Abstract
Purpose
To describe and examine the observation that eccentric eye positions may develop under certain general anaesthetic conditions and negatively impact upon operating conditions during ocular surgery.
Methods
A case series description with historical review followed by a 2-week prospective observational survey examining the general anaesthetic techniques utilized during ocular surgery and the associated development of an eccentric eye position.
Results
A total of 52 cases were studied, of which four developed eccentric eye positions. 50% of patients received effective muscle relaxation. Without muscle relaxants, the incidence of eccentric eye positioning was 18%.
Conclusions
Eccentric ocular positions are likely to occur in light planes of general anaesthesia. In the case of ocular surgery, this phenomenon may create surgical difficulty and increase the risk of complication and patient morbidity. Arguments for the planned use of balanced general anaesthesia with non-depolarizing muscle relaxants are presented.
Similar content being viewed by others
Introduction
High-volume local anaesthetic (LA) day-case surgery is the preferred option for many ocular procedures, not least phacoemulsification. Yet general anaesthesia (GA) remains the anaesthetic of choice for selected procedures and patient groups in order to ensure acceptable operating conditions. For example, all ocular procedures performed on children, squint surgery, intraocular surgery in young or anxious patients, and those with disorders such as Parkinson's disease, learning difficulty, or dementia.
We wish to raise awareness to a phenomenon occurring under certain GA conditions that has significant implications for ocular surgery. When occurring, it results in an unsatisfactory surgical field, creates significant intraoperative difficulty and increases the risk of complications and therefore patient morbidity. To our knowledge, it has not been previously reported in this context.
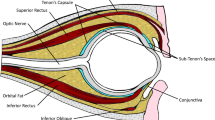
This report is based on observations made on six patients undergoing ocular surgery under GA. In each case, the procedure undertaken was found to be unexpectedly difficult owing to the development of a fixed, eccentrically deviated eye, positioned as if in extreme upward gaze. This group included four patients undergoing cataract surgery and two having squint surgery. It is important to emphasize that the eccentric position appeared to develop because of an intense and sustained contraction of the superior rectus muscle over its opposites. In the two patients having squint surgery, this meant that the eyes could not be manipulated satisfactorily in order to permit surgery to be undertaken. Following discussions with the anaesthetists, non-depolarizing muscle relaxants (NDMR) were administered which resolved the difficulty, allowing surgery to begin.
Arguably, the occurrence of this phenomenon during cataract surgery is of more consequence as complications and patient morbidity may ensue. In two of the four patients having cataract surgery, loss of the capsulorhexis superiorly occurred where the development of the eccentric position created difficult off-axis views and hindered the manoeuvrability of instruments within the eye. Fortunately, in each case, surgery was completed cautiously without further complication. However, an incomplete capsulorhexis undoubtedly increases significantly the risk of posterior capsule rupture and its associated sequelae.1
Of concern, in all six cases the attending surgical and anaesthetic teams were uncertain of the cause of the ocular deviation. A retrospective review of the anaesthetic charts revealed that all six patients had undergone GA with spontaneous respiration techniques without effective NDMR. It was considered that the explanation for the observed ocular deviation may lie with the anaesthetic conditions and that further investigation was warranted.
An electronic literature search yielded no citations describing this phenomenon in the context of causing difficulties in ocular surgery. Furthermore, no description of this problem was found in two recent anaesthetic textbooks dedicated to ophthalmic surgery.2, 3 However, it is widely known that eye movements occur during induction of anaesthesia and these have been used to help evaluate the depth of anaesthesia.
It was John Snow4 in 1848 who first developed the concept of anaesthetic depth, and notably first observed how ‘Usually the eyes become inclined upwards…’ at the point of sufficient anaesthetic depth. Guedel5 further refined the concept of anaesthetic depth and in 1937 published his classic description of the clinical stages of anaesthesia. He divided GA into four stages based on observations on how certain key physiological responses changed with increasing depth of anaesthesia. Stages 1 and 2 relate to the induction of anaesthesia. The third stage is the point at which mental control is lost and there is full rhythmic respiration. Guedel termed this stage ‘surgical anaesthesia’ and further divided it into four different planes. Plane 1 is characterized by slight somatic relaxation and notably, active extraocular muscles, usually, the author found, in the form of a fixed eccentric eye position. Significantly, in deeper planes of anaesthesia, the extraocular muscles became flaccid.
However, Snow's and Guedel's observations were made on patients anaesthetized with ether and chloroform, so it is not clear how relevant they are to modern GA. In order to explore this, we choose to perform an observational survey to determine current practice for GA in ocular surgery and to estimate the incidence of eccentric eye position development.
Methods
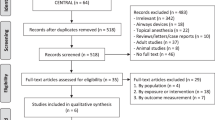
A 2-week prospective observational study was performed examining the anaesthetic techniques utilized for ocular surgery at two large ophthalmic units in the south of England. A questionnaire was completed by the anaesthetist for each case. Data collected included grade of anaesthetist, choice of ventilation, or spontaneous respiration, the anaesthetic agents used, the use and type of muscle relaxant, the presence of any significant ocular deviation, and any measures taken to address it, such as the deepening of anaesthesia or the administration of muscle relaxant.
Results
A total of 52 procedures were surveyed over the 2-week period. Of these, 56% (29) were anaesthetized by a consultant, 40% (21) by a staff grade, and 4% (2) by a specialist registrar (Table 1).
Overall 59% (31) of patients were ventilated of which 74% (23) had NDMR. 42% (22) had surgery performed under spontaneous respiration GA of which 14% (3) had muscle relaxant to assist intubation. One patient received total intravenous anaesthesia. Atracurium was the NDMR of choice in 29% (15) of the surveyed patients and vecuronium in 21% (11) patients. In all, 50% of surveyed patients received no planned NDMR.
Significant ocular deviation was seen in 8% (4) patients. Three of these four were ventilated, with one receiving total intravenous anaesthesia (TIVA). None had received NDMR (Figure 1). Measures taken to address the deviation included deepening of the anaesthesia in one case and the administration of NDMR in two. The incidence of this phenomenon in those patients not receiving NDMR was 18%.
Discussion
Clearly, an essential component of anaesthesia is that the patient is unaware of the surgical intervention. In the case of ocular surgery, both intraocular and extraocular, a further important requirement should be that the extraocular muscles are fully relaxed in order to allow a satisfactory surgical field. The survey presented confirms the premise that, in the absence of NDMR, eccentric ocular positions may develop under certain anaesthetic conditions. The incidence approached 20% in those patients not receiving NDMR.
We propose that, even with modern GA, this phenomenon is likely to occur in light planes of anaesthesia as first described by Snow. This supposition is supported by the finding that deepening of anaesthesia was used in one case to resolve the problem. This method of dealing with the problem will be discussed; however, it is important to note that, currently, there are no readily available, adequate monitors of the depth of anaesthesia.6
In a study that supports our findings and arguments, Power et al6 examined the depth of anaesthesia achieved by the administration of sevoflurane through induction by comparing clinical eye signs with EEG polysomnography. They showed that in young adults, the deepest level of sleep was reached on average 3 min prior to the onset of eccentric ocular positioning. What this suggests is that although a patient may appear satisfactorily anaesthetized, eccentric eye positioning may still occur. A further supposition is that it may be possible for patients to drift into lighter planes of GA intraoperatively without the knowledge of the anaesthetist, potentially resulting in the development of eccentric ocular positions.
One possible confounding factor that we have not studied is the use of narcotic premedication. There is some belief that these may help suppress the development of an eccentric eye postion;5 however, we could not find evidence from the literature to support this assertion. However, of relevance, there is some interest in the influence of brain function on the depth of anaesthesia that is achieved by a given mean alveolar concentration of inhaled drug.6 It is interesting to note that Snow first proposed that the amount of anaesthesia is not as important as the state of the central nervous system. If this is the case, then narcotic premedications may well help prevent the development of eccentric eye positions. The potential for worrying acute rises in intraocular pressure (IOP) postoperatively from nausea and vomiting limits the use of opiate premedications in ocular surgery.
In theory, there are a number of interventions, both ophthalmic and anaesthetic, which could be used to prevent this problem causing surgical difficulty. Possible ophthalmic interventions include the use of a superior rectus stay suture and the use of LA infiltrations, such as sub-tenons or peribulbar injections. While there is no doubt that LA infiltration may resolve the problem, the inconvenience of having to perform this additional intervention, perhaps at a critical stage of an intraocular procedure makes it impractical. A similar argument can be made against a superior rectus stay suture. Furthermore, in our experience, the contraction of the superior rectus is extreme and the use of a stay suture to overcome this may cause unwanted and perhaps dangerous increases in IOP. Anaesthetically, there are two options; treating the phenomenon if and when it develops, either by deepening the anaesthesia or administering muscle relaxants, or secondly, prevention in the form of a planned balanced GA including long-acting muscle relaxants. As Guedel established, achieving deep planes of anaesthesia results in flaccid extraocular muscles; however, as discussed, there are no readily available or reliable methods for determining the depth of GA. In addition, further deepening of anaesthesia comes at the physiological price of prolonged cardiorespiratory depression and may delay patient recovery. This may not be desirable in elderly patients requiring general anaesthesia.
Our preference is for patients to receive a planned balanced GA including a NDMR of at least medium duration (20 min), such as atracurium or vecuronium. This technique clearly prevents the development of eccentric eye positions and therefore averts added surgical risk. From the anaesthetic point of view, the use of muscle relaxants may prolong recovery times as reversal of the neuromuscular blockade may be required. However, the use of a medium duration NDMR curtails this problem as reversal is often not required (unlike longer-acting agents). For rapid surgery, short-acting agents such as mivacurium may still offer the advantage of avoiding reversal of neuromuscular blockade. One further note, although rare, muscle relaxants may be associated with an increased risk of a critical respiratory event,7 primarily when extubation is performed prior to full reversal.
Conclusion
In our experience, the development of an eccentric eye position can lead to significant intraoperative difficulty. More importantly, it increases the risk of complications and patient morbidity. In many ophthalmic units, the emphasis on local anaesthesia for rapid day-case surgery, often performed by the ophthalmologists, has resulted in reduced interaction with anaesthetists. Communication is important when interaction does take place in order to avoid the problem of eccentric ocular positions during surgery under GA.
In the context of clinical governance, in particular risk management, ophthalmologists should be aware of this problem so that appropriate liaison can be made with anaesthetists.
References
Gimbel HV, Neuhann T . Development, advantages, and methods of the continuous circular capsulorhexis technique. J Cataract Refract Surg. 1990; 16: 246–249.
Johnson RW, Forrest FC . Local and General Anaesthesia for Ophthalmic Surgery. Butterworth-Heinemann Ltd: Oxford, 1994.
Barry Smith G, Hamilton RC, Carr CA . Ophthalmic Anaesthesia: A Practical Handbook,, 2nd ed. Arnold: London, 1996.
Snow J . On the Inhalation of Vapour Ether in Surgical Operations. Churchill: London, 1847.
Guedel AE . Inhalation Anaesthesia. A Fundamental Guide, 1st ed. Macmillan: New York, 1937.
Power C, Crowe C, Higgins P, Moriarty DC . Anaesthetic depth at induction: an evaluation using clinical eye signs and EEG polysomnography. Anaesthesia 1998; 53: 736–743.
Rose DK, Cohen MM, Wigglesworth DF, DeBoer DP, Math M . Critical respiratory events in the postanesthesia care unit. Anesthesiology 1994; 81: 410–418.
Author information
Authors and Affiliations
Corresponding author
Additional information
The results of this study have been presented at the Annual British Ophthalmic Anaesthetic Society Meeting, June 2003.
Rights and permissions
About this article
Cite this article
Rossiter, J., Wood, M., Lockwood, A. et al. Operating conditions for ocular surgery under general anaesthesia: an eccentric problem. Eye 20, 55–58 (2006). https://doi.org/10.1038/sj.eye.6701789
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701789
Keywords
This article is cited by
-
Anästhesie in der Ophthalmologie – Ophthalmologie in der Anästhesie
Spektrum der Augenheilkunde (2010)
-
Operating conditions for ocular surgery under general anaesthesia: an eccentric problem
Eye (2007)
-
Eye positions during ocular surgery
Eye (2007)