 57 patients, 10 (17%) were 15 years old or younger (Table 3), while 75.5% and 7% were aged 16–45 and 46–60 years, respectively (Table 4). Male subjects predominated over female subjects in all age groups but this dominance was more pronounced among patients whose injuries were secondary to fall, assault, and gunshot (Table 2). It was equally more pronounced among patients aged 45 years and above, and in patients who had severe complications.
When the severity of ocular injury was related to Glasgow Coma Score (GCS) on admission (Table 4), nearly half (21) of the ocular and visual injuries occurred in mildly head-injured patients with GCS of 13–15. Severe ocular injury was associated with severe head injury whose GCS was less than or equal to 8 on admission.
While soft-tissue (or mild) injury was the predominant form among pedestrians, the moderate neuro-ophthalmic type was more common among cyclists (Table 4).
Discussion
Eye injuries remain the most common cause of monocular blindness, a life-long disability, and when the outcome is less serious than blindness extensive medical care, including surgery, hospitalization, and repeated treatments over long periods may be required.9 In spite of this, majority of the past reviews on this subject have focused on specific aspects of the visual anatomy, such as the ocular cranial nerves, optic nerves, or the posterior visual pathways,5, 7, 10, 11, 12 rather than a complete overview of the manner in which head injury affects the visual system.2, 3, 13, 14 This study has added to the latter list and has given credibility to a few previous findings.
Although the true incidence of ocular injuries resulting from head trauma is not known in many underdeveloped countries such as Nigeria, the high frequency of occurrence (25.3%) obtained in this study corroborates well with a frequency of 25% reported following automobile accidents in a western series15 and 28% reported for head-injured children in western Nigeria,14 but understandably much below the 40% reported for adults and children following head and facial injuries in a centre based in the eastern part of Nigeria.13
It is not surprising that traffic accidents were responsible for the greater proportion of head injuries associated with ocular manifestations. In many series worldwide, traffic accident constitutes the leading cause of head injury4, 13, 14 except in a few where fall from height is the most common.3 In our setting, motorized transportation has been on the rise in recent years and this is not without the attendant risk of increased auto accidents. This is worst in those parts of the world like ours, where traffic regulations and speed limits are not strictly observed and unlicensed careless driving is treated with levity.
The lids and conjunctiva in the anterior segment of the eye were more commonly involved in head injuries than the posterior segment, ocular cranial nerves, or the bony orbit. Injuries to this segment result from direct impact on the rigid frontal bones and orbital margins, producing periorbital ecchymosis, lid laceration, subconjuctival haemorrhage, and chemosis.
Of the neuro-ophthalmic complications, traumatic ocular motor abnormality was the most frequent, the abducens being the most commonly affected cranial nerve followed by oculomotor and trochlear nerves. The incidence of abducens nerve palsy in severe head injuries has been reported as 27%. The mechanism of its palsy, secondary to severe head injuries, has been attributed to avulsion or contusion of the nerve at the base of the posterior clinoid process, where it lies beneath the rigid petrospheniod (Gruber's) ligament, medial to the sensory root of the fifth nerve at the apex of the temporal bone.11 It is also the most commonly damaged cranial nerve when a basilar fracture crosses the petrous ridge and a clear relationship can usually be established with facial paralysis and deafness.11 This makes the seventh and eighth cranial nerve damage a common association with head injuries associated with ocular manifestations as observed in this series. Abducens palsy could also derive from sufficient middle cranial fossa haemorrhage causing compression and pressure paralysis on one or both sides.11
Visual loss resulting from globe rupture, traumatic optic nerve damage, or occipital cortical injury associated with head injury in this series should be regarded as the most significant disability. Trauma-induced injury to the optic nerve can occur anywhere along the nerve's intraorbital to intracranial length. Considering traumatic neuropathy identified in one patient (1.8%) as a separate entity, its pathogenesis was thought to be largely a matter of speculation;10 however, autopsy and pathological findings5 have confirmed the presence of dural haemorrhage, interstitial nerve haemorrhage, shearing lesions, as well as localized ischaemia and oedema, which are considered as secondary events to initiate neuropathy. Such injuries are ordinarily self-limiting as it was in our patient, with improvements occurring in 3–4 days.10 However, when they do persist, corticosteroid therapy or optic nerve decompression has been advocated.16 Currently, endoscopic optic nerve decompression by an intranasal or trans-ethmoidal or trans-sphenoidal approach is gaining popular support. Cortical blindness occurring in one patient is not a common finding in the head-injured patients, monocular blindness being a more common feature. Partial or total blindness is apt to hamper full recovery after survivors have successfully come out of coma and have achieved ambulation. It is thus important to identify such patients early by integrating the services of a neurosurgeon and an ophthalmologist in order to foster prompt intervention and visual rehabilitation.
Internuclear ophthalmoplegia (INO) was detected during a follow-up visit in a 35-year old man who suffered closed head injury due to an automobile accident. There was no previous history of ophthalmic, medical, or neurological disorder (eg multiple sclerosis). On attempted right lateral gaze, the left eye failed to adduct across the midline and there was nystagmus of the abducting right eye. Attempted convergence and vertical movements of the eyes, visual acuity (6/6), and pupillary response to light were normal. This suggested that he had the posterior variety of INO with a lesion located to the pontomesencephalic junction in the midline of the medial longitudinal fasciculus (MLF) caudal to the oculomotor nucleus.17, 18 Bilateral INO is pathognomonic of multiple sclerosis19 but unilateral INO though rare has been described in association with vascular disease, central nervous system infections, and drugs. It is, however, a rare complication of head injury.18 Apart from INO, double vision (diplopia) could be secondary to strabismus, gaze palsy, and decompensated binocular skills in patients with brain injury.
Conclusion
Injury to the globe and adnexae and ocular cranial nerve palsies constitute the most common oculovisual complications following head injury in our centre.
References
WHO Geneva. Strategies for the Prevention of Blindness in National programmes. A Primary Health Care Approach, 2nd edn. WHO Library Cataloguing: England, 1997, pp 74–76.
Baker RS, Epstein AD . Ocular motor abnormalities from head trauma. Survey Ophthalmol 1991; 35(4): 245–267.
Chaudhuri Z, Pandey PK, Gupta R, Chauhan D . Profile of ocular morbidity associated with head injury. AIOC Proceedings. MISCELLANEOUS 2002; p: 609.
Burch FE . Ocular evidence of head trauma. Wisc Med J 1942; 41: 1092–1097.
Crompton MR . Visual lesions in closed head injury. Brain 1970; 93: 785–792.
Duke Elder S, Wybar KC . The Anatomy of the Visual System. Eye and Sport Medicine, Vol. 2. CV Mosby: St Louis, 1961, pp 559–567.
Cohen M, Groswasser Z, Barchadski R, Appel A . Convergence insufficiency in brain-injured patients. Brain Injury 1989; 3(2): 187–191.
Teasdale G, Jennett B . Assessment of coma and impared consciousness: a practical scale. Lancet 1974; 2: 81–83.
Karlson TA, Klein BEK . The Incidence of acute hospital-treated eye injuries. Arch Ophthalmol 1986; 104: 1473–1476.
Ramsay JH . Optic nerve injury in the fracture of the canal. Br J Ophthalmol 1979; 63: 607–610.
Schneider RC, Johnson FD . Bilateral traumatic abducens palsy: a mechanism of injury suggested by the study of associated cervical spine fractures. J Neurosurg 1971; 34: 33–37.
Rush JA, Younge BR . Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol 1981; 99: 76–79.
Magulike NO . Ophthalmic manifestation of head and facial injuries. Nigerian J Surg Sci 2000; 10(1): 1–3.
Shokunbi MT, Agbeja AM . Ocular complications of head injury in children. Child's Nerv Syst 1991; 7: 147–149.
Fite JD . Neuro-ophthalmological syndrome in automobile accidents. South Med J 1970; 63: 567–570.
Waga S, Kubo Y, Sakakura M . Transfrontal intradural microsurgical decompression for traumatic optic nerve injury. Acta Neurochir 1998; 91: 42–46.
Hsu HC, Chen HJ, Lu K, Liang CL . Reversible bilateral imnternuclear ophthalmoplegia following head injury. Acta Ophthalmol Scand 2001; 79: 57–59.
Cogan DG . Inter-nuclear ophthalmoplegia, typical and atypical. Arch Ophthalmol 1970; 84: 583–589.
Baker RS . Internuclear ophthalmoplegia following head injury. Case report. J Neurosurg 1979; 51: 552–555.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Odebode, T., Ademola-Popoola, D., Ojo, T. et al. Ocular and visual complications of head injury. Eye 19, 561–566 (2005). https://doi.org/10.1038/sj.eye.6701566
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701566
Keywords
This article is cited by
-
Ocular injuries associated with motor vehicle accidents: long term effects on quality of life
International Ophthalmology (2024)
-
Potential Mechanisms of Acute Standing Balance Deficits After Concussions and Subconcussive Head Impacts: A Review
Annals of Biomedical Engineering (2021)
-
A comparison of pediatric ocular injuries based on intention in patients admitted with trauma
BMC Ophthalmology (2019)
-
Ophthalmic complications among cases of head trauma in north-eastern Iran
International Ophthalmology (2014)
-
Ocular manifestations of head injury and incidence of post-traumatic ocular motor nerve involvement in cases of head injury: a clinical review
International Ophthalmology (2014)