Abstract
Aims
To assess the effect of Nd:YAG laser posterior capsulotomy in the context of unilateral posterior capsular opacification (PCO) on spatial acuity, contrast sensitivity, and stereoacuity.
Methods
This prospective study involved 60 consecutive subjects with unilateral PCO. The aforementioned parameters of visual function were assessed immediately prior and 3 weeks subsequent to unilateral posterior capsulotomy.
Results
In eyes that underwent laser posterior capsulotomy, the median spatial acuity (log minimum angle of resolution (MAR)) improved from 0.34 (20/44) to 0.16 (20/29) (P=<0.001, Wilcoxon test), while the median contrast sensitivity improved from 22.4 to 35.5 dB (P=<0.001, Wilcoxon test) after posterior capsulotomy. Fellow eyes exhibited negligible change in these visual parameters. The median stereoacuity improved from 240 to 60 s of arc (P=<0.001, Wilcoxon test).
Conclusion
In the context of unilateral opacification of the posterior capsule, Nd:YAG laser posterior capsulotomy affords significant improvement in stereoacuity, apparently in excess of improvements in spatial acuity and contrast sensitivity. Routine measurement and documentation of these parameters of visual function is recommended especially when subjective visual disability appears disproportionate with impairment of spatial acuity.
Similar content being viewed by others
Introduction
Posterior capsular opacification (PCO) is a common late sequel of uncomplicated modern cataract surgery, the prevalence of which has been estimated at up to 50% at 5 years after surgery.1 PCO may symptomatically compromise visual acuity, contrast sensitivity, produce excessive glare, or alternatively, compromise the adequacy of visualisation of the fundus for diagnostic and/or therapeutic purposes, all of which constitute indications for intervention. Treatment involves the creation of an optically clear opening in the posterior capsule by photodisruption with the Neodymium:Yttrium–Aluminium–Garnet laser (Nd:YAG laser), commonly termed YAG laser capsulotomy.
Improvements in both spatial visual acuity and contrast sensitivity are well documented after posterior capsulotomy.2 We are, however, unaware of any published literature in relation to stereoacuity in the context of unilateral PCO, and by extension, the effect of unilateral posterior capsulotomy on this parameter of visual function. This study was therefore designed to study this phenomenon.
Materials and methods
With formal approval from the West Somerset Research Ethics Committee, 60 consecutive individuals with unilateral PCO, with visual acuity of log minimum angle of resolution (MAR) 0.5 (20/63), or better in the contralateral eye were recruited into a prospective study over a 9-month period. Exclusion criteria included a history of complicated cataract surgery, amblyopia, a history of squint or any known deficiency of binocular single vision. Contralateral eyes were phakic with minimal/no lens opacity or pseudophakic with clear posterior capsules.
With informed consent from each subject, spatial visual acuity (logMAR), contrast sensitivity (Pelli–Robson) in both eyes and stereoacuity (TNO) were measured by one researcher (TB) before unilateral posterior capsulotomy. The TNO test was employed in preference to other tests of stereopsis (Titmus and Frisby), since by not offering the subject monocular clues it thus affords a more robust measurement of stereopsis. The surgical procedure involved the creation, by one of three possible surgeons, of an opening of 4 mm diameter in the posterior capsule, with the Nd:YAG laser, without correcting for magnification. The subjects were reviewed 3 to 5 weeks subsequent to YAG laser capsulotomy, when these parameters of visual function were re-measured, by the same researcher, who however, no longer had access to the precapsulotomy measurements.
For comparison, visual acuity scores were converted (antilogarithm) from logMAR to the MAR expressed in minutes of arc; log contrast sensitivity (log CS) as measured on the Pelli–Robson chart was converted (antilogarithm) and expressed in decibels (dB); and stereoacuity was expressed in seconds of arc. The results were analysed with a Wilcoxon test.
Results
Spatial acuity
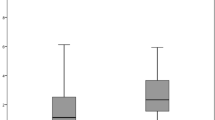
Eyes that underwent posterior capsulotomy exhibited an improvement in the median logMAR visual acuity from 0. 34 (20/44) to 0.16 (20/29), prior and subsequent to laser capsulotomy, respectively (P<0.001, Wilcoxon test; Tables 1 and 2). For fellow eyes, the median logMAR visual acuity remained unchanged at 0.20 (20/32).
Contrast sensitivity
Eyes that underwent laser capsulotomy displayed an improvement in median log CS from 1.35. (22.4 dB) to 1.55 (35.5 dB) (P<0.001, Wilcoxon test). For fellow eyes, the median log CS remained relatively unchanged at 1.50 and 1.53 prior and subsequent to laser capsulotomy.
Stereoacuity
Median stereoacuity improved from 240 to 60 s of arc (P=<0.001, Wilcoxon test) after laser capsulotomy.
Discussion
The most commonly measured parameter of visual function is that of spatial acuity. By extension this is therefore often a major determinant in the decision to proceed to surgical intervention such as cataract surgery or laser posterior capsulotomy. Though it is well recognised that other aspects of visual function may be compromised by media opacity, measurement of such parameters is not commonly undertaken in clinical practice.
Opacification of the posterior capsule may result in impaired spatial acuity, contrast sensitivity, stereoacuity, and glare, all of which have the potential to cause significant subjective visual disability, often out of proportion to diminution of spatial acuity. Impaired stereoacuity is a well-recognised consequence of unilateral visual impairment.3 Accordingly, improved stereoscopic vision has been demonstrated in the context of second eye cataract surgery.4, 5
Our results conclusively demonstrate the deleterious effect of unilateral PCO on stereoacuity and the considerable improvement that accrues from laser capsulotomy in this context. It is well recognised that after laser capsulotomy, improvement in contrast sensitivity often exceeds that in spatial acuity; our results show that the magnitude of improvement of stereoacuity is comparable with that of contrast sensitivity. Such improved stereoacuity carries significant benefits in everyday life.
We therefore suggest that measurement of both stereoacuity and contrast sensitivity is important for any individual with media opacity, in whom subjective visual disability appears disproportionate to diminution of spatial acuity. Not only does this afford a more thorough assessment of visual disability—in this age of ever increasing litigation, a documented deficiency of either of these parameters serves the important function of justifying the performance of a surgical procedure, with its attendant risks.
References
Apple DJ, Solomon KD, Tetz MR, Assia EI, Holland EY, Legler UF et al. Posterior capsule opacification. Surv Ophthalmol 1992; 37 (2): 73–116.
Magno BV, Datiles MB, Lasa MS, Fajardo MR, Caruso RC, Kaiser-Kupfer MI . Evaluation of visual function following neodymium:YAG laser posterior capsulotomy. Ophthalmology 1997; 104 (8): 1287–1293.
Kwapiszeski BR, Gallagher CC, Holmes JM . Improved stereoacuity: an indication for unilateral ataract surgery. J Cataract Refract Surg 1996; 22 (4): 441–445.
Talbot EM, Perkins A . The benefit of second eye cataract surgery. Eye 1998; 12 (6): 983–989.
Laidlaw A, Harrad R . Can second eye cataract extraction be justified? Eye 1993; 7 (5): 680–686.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests/research funding: none
Competing interests: none
Rights and permissions
About this article
Cite this article
Menon, G., Wong, K., Bundhun, T. et al. The effect of Nd:YAG laser posterior capsulotomy on stereoacuity. Eye 23, 186–189 (2009). https://doi.org/10.1038/sj.eye.6702932
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702932
Keywords
This article is cited by
-
The influence of mild posterior capsular opacification on spectral domain optical coherence tomography retinal nerve fiber layer thickness
International Ophthalmology (2022)
-
Comparison of wavefront aberrations in eyes with multifocal and monofocal iols before and after Nd:YAG laser capsulotomy for posterior capsule opacification
International Ophthalmology (2020)