Abstract
Aims
To determine the nature and prevalence of ophthalmological findings for a cohort of children in a paediatric cochlear implant program and to assist the clinician in devising an investigative plan for this population.
Methods
Retrospective medical record review of children who underwent multichannel cochlear implantation at a tertiary care hospital between February 1996 and July 2008.
Results
In all, 141 children (mean age 28 months, range 16 months to 9 years) had complete medical record documentation consisting of orthoptic and opthalmological examination, including cycloplegic refraction. A total of 59 children (41.8%) had ocular abnormalities with refractive errors being the most common abnormality. Hypermetropia was the most common refractive error and was found in 21 children (14.8%). Strabismus was found in six patients, with constant esotropia being the most common. Ocular pathology (excluding refractive or muscle abnormalities) were found in nine patients (6.3%). Three patients had syndromes associated with ocular findings including Waardenburg and Usher syndrome. During the follow-up period, 14 children were fitted with prescription lenses, 3 had strabismus surgery, and 2 underwent ptosis.
Conclusions
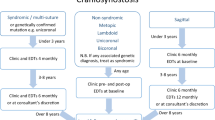
Routine orthoptic and ophthalmologic examination can be beneficial in the initial evaluation of children assessed for cochlear implants. Electroretinography is useful in evaluating children with unexplained congenital sensorineural hearing loss, suggestive symptoms including night blindness, unexplained reduction in visual acuity, or delayed motor milestones. Routine yearly follow-up may aid in the detection of changing refractive errors and the possibility of later-onset retinal degeneration.
Similar content being viewed by others
Introduction
Cochlear implants have steadily improved over the last decades, dramatically changing the prospects for profoundly deaf children.1 A majority of cases of congenital and infantile hearing loss are sensorineual in origin. These devices are thus successful in restoring some hearing by electrical stimulation of proximal neural elements. It is now accepted that early cochlear implantation may facilitate rapid transformation of a deaf child to a fully functioning member of the community.2
Ophthalmic problems in deaf children have a serious effect on development of their communication skills. As visual and auditory channels are responsible for more than 95% of information acquisition,3 any ophthalmic disorder may thus negatively affect on this process. It is well documented that the incidence of visual problems is higher among the deaf than a corresponding population of hearing individuals.4, 5, 6
At referral for cochlear implantation, the specialist service should arrange for the child to be seen by an orthoptist and an ophthalmologist as soon as possible. This assessment may need to be repeated at intervals after the diagnosis.7 The aims of screening for ophthalmic disorders are to identify any ocular abnormality limiting visual acuity, any pigmentary retinopathy, or optic nerve abnormality. Some disorders may be correctable (eg, refractive) or treatable (eg, cataracts).8 It is crucial to establish normal visual acuity, as hearing-impaired children are extremely dependent on vision to compensate for the loss of auditory input.4 Those children with non-correctable and non-treatable visual disorders, such as retinitis pigmentosa in Usher's syndrome, are especially good candidates for early cochlear implants, which will improve listening and spoken language skills.9
Deaf blindness is more than the sum of deafness and blindness on their own. It is a unique and entirely different condition requiring a multi-disciplinary approach.10 Deaf children are heavily dependent on their sense of vision to develop efficient communication skills. Hearing and visually impaired children are significantly affected, being less able to lip read, less cooperative, and less capable of manual tasks then hearing-impaired children with normal vision.11 If unrecognized, especially in the early years of life, children may fail to develop the ability to develop linguistic and communicative skills, with a significant effect on education, socioemotional development, and future professional prospects.
The objective of this study was to determine the nature and prevalence of ophthalmological findings for a cohort of children in a paediatric cochlear implant program and to assist the clinician in devising an investigative plan for this population.
Materials and methods
Study population
The study was a retrospective review of the medical records of 196 children who underwent multichannel cochlear implantation at Beaumont University Hospital, Dublin, Ireland between February 1996 and July 2008. Beaumont University Hospital is the National Irish Referral Centre for Cochlear Implants and is a member of the British Cochlear Implant Group representing all the Cochlear Implant Centres throughout the United Kingdom and Ireland. Cases were identified through the electronic database of paediatric patients who received a cochlear implant.
Data collection
Data collected from the medical records included patient gender, age, cause of hearing loss (if known), relevant prenatal, perinatal and postnatal factors, family history of hearing loss, genetic testing results, and orthoptic and ophthalmological assessment.
Visual assessment included visual acuity (Snellen letters, Sheridan Gardner singles, Kay pictures, Cardiff Acuity Cards, or fixation/following evaluation), cover test, complete motility examination, and binocular function evaluation (Frisby stereoacuity) by an orthoptist. Convergence and optokinetic nystagmus were recorded. All children underwent slitlamp examination, direct and indirect ophthalmoscopy, and cycloplegic retinoscopy by an ophthalmologist. Electrodiagnostic tests were not performed routinely. Patients underwent yearly control evaluations after the initial diagnosis unless otherwise indicated.
Results
Records of 141 ophthalmological examinations carried out in our department during the study period were available for review. All 141 children (mean age 28 months, range 16 months to 9 years) had complete medical record documentation consisting of orthoptic and opthalmological examination, including cycloplegic refraction. The ophthalmological findings and aetiology of deafness are summarized in Tables 1 and 2, respectively. The criteria for defining a vision disorder as significant were obtained from the study on children with severe and profound sensorineural deafness by Armitage et al.5
Visual function was remarkably good in our patients with only 34 children (23.6%) having visual acuity worse than six out of nine patients. A total of 59 children (41.8%) had ocular abnormalities with refractive errors being the most common abnormality. Hypermetropia was the most common refractive error and was found in 21 children (14.8%). Strabismus was found in six patients, with constant esotropia being the most common. Ocular pathology (excluding refractive or muscle abnormalities) were found in nine patients (6.3%). In one patient, visual loss occurred in early childhood because of congenital horizontal pendular nystagmus.
One child was diagnosed with Waardenburg syndrome after the finding of iris heterochromia and telecanthus. Two patients with an unidentified cause of deafness and positive history for late walking (mean age 25 months), were diagnosed with Usher syndrome after abnormal electroretinography. During follow-up, reduced visual acuity, optic disc pallor, and attenuated retinal vessels occurred at the age of 5 years; however, retinitis pigmentosa occurred only later than the age of 8 years, comparable to that in children described earlier. During the follow-up period, 14 children were fitted with prescription lenses, two underwent ptosis surgery and three children had strabismus surgery.
Discussion
Earlier studies have reported a high incidence of visual impairment among the hearing-impaired population. (Table 3) Most of them assessed deaf children in residential or day schools and included children of all ages and causes. Only one other study assessed children who underwent cochlear implantation.25 This retrospective study with a 12-year follow-up, provides data on the prevalence and characteristics of ophthalmological findings after screening of a paediatric cochlear implant population. Follow-up for many of our patients was long enough to show objective benefit to our patients.
Consistent findings show that 12–60% of deaf children have significant vision impairment (Table 3). These studies vary in patient population, the types of visual problems they have assessed, the tests used, and the criteria to define and classify visual impairment. Thus, the incidence rates for specific visual problems are often not directly comparable across studies. In a comparative analysis,4 the incidence of visual impairment in the hearing-impaired group is more than two and a half times higher than that found in a normal school population.6
The role of screening is to determine visual acuity and identify abnormalities amenable to specific treatment and better overall management. Second, this on-going commitment aids in identification of hereditary hearing loss syndromes that are associated with ocular findings. Several authors concluded that deaf students had a high frequency of eye disease,7, 22, 27 and that early diagnosis and treatment could improve their quality of life and that the potential benefits of ophthalmologic screening in deaf children is enormous.22 Armitage et al5 found that in 48% of deaf children, visual impairment had remained undetected before screening. The British National Screening committee recommended that children with deafness should have routine expert eye examination performed by an orthoptist and ophthalmologist.7 Our findings suggest that all children assessed for cochlear implants would benefit from routine ophthalmic assessment.
Ocular findings are quite variable and could affect the anterior and posterior segment of the eye with abnormal development of the lens, optic nerve, and retina. These higher rates of ocular abnormality have been attributed to the retina and cochlea maturing during the same embryological period (fourth embryonic week) from the same embryonic layer (ectoderm), which may be susceptible to genetic and/or environmental factors.8 The most frequent ophthalmic finding is refractive errors (26.4%), similar to the earlier studies. Fourteen of our patients with refractive errors were fitted with corrective spectacles. Correction of refractive errors has been found to bring significant improvement even in motor behaviours.32
In a prospective study of the prevalence of vision disorders, other than refractive anomalies, the most prevalent conditions in the clinical paediatric population are binocular and accommodative disorders.33 At initial assessment, binocular vision was reduced and absent in 9.7 and 4.2%, respectively, similar to previously reported.5 The incidence of manifest strabismus in our study (8.4%) was significantly higher than that of 4.6% found in a normal population.6 During the follow-up period, 11 children (7.8%) underwent conservative or surgical correction.
The likelihood of visual impairment is independent of the aetiology of the hearing loss. Armitage et al5 did not find any statistically significant difference in the incidence of visual impairment among the congenital and acquired hearing-impaired groups. However, children with deafness >80 dB had a statistically significant increase in the prevalence of retinal abnormality compared with children with deafness <80 dB.24
Studies of hearing-impaired populations indicate a genetic basis in approximately 50% of all hearing loss.34 Cochlear implant assessment includes imaging studies and genetic testing in addition to ophthalmologic referral. Despite the enormous heterogeneity of genetic hearing loss, variants in one locus, Gap Junction Beta 2 (GJB2) or connexin 26 (CX26), account for up to 50% of cases of nonsyndromic sensorineural hearing loss.35 We did not find any ophthalmological abnormalities in the subgroup of 15 patients with CX26 mutations. Rarely, autosomal dominant CX26 mutations may result in Keratitis-Ichthyosis-Deafness (KID) syndrome characterized by congenital hearing loss associated with skin lesions and vascularizing keratitis.36
Approximately 15–30% of hereditary hearing impairment involves other organ systems and occurs as a syndrome. In addition, abnormal ocular findings are associated with certain common deafness syndromes. In 8% of congenitally deaf children examined, eye examination confirmed a previously suspected cause of deafness, and in another 8%, a diagnosis that had not been suspected was made.37 Thus, ophthalmic examination may prove invaluable to identify or clarify the cause of deafness such as CHARGE association, Usher syndrome or congenital CMV or Rubella.7
Some studies recommend electrodiagnostic testing as part of routine ophthalmologic evaluation of children with sensorineural hearing loss to identify Usher syndrome.9, 25 Electroretinography is a noninvasive test that identifies retinitis pigmentosa before the onset of funduscopic and visual abnormalities. Mets et al9 found a 10% prevalence of Usher's syndrome in children with severe to profound sensorineural hearing loss. Two patients in our group, with an unidentified cause of deafness and positive history for late walking, were diagnosed with Usher syndrome after abnormal electroretinography. Retinitis pigmentosa occurred only later with long-term follow-up after the age of 8 years. As early retinal changes are uncommon, electroretinography should be considered in children with unexplained profound congenital sensorineural hearing loss and delayed motor milestones.38
The limitations of this study should be noted. First, a major limitation of our study was its retrospective nature. Second, the results of ophthalmologic examinations were unavailable for many of our patients, introducing the possibility of selection bias. Many of our patients were referred to their local ophthalmologists for assessment before the introduction of mandatory ophthalmology screening, the results of which were unavailable. Despite these limitations, we believe our data support routine ophthalmological screening of children in the cochlear implant population.
The high prevalence of visual abnormalities in the paediatric cochlear implant population emphasizes the importance of thorough ophthalmological screening. The first aim is to determine visual acuity. Some of the symptoms can be successfully corrected surgically, ensuring better visual development and improving the quality of life after cochlear implantation. Second, uncommon ophthalmological manifestations can be used in identification of hereditary hearing loss syndromes that are associated with ocular findings.
It remains to be agreed which tests should be performed. Routine orthoptic and ophthalmologic examination can be beneficial in the initial evaluation of children assessed for cochlear implants. Electroretinography is useful in evaluating children with unexplained congenital sensorineural hearing loss, suggestive symptoms including night blindness, unexplained reduction in visual acuity, or delayed motor milestones. Routine yearly follow-up may aid in the detection of changing refractive errors and the possibility of later-onset retinal degeneration.
References
Owens D, Espeso A, Hayes J, Williams RG . Cochlear implants: referral, selection and rehabilitation. Curr Paediatr 2006; 16: 360–365.
Migirov L, Carmel E, Kronenberg J . Cochlear implantation in infants: special surgical and medical aspects. Laryngoscope 2008; 118 (11): 2024–2027.
Fillman RD, Leguire E, Rogers GL, Bremer DL, Fellows RR . Screening for vision problems, including Usher's syndrome, among hearing impaired students. Am Ann Deaf 1987; 132: 194–198.
Regenbogen L, Godel V . Ocular deficiencies in deaf children. J Pediatr Ophthalmol Strabismus 1985; 22: 231–233.
Armitage IM, Burke JP, Buffin JT . Visual impairment in severe and profound sensorineural deafness. Arch Dis Childhood 1995; 75: 53–56.
Coleman HM . An analysis of the visual status of an entire school population. J Am Optom Assoc 1970; 41 (4): 341–347.
Vision care for deaf children and young adults. Guidelines for professionals working with deaf children, SENSE/NDCS, 200.
Nikolopoulos TP, Lioumi D, Stamataki S, O'Donoghue GM . Evidence-based overview of ophthalmic disorders in deaf children: a literature update. Otol Neurotol 2006; 27: S1–S24.
Mets MB, Young NM, Pass A, Lasky JB . Early diagnosis of Usher syndrome in children. Trans Am Ophthalmol Soc 2000; 98: 237–242.
Russell-Eggitt I . The deaf-blind child. In: Taylor D (ed). Paediatric Ophthalmology. Wiley-Blackwell: Oxford, 1997, p 1053.
Suchman RG . Visual impairment among deaf children. Frequency and educational consequences. Arch Ophthalmol 1967; 77 (1): 18–21.
Lawson Jr LJ, Myklebust HR . Ophthalmological deficiencies in deaf children. Except Child 1970; 37: 17–20.
Luhr JP, Dayton KK . Combining clinical and educational services. Am Ann Deaf 1971; 116: 566–568.
Alexander JC . Ocular abnormalities among congenitally deaf children. Can J Ophthalmol 1973; 8: 428–433.
Pollard G, Neumaier R . Vision characteristics of deaf students. Am J Optom Physiol Opt 1974; 51: 839–846.
Mohindra I . Vision profile of deaf children. Am J Optom Physiol Opt 1976; 53: 412–419.
English J . A five-state study of Usher's syndrome: incidence and service implications. Am Ann Deaf 1978; 123: 361–364.
Quinsland LK, Caccamise F, Johnson D . Identification of visual impairments among hearing-impaired persons and implications for educational programs: a preliminary report. Am Ann Deaf 1978; 123: 406–416.
Johnson DD, Caccamise F, Rothblum AM, Hamilton LF, Howard M . Identification and follow-up of visual impairments in hearing-impaired populations. Am Ann Deaf 1981; 126 (3): 321–360.
Walters JW, Quintero S, Perrigin DM . Vision: its assessment in school-age deaf children. Am Ann Deaf 1982; 127 (4): 418–432.
Woodruff ME . Differential effects of various causes of deafness on the eyes, refractive errors, and vision of children. Am J Optom Physiol Opt 1986; 63 (8): 668–675.
Rogers GL, Fillman RD, Bremer DL, Leguire LE . Screening of school-aged hearing impaired children. J Pediatr Ophthalmol Strabismus 1988; 25: 230–232.
Ma QY, Zeng LH, Chen YZ, Li ZY, Guo XM, Dai ZY et al. Ocular survey of deaf-mute children. Yan Ke Xue Bao 1989; 5 (1–2): 44–46.
Leguire LE, Fillman RD, Fishman DR, Bremer DL, Rogers GL . A prospective study of ocular abnormalities in hearing impaired and deaf students. Ear Nose Throat J 1992; 71: 643–646.
Siatkowski RM, Flynn JT, Hodges AV, Balkany TJ . Ophthalmologic abnormalities in the pediatric cochlear implant population. Am J Ophthalmol 1994; 118: 70–76.
Elango S, Reddy TN, Shriwas SR . Ocular abnormalities in children from a Malaysian school for the deaf. Ann Trop Paediatr 1994; 14: 149–152.
Brinks MV, Murphey WH, Cardwell W, Otos M, Weleber RG . Ophthalmologic screening of deaf students in Oregon. J Pediatr Ophthalmol Strabismus 2001; 38 (1): 11–15.
Mafong DD, Pletcher SD, Hoyt C, Lalwani AK . Ocular findings in children with congenital sensorineural hearing loss. Arch Otolaryngol Head Neck Surg 2002; 128 (11): 1303–1306.
Guy R, Nicholson J, Pannu SS, Holden R . A clinical evaluation of ophthalmic assessment in children with sensori-neural deafness. Child Care Health Dev 2003; 29 (5): 377–384.
Hanioǧlu-Kargi S, Köksal M, Tomac S, Uǧurba SH, Alpay A . Ophthalmologic abnormalities in children from a Turkish school for the deaf. Turk J Pediatr 2003; 45 (1): 39–42.
Bakhshaee M, Banaee T, Ghasemi MM, Nourizadeh N, Shojaee B, Shahriari S et al. Ophthalmic disturbances in children with sensorineural hearing loss. Eur Arch Otorhinolaryngol 2009; 266 (6): 823–825.
Kwok SK, Ho PC, Chan AK, Gandhi SR, Lam DS . Ocular defects in children and adolescents with severe mental deficiency. J Intellect Disabil Res 1996; 40 (Pt 4): 330–335.
Scheiman M, Gallaway M, Coulter R, Reinstein F, Ciner E, Herzberg C et al. Prevalence of vision and ocular disease conditions in a clinical pediatric population. J Am Optom Assoc 1996; 67 (4): 193–202.
Grundfast KM, Atwood JL, Chuong D . Genetics and molecular biology of deafness. Otolaryngol Clin North Am 1999; 32 (6): 1067–1088.
Kenneson A, Van Naarden Braun K, Boyle C . GJB2 (connexin 26) variants and nonsyndromic sensorineural hearing loss: a HuGE review. Genet Med 2002; 4 (4): 258–274.
Richard G, Rouan F, Willoughby CE, Brown N, Chung P, Ryyanen M . Missense mutations in the GJB2 encoding connexin-26 cause the ectodermal dysplasia keratitis-ichthyosis-deafness syndrome. Am J Hum Genet 2002; 70 (5): 1341–1348.
Campbell CW, Polomeno RC, Elder JM, Murray J, Altosaar A . Importance of an Eye examination in identifying the cause of congenital hearing impairment. J Speech Hear Disord 1981; 46: 258–261.
Rajput K, Bitner-Glindzicz M, Fonseca S, Mac Ardle B . Aetiological investigation into severe to profound permanent hearing loss in children. British Association of Audiovestibular Physicians and British Association of Paediatricians in Audiology (October 2008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Falzon, K., Guerin, M., Fulcher, T. et al. Ophthalmological screening of a paediatric cochlear implant population: a retrospective analysis and 12-year follow-up. Eye 24, 1031–1036 (2010). https://doi.org/10.1038/eye.2009.248
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.248