Abstract
Aim
To survey low vision in an urban population and assess impact on quality of life, rehabilitation and support.
Methods
In a cross-sectional population survey, 66 patients were identified from databases of three general practices and surveyed by investigator administered questionnaire. Main outcome measures were ocular diagnoses, (US) National Eye Institute Visual Function-Questionnaire (NEI-VFQ) scores assessing visual and nonvisual disability, eligibility for, awareness and receipt of rehabilitation and support.
Results
Of 24 420 individuals on the lists of the three study practices, we found 101 registered as blind or partially sighted (prevalence 0.41%). A total of 66 patients participated with ocular diseases of age-related macular degeneration 39 (59%), glaucoma 11 (17%), diabetic retinopathy two (3%), retinitis pigmentosa two (3%), and 12 (18%) ‘others’. Better eye visual acuity was counting fingers or worse in 32 (48.5%). NEI-VFQ scores were poor—overall mean 41.5% (SD 23.5). In all, 80% had a social services home visit with one-third of these still in contact. In all, 66% had undergone a low vision aid assessment and 57.6% of these used their aid. The awareness and receipt of benefits arising from registration as visually impaired were lower than for other supportive measures available for reasons unrelated to vision. None had a guide dog.
Conclusions
We found expected patterns of low vision but poorer levels of function and support that may reflect age and deprivation in a population failed by the current systems for identification, registration, and rehabilitation based on legislation overtaken by demographic change and social provision independent of visual status.
Similar content being viewed by others
Introduction
Visual impairment and blindness present a significant socio-economic and social burden, both for the individual and society. In England and Wales in 1997, the Office for National Statistics estimated that there were 193 956 and 160 197 people registered as blind or partially sighted, respectively.1 In Wales, there were 9643 registered as blind and 10 565 as partially sighted by 31 March 2004.2
In the United Kingdom, a person can be registered as blind when ‘they cannot do any work for which eyesight is essential’ based on The National Assistance Act of 1948.
UK guidelines for blind registration include a Snellen visual acuity (VA) of less than 3/60 with a full field of vision and various levels of better VA in the presence of visual field defects.
There is no legal definition of partial sightedness in the UK but the suggested criteria are based on a person being ‘substantially and permanently handicapped by defective vision caused by congenital defect or illness or injury’.3 It includes VA measurement of 3/60 to 6/60 with a full field and up to 6/18 in the presence of an extensive field defect such as homonymous hemianopia.
At the time our study was undertaken, the registration process was initiated by a consultant ophthalmologist following completion of form BD8.3 Patients are assessed by a social worker and informed of the various benefits that are available. These include disability living allowance (DLA)/attendance allowance (AA), additional income support, additional housing benefit or council tax benefit, or both, exemption from ‘nondependants’ deduction from income support, housing benefit and council tax benefit, severe disablement allowance, incapacity benefit, disabled person's tax credit, help towards the cost of residential or nursing home fees, community care services and assistance from the local council, free NHS sight test, free NHS prescriptions, low vision aids, special equipment, a reader or assistance at work, help with travel costs, free postage on items marked ‘Articles for the Blind’, railcard and other travel concessions, local travel schemes, and protection via the disability discrimination act. There are a few additional benefits for the blind only. These include blind person's personal income tax allowance, reduction in television licence fee, loan of radios, cassette players and TV sound receiver, help with telephone installation charges and line rental, car parking concessions under the Blue Badge scheme, and exemption from BT directory enquiry charges.4
Aims
This study was to survey the local population of visually impaired individuals, to assess their levels of disability, including the impact on daily life, and to document the support and rehabilitation received as a result of the registration process.
Materials and methods
Visually impaired patients were identified from the databases of three local UK style Primary Health Care General Medical Practices where records were kept of patients belonging to the Practice List who had been registered as having low vision using the then existing form BD8. Details of cases identified and included in the survey are given in Table 1.
If, following an initial telephone enquiry, patients were able and agreeable they were visited in their homes by the first author (GW) where the questionnaire was administered (and VA measured using a reduced (3 m) Snellen chart, best possible conditions of illumination, and patients’ own distance correction—with or without pinhole as required). Ethics approval was granted by the local bodies responsible for supervision of this undergraduate research project.
The questionnaire was administered by the first author (GW) using standard questions for each category.
The level of visual impairment was assessed with the shortened National Eye Institute Visual Function Questionnaire (NEI-VFQ 25).5, 6, 7 The NEI-VFQ is a standardised questionnaire used in ophthalmology. It was developed in the United States by Mangione et al5 and has been adopted for worldwide use in relation to quality-of-life evaluation in patients with many different ophthalmic conditions. A number of questions are asked and scored according to the authors’ instructions in order to assess categories representing general health, general vision, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, colour vision, and peripheral vision. Near and distance VA were also assessed. Distance VA was measured using a 3 m Snellen chart at 3 m and near using a standard test type; illumination was the maximum available in the home.
Patients were also asked if they were aware of, or in receipt of the benefits they are entitled to following registration (as outlined in the introduction).
The statistics package used for the regression analysis was MultiStat version 1.11, Biosoft, Cambridge, UK.
Results
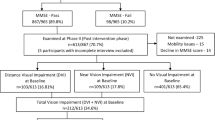
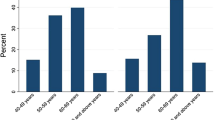
Table 1 shows the breakdown of patients included in the study and the reasons for nonparticipation. The overall numbers were 66 patients out of 101 potential (65%). Exclusions were for illness 12, not contactable at listed address 14 and nine patients refused. It is noteworthy that 10% of 101 suffered from dementia sufficient to prevent participation. Demographic and clinical characteristics are listed in Table 2. Ages ranged from 50 to 99 (mean 81.3 years).
The total number of people registered blind or partially sighted was 101 in the total population of 24 420 people (of all three general practices). The prevalence was therefore 0.41%. Ocular diagnoses leading to registration for the blind and partially sighted are shown in Table 3.
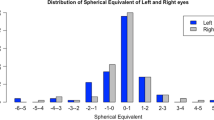
Both blind and partial sight registration criteria are based on better eye VA. The results for our patients are shown in Figure 1.
The NEI-VFQ questionnaire responses for both those registered as blind and partially sighted demonstrated low mean percentage scores in all categories with the exception of ocular pain (Figure 2). No individual surveyed was a current driver. The greatest difficulties experienced were for near, distance, and general vision activities, followed by peripheral vision, sight-specific role difficulties, dependency, mental health, and social functioning. Colour vision scores were better.
Correlation between age and percentage test scores were analysed for the group as a whole with simple regression analysis. This revealed that there was significant correlation between age and difficulties with near (r=−0.24, P=0.047) and distance activities (r=−0.26, P=0.027) and role difficulties (r=−0.29, P=0.016). There was borderline correlation with social functioning (r=−0.23, P=0.06). No significant correlation was found between age and other NEI-VFQ subscales.
Of the whole group, 48.5% had VA of counting fingers or worse in the better eye. Only 27% had VA of 6/18 or better. Out of 29, 13 patients registered as partially sighted had better eye VA less than or equal to 6/60 and are possibly eligible for re-registration as blind. In all, 65% (n=43) had near acuity less than N48.
Of the 66 patients, only 53 (80%) had received a visit by a representative from social services for an assessment. Of these, only 22 (33.3%) were still in regular contact with social services. Furthermore, only 24 (36.3%) possessed a white stick and none had a guide dog, given that 37 patients were registered blind. Of the patients, 44 (66.6%) had to negotiate steps to their front door. Aids to improve mobility and safety (handrails around the house, large knobs and handles, bathroom gadgets, stair lift) were only possessed by 24 (36%), 4 (6%), 16 (25%), and 9 (13.5%), respectively, but when present were found to be helpful. The same applied to kitchen appliances; gadgets available included; liquid level indicator, talking scales, and markings on cooker/appliances. These were possessed by 26 (40%), 8 (12%), and 18 (27%) patients, respectively. In all, 29 (44%) patients possessed a speaking watch/clock. In addition to our observation that uptake of practical aids was less than universal, we noted that the distribution of aids was irregular; that is, while 10 individuals possessed six or more (out of a possible 15 types of aid) 43 had five or fewer, and nine had none at all. Simple regression analysis showed no correlation between number of aids possessed and overall NEI-VFQ visual function score (r=−0.03, P=0.93).
Despite an incomplete delivery of formal low visual aid (LVA) assessments (n=44, 66%), 54 (82%) possessed an LVA of which 38 (70%) found their aid to be of use. Thus, it would appear that at least 18% were acquiring LVAs of their volition. Most LVAs were simple magnifiers with only a small minority having more sophisticated appliances such as spectacle mounted Galilean telescopes.
The UK benefits system is complex. This is apparent from the low levels of awareness and uptake of some of the social and financial benefits arising from registration as blind or partially sighted (Table 4). In contrast, most patients were aware of more generic entitlements as a result of age or income and living in their part of Wales (Table 4).
Finally, we asked about comorbidity and smoking among our patients. Six (9%) had Type II diabetes mellitus, 22 (33.3%) were hypertensive, 17 (25.7%) had ischaemic heart disease (of which nine had a myocardial infarction), 13 (19.6%) had suffered a cerebrovascular accident, and 10 (15%) were current smokers. There was some overlap.
Discussion
Losing vision is a profound event in the life of any individual. But it is not only sight that is lost. Independence, confidence, self-esteem, ability to cope, and care for self and others may also be adversely affected. Psychosocial comorbidity may ensue.
We found patterns of low vision as expected for the UK and other Western societies. In Swansea and Neath/Port Talbot, there are 1386 individuals registered as blind and 1791 as partially sighted.2 Nevertheless, we are unable to rule out some failure of case identification in our population and so the true prevalence of low vision can only be estimated—particularly considering our population which is relatively elderly and has a high prevalence of diabetes. This would appear to be likely for our Neath-based population (Table 2). Given that reported life expectancy for Wales (1998–2000 data) is 74.8 years for male subjects and 79.7 years for female subjects in 1998–2000, this would appear to represent either a true excess of low vision in female subjects or significant under-detection in male subjects.8
Our proportions for registration for AMD, glaucoma, and diabetic retinopathy were consistent with reports of other workers.9, 10, 11, 12, 13, 14
In our study, cataract (a remediable condition) was not a cause of registration compared with 3% of blind registrations in the report of Evans et al.1 In general, the levels of disability were worse for those registered blind than for the partially sighted. We also found that several individuals classified as partially sighted are actually eligible for registration as blind. Clearly such individuals have a progressive condition and their changing needs have to be addressed. Visual function results for near and distance vision and difficulties in fulfilling an individual's role were inversely correlated with age in agreement with findings of the Beaver Dam Eye Study.15
Of the studies utilising the NEI-VFQ to investigate visual function,6, 7 none have demonstrated mean scores as low as in our study. Brody et al16 compared NEI-VFQ scores in nondepressed and depressed patients with AMD. Their depressed group had somewhat higher mean scores than in our study; indeed some had VA sufficient for driving (Table 5). The Wisconsin Epidemiologic Study of Diabetic Retinopathy6 used the NEI-VFQ-25 to determine quality of life in people with varying severity of VA, retinopathy, and a number of comorbid factors associated with diabetes mellitus. They found that poorer mean scores were strongly associated with worsening vision but again, scores were higher than in our study (Table 5).
We are unable to give a robust explanation for the low scores we obtained from our patients in response to what is a clearly written and well-validated questionnaire. It is possible that our patients really do have lower visual function and that they are adversely affected by factors such as depression—as for the group in Brody's study16 which they most closely resemble.
To the best of our knowledge, this is the first report of its type to deal not only with the effects of visual loss but also the perceptions and receipt of social benefits, with significant contributions coming from the partially sighted. The optimum time for intervention and support for those with low vision is immediately following confirmation of ocular diagnosis and eligibility for registration. Current systems involve referral for this confirmation by a consultant ophthalmologist. The Hospital Eye Service suffers from long waiting times (currently many months in South Wales) and assessment by Social Services is also subject to considerable delay (several months in West Glamorgan). Only then is a patient in a position to start to benefit from the support and rehabilitation they need. The majority of patients in our study would not appear to have benefited fully from their registration as visually impaired. And even this finding relates to those who have been identified as having visual rehabilitation needs. Our wider population need may well be greater.
The documentation for the registration process has recently been modified with the introduction of the United Kingdom Certificate of Visual Impairment (CVI), which is still completed by a consultant ophthalmologist in secondary care. To supplement this a Letter of Visual Impairment (LVI) is initiated in the primary care setting to allow social services assessment and support to be commenced while the patient is awaiting formal confirmation of diagnosis by a consultant. Given the workload of the Hospital Eye Service in managing treatable ocular pathology, it is perhaps better for the initiation of multidisciplinary support for the untreatable visually impaired to be relocated to a primary care setting. This issue has been addressed to some extent by the introduction of the LVI and CVI. Furthermore, primary care optometrists are well placed to deliver the simple magnification aids that most patients in our and others’ studies17, 18, 19, 20 found to be of most practical help. Such a move to low vision aid provision in primary care has been made in Wales.21
It will be of interest to repeat our survey in a few years time to evaluate the effects of such initiatives on the identification of and provision of support to those with low vision together with any impact made on the quality of life.
References
Evans J, Rooney C, Ashwood F, Dattani N, Wormald RW . Blindness and partial sight in England and Wales: April 1990–March 1991. Health Trends 1996; 28 (1): 5–12.
Disability Register. Welsh Assembly Government Figures. http://www.dataunitwales.gov.uk/pss/Data.asp?cat=252, 2004.
Publications T . National Health Service Record of examination to certify a person as blind or partially sighted. Form BD8. 1990.
Royal National Institute of the Blind (RNIB). Benefits and Concessions for Registered Blind and Partially Sighted. RNIB: London, 1997.
Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD . Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 2001; 119 (7): 1050–1058.
Klein R, Moss SE, Klein BEK, Gutierrez P, Mangione CM . The NEI-VFQ-25 in people with long-term type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Arch Ophthalmol 2001; 119 (5): 733–740.
Stelmack JA, Stelmack TR, Massof RW . Measuring low-vision rehabilitation outcomes with the NEI VFQ-25. Invest Ophthalmol Vis Sci 2002; 43 (9): 2859–2868.
Life expectancy in Wales 1998–2000. Welsh Assembly Government Figures.http://www.wales.gov.uk/keypubstatisticsforwalesheadline/content/health/2002/hdw20020307-e.htm.
Leibowitz HM, Krueger DE, Maunder LR, Milton RC, Kini MM, Kahn HA et al. The Framingham Eye Study monograph: an ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973–1975. Surv Ophthalmol 1980; 24 (Suppl): 335–610.
Vingerling JR, Dielemans I, Hofman A, Grobbee DE, Hijmering M, Kramer CF et al. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology 1995; 102 (2): 205–210.
Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology 1992; 99 (10): 1499–1504.
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99 (6): 933–943.
Klein R, Klein BE, Tomany SC, Meuer SM, Huang GH . Ten-year incidence and progression of age-related maculopathy: The Beaver Dam Eye Study. Ophthalmology 2002; 109 (10): 1767–1779.
Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P . Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol 1993; 77 (1): 17–21.
Klein BE, Klein R, Lee KE, Cruickshanks KJ . Associations of performance-based and self-reported measures of visual function. The Beaver Dam Eye Study. Ophthalmic Epidemiol 1999; 6 (1): 49–60.
Brody BL, Gamst AC, Williams RA, Smith AR, Lau PW, Dolnak D et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology 2001; 108 (10): 1893–1900; discussion 1900-1.
Leat SJ, Rumney NJ . The experience of a university-based low vision clinic. Ophthalmic Physiol Opt 1990; 10 (1): 8–15.
Bailey I . Low vision and the elderly patient. J Am Optom Assoc 1988; 59 (4 Part 1): 307–311.
Ji YH, Park HJ, Oh SY . Clinical effect of low vision aids. Korean J Ophthalmol 1999; 13 (1): 52–56.
Fonda GE . Designing half-eye binocular spectacle magnifiers. Surv Ophthalmol 1991; 36 (2): 149–154.
Margrain TH, Ryan B, Wild JM . A revolution in Welsh low vision service provision. Br J Ophthalmol 2005; 89: 933–934.
Acknowledgements
The National Eye Institute Visual Function Questionnaire (NEI-VFQ) was developed by RAND (RAND Health Program, Santa Monica, California (www.rand.org)) under the sponsorship of the National Eye Institute (USA).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work been presented as a poster at the Royal College of Ophthalmology Annual Congress, Birmingham, May 2003
Rights and permissions
About this article
Cite this article
Williams, G., Pathak-Ray, V., Austin, M. et al. Quality of life and visual rehabilitation: an observational study of low vision in three general practices in West Glamorgan. Eye 21, 522–527 (2007). https://doi.org/10.1038/sj.eye.6702256
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702256