Abstract
Purpose
To analyze whether an association exists between keratometric and pachymetric changes in the cornea, and whether it can be used to create pachymetric cutoff criteria secondary to keratometric criteria.
Methods
In this cross-sectional study, 1000 candidates presenting to the refractive surgery services of a tertiary care hospital underwent bilateral Orbscan IIz (Bausch and Lomb) assessment along with other ophthalmic evaluation.
Results
Stepwise regression analysis-based models showed that simulated keratometry (simK) astigmatism was significantly predicted by the minimum corneal thickness (MCT) and difference between central and MCT (δCT), mean SimK by the MCT and δCT, and maximum keratometry in the central 10-mm zone by the MCT and δCT (P<0.001). The mean MCT values were 542.5±39.6, 539.9±39.2, 524.2±49.5, and 449.3±73.7 μm for flatter normal (<44 D), steeper normal (≥44 D), keratoconus suspect and keratoconic eyes, respectively (P<0.001). The mean differences between central corneal thickness and MCT (δCT) were 12.2±7.1 μm, 12.4±7.4 μm, 14.4±8.9 μm and 23.2±10.1 μm for the flatter normal, steeper normal, keratoconus suspect, and keratoconic eyes, respectively (P<0.001). Mean and 2SD cutoff were used to suggest that a cornea having MCT<461 μm or δCT>27 μm has only a 2.5% chance of being normal and not a keratoconus suspect or worse.
Conclusion
Pachymetric diagnostic cutoffs can be used as adjuncts to the existing topographic criteria to screen keratoconus suspect and keratoconic eyes.
Similar content being viewed by others
Introduction
Keratoconus is a usually bilateral, progressive, non-inflammatory pathology of the cornea leading to its thinning and ectasia.1 Several researchers have worked on the grading criteria for keratoconus.2, 3, 4, 5, 6 Most of the grading criteria take into account either keratometric or clinical signs to classify keratoconic and pre-keratoconic corneas. Recently, attempt has been made to use other factors such as ocular hysteresis and corneal wavefront in grading and classifying this disease.7, 8, 9, 10 Keratoconus often involves thinning as well as protrusion of the cornea. The diagnosis of keratoconus on the basis of pachymetric evaluation has been attempted in the past. Rabinowitz et al11 suggested that ultrasonic pachymetry is not as useful as keratometric classification in excluding and diagnosing keratoconus. In contrast, Watters and Owen12 demonstrated that the difference between the superior and inferior corneal thickness as noted on ultrasonic pachymetry can be used to grade keratoconus. Pflugfelder et al13 found Orbscan (Bausch and Lomb, Rochester, NY, USA) pachymetry-based indices to be both sensitive and specific for diagnosing keratoconus. Li et al14 demonstrated that optical coherence tomography (OCT) pachymetry maps can detect the characteristic abnormal corneal thinning in keratoconic eyes in a manner as sensitive and specific as the keratometric KISA% index.
Therefore, these studies have suggested that pachymetric difference in normal and keratoconic corneas exist, and can be used (in automated systems like OCT and Orbscan) to diagnose keratoconus. However, it is not well established (a) whether a correlation exists between keratometric and pachymetric changes in the cornea, (b) whether there is a progressive association between these factors in the normal, keratoconus suspect and keratoconic cases from the same population, and (c) whether stringent criteria for multiple diagnostic cutoff can be established to create supplementary pachymetric criteria to add on to the currently existing keratometric classifications.
Materials and methods
This cross-sectional study was conducted at a tertiary care ophthalmic hospital and eye research center. Consecutive young myopic candidates presenting to our hospital for keratometric analysis were included in the study. The indications acceptable for inclusion in the study were: screening for lasik surgery, high astigmatism, frequent change of glasses, or a clinical diagnosis of keratoconus. Those with a history of any ocular surgery or any other ocular morbidity including poor ocular surface and dry eyes were excluded. Patients with secondary keratoconus and acute hydrops were excluded. All contact-lens wearers were asked to be off soft contact lenses for a minimum of 3 weeks and rigid gas-permeable lenses for a minimum of 5 weeks. If there was an evidence of corneal warpage on the Orbscan even after this waiting period, they were not included in the study. All the volunteers underwent three Orbscan anterior segment analysis (Orbscan IIz, Software version 3.14, Bausch and Lomb) scans with 15-min intervals between two scans using the Zyoptix mode. The acoustic factor was 0.94 and the default best-fit sphere was used. All the tests were performed between 1400 and 1700 hours to minimize the effect of diurnal variation. All tests were performed by a single experienced examiner (GK) and evaluated for satisfactory scanning by two different cornea specialists (GP, PD). All patients underwent the test on both eyes, after which one eye was randomly selected for the evaluation based on a computer-generated random number allocation chart.
The study was approved by the ethics committee of the hospital approved the study. All tenets of the Declaration of Helsinki were followed.
Statistical analysis
The data were entered on an Excel Sheet (Microsoft Inc., Redmond, WA, USA) and transferred to SPSS 16.0. (SPSS Inc., Chicago, IL, USA) for statistical analysis. Kruskal–Wallis test was used to analyze the overall difference of means and Mann–Whitney U-test was used for subsequent subgroup analysis. Regression models were computed to assess the correlation between multiple variables from corneal thickness and corneal keratometry. Stratification of the corneas was done using the Massachusetts Eye and Ear Infirmary criteria (MEEI criteria) and the KISA% index.2, 6
The differentiation between a keratoconus suspect and a keratoconic eye was done by the MEEI criteria, which uses both topographic and clinical criteria.6 The criteria include the following factors:
-
a)
Difference in keratometry with the fellow eye: <1.9, score 0; ≥1.9, score 1.
-
b)
Highest keratometry of the examined eye: <47.2, score 0; 47.3–48.7, score 1; ≥48.7, score 2.
-
c)
Difference in inferior and superior astigmatism: <1.4, score 0; 1.4–1.9, score 1; ≥1.9, score 2.
-
d)
≥2 findings on clinical examination: Atopy, Downs, family history of keratoconus or clinical signs of keratoconus (Fleisher, Vogt, Munson, nerves, scarring): No, score 0; Yes, score 2.
-
e)
Signs of corneal hydrops present, score 2; no, score 0.
In this index, a score of 0 was considered normal, a score of 1–3 was considered suspect, and a score of 4–9 was considered keratoconic.6 It may be noted that we excluded cases with acute hydrops and secondary keratoconus in the study.
The KISA% index was used as follows:2

where K is the K-value, an expression of central corneal steepening; the I–S value an expression of inferior–superior dioptric asymmetry; the AST index quantifies the degree of regular corneal astigmatism (Sim K1–Sim K2); and the skewed radial axis (SRAX) index an expression of irregular astigmatism occurring in keratoconic eyes. Further details on KISA% index are given in the study by Rabinowitz and Rasheed.2 In this index, an eye with a value between 60 and 100% is considered as a keratoconus suspect and that with a value >100% is considered as keratoconic.
Both indices, MEEI and KISA%, were applied to all patients. The higher of the two grades was used to label the eye as normal, a keratoconus suspect or keratoconic. ‘Normal’ were further divided into two subgroups: mean Orbscan simulated keratometry <44 D (flatter cornea) and mean Orbscan simulated keratometry ≥44 D (steeper cornea). Representative Orbscan outputs for these four groups are shown in Figures 1, 2, 3 and 4. The keratometric and pachymetric single maps are shown in Supplementary Figures 1a,b, 2a,b, 3a,b, and 4a,b.
A useful measure of the asymmetrical paracentral thinning seen in keratoconus is the difference between the central and the minimum corneal thickness (MCT). Therefore, the difference between the central and MCT was independently analyzed as a possible predictive factor in this study. Furthermore, in some advanced cases, because of a more generalized thinning of the cornea, the difference between central corneal thickness (CCT) and MCT can decrease in comparison with a more early case. Therefore, a new index was devised to measure the effect of eccentric thinning of the cornea over and above the generalized thinning. This index yields the difference between MCT and CCT as a percentage of the average of the MCT and CCT.

The mean and 2SD of the pachymetric values in the various keratometric classification groups were used to establish the diagnostic cutoff limits (<2.5% data outside the upper or lower limits as per the case).
Results
Demographics
In all, 566 male and 434 female patients participated in the study. The average age was 24.8±2.5 years.
Overall assessment of the data
The keratometric variables assessed were simulated keratometry (Sim K) astigmatism, mean Sim K, and overall maximum keratometry in the central 10-mm zone (the central 10 mm was included as some cases of keratoconus suspect have early topographic changes in the zone outside the keratometrically measured 3 mm). The pachymetric variables assessed were CCT, MCT, and numerical difference between CCT and MCT (δCT) .The mean, SD, and maximum and minimum values of the 1000 eyes are given in Supplementary Table 1.
Regression analysis
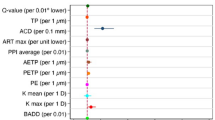
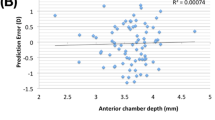
The pachymetric factors (CCT, MCT, δCT) were analysed to assess their predictive value for keratometric factors. Sim K astigmatism, mean Sim K, and overall maximum keratometry in the central 10-mm zone (Max Km10 mm) were found to be predicted using both the MCT and δCT (r2=0.14, P=1.9 × 10−32; r2=0.17, P=3.6 × 10−41; and r2=0.2, P=2.8 × 10−49, respectively). However, CCT did not have any additional statistically significant predictive impact on the keratometric parameters.
Best-fit curves
Best-fit curves were plotted to demonstrate the specific relationship between MCT and δCT and the three keratometric factors (Max Km10 mm, Sim K astigmatism, and mean SimK). Even though the linear fits were highly significant between these variables, MCT showed an additional quadratic fit primarily due to the rapid skewing of keratometric data in the suspect and keratoconic ranges (Supplementary Figures 5a–f).
Classification based on keratometry groups
Once it was established that MCT and δCT were correlated to the keratometry, the cases were divided as per the keratometric groups: flatter normal (n=219, 21.9%), steeper normal (n=611, 61.1%), keratoconus suspect (n=129, 12.9%), and keratoconus (n=41, 4.1%). CCT was also stratified according to keratometric groups, because many surgeons will not have access to a topographer (which measures MCT), and would use ultrasound pachymetry to evaluate CCT only. Mean pachymetric values for these groups were calculated.
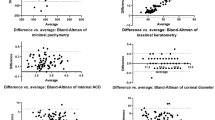
The mean CCT values were 554.7±39.1, 552.2±38.0, 538.6±47.0, and 472.4±73.2 μm for flatter normal, steeper normal, keratoconus suspect, and keratoconic eyes, respectively (P=2.3 × 10−12, Kruskal–Wallis test) (Supplementary Figure 6a). There was no statistical difference between the flatter and steeper normal corneas (P=0.3, Mann–Whitney U-test). The difference between the steep cornea and the keratoconus suspect groups was significant (P=0.004, Mann–Whitney U-test), as was the difference between the keratoconus suspect and keratoconus groups (P=4.1 × 10−7, Mann–Whitney U-test).
The mean MCT values were 542.5±39.6, 539.9±39.2, 524.2±49.5, and 449.3±73.7 μm for flatter normal, steeper normal, keratoconus suspect, and keratoconic eyes, respectively, (P=4.5 × 10−15, Kruskal–Wallis test) (Supplementary Figure 6b). There was no significant difference between the flatter and steeper normal corneas (P=0.3, Mann–Whitney U-test). However, there was a significant difference between the steep normal cornea and keratoconus suspect groups (P=0.002, Mann–Whitney U-test), and between the keratoconus suspect and keratoconus groups (P=7.1 × 10−9, Mann–Whitney U-test).
The mean differences between central corneal thickness and MCT (δCT) were 12.2±7.1, 12.4±7.4, 14.4±8.9, and 23.2±10.1 μm for flatter normal, steeper normal, keratoconus suspect, and keratoconic eyes, respectively (P=2.1 × 10−10, Kruskal–Wallis test) (Supplementary Figure 6c). There was a significant difference between the steeper normal and keratoconus suspect groups (P=0.014, Mann–Whitney U-test), and between the keratoconus suspect and keratoconus groups (P=1.9 × 10−6, Mann–Whitney U-test). However, there was no difference between the flatter and steeper normal groups (P=0.8, Mann–Whitney U-test).
The mean normalized pachymetric difference index values were 2.3±1.4 μ, 2.4±1.5 μ, 2.8±2.1 μ and 5.2±2.3 μ for flatter normal, steeper normal, keratoconus suspect, and keratoconic eyes, respectively (P=7.7 × 10−14, Kruskal–Wallis test). There was no difference between the flatter and steeper normal groups (P=0.7, Mann–Whitney U-test) (Supplementary Figure 6d). The difference between steep normal cornea and keratoconus suspect groups was significant (P=0.005, Mann–Whitney U-test), as was the difference between the keratoconus suspect and the keratoconus groups (P=1.2 × 10−8, Mann–Whitney U-test).
Diagnostic cutoffs
Mean and 2SD plots were drawn for the pachymetric criteria stratified above. Higher-specificity cutoffs were computed as follows: The lower tail (mean minus 2SD) cutoffs were used to establish the safe keratometric limits for CCT and MCT. The upper tail (mean plus 2SD) cutoffs were used to establish similar limits for the difference between central corneal thickness and MCT, and for the normalized pachymetric difference index.
Higher-sensitivity cutoffs were computed as follows: The lower tail (mean minus 1SD) cutoffs were used to establish the safe keratometric limits for CCT and MCT. The upper tail (mean plus 1SD) cutoffs were used to establish similar limits for the difference between central and MCT and for the normalized pachymetric difference index.
Table 1 shows the diagnostic cutoffs computed at the above-discussed levels.
Discussion
There have been many excellent studies on the keratometric stratification and classification of keratoconus.1, 2, 3, 4, 5, 6 However, there is paucity of similar gradation/cutoff criteria based on pachymetry. The aim of the current study was to evaluate if there is a correlation between thinning and corneal steeping, and if such a correlation exists, whether it can be used to establish additional cutoffs and criteria.
Regression analysis fits established that there is a correlation between the two sets of criteria in a varying fraction of the study population (approximately depending on the R2 fits).
One of the major indications of keratometric screening in normal population is screening for refractive surgery and therefore we used two existing criteria (MEEI and KISA%) used for lasik screening to stratify the data.2, 6 In our study, the subjects were young myopic refractive surgery candidates in a tertiary care eye center, which may not be representative of a population-based data. Therefore, we would suggest that the interpretation of the study be currently limited to cohorts similar to the one in the study.
Considering the fact that there was no difference in the pachymetric values of the two subgroups of keratometrically normal cornea, and there were significant differences when we compared the steep and the keratoconus suspect groups, our finding in a way validates the currently used keratometric cutoff for forme fruste keratoconus.
Once it was established that there are significant differences between the major three groups in the above-stated criteria, our primary aim was to establish high-specificity diagnostic cutoffs, to be used as adjuncts to the keratometry cutoffs. These high-specificity cutoffs were computed using 2SD differences as explained in the method above. Our findings suggest that a cornea having a MCT and CCT less than ∼461 and ∼476 μm, respectively, lies beyond the mean minus 2SD cutoff (97.5% data being more than this value, for a one-tailed assessment), and has only a 2.5% chance of being normal and not a keratoconus suspect or worse. Furthermore, a cornea having an MCT and CCT less than ∼444 and ∼425 μm, respectively, has only a 2.5% chance of being a keratoconus suspect and not a frank keratoconus. Therefore, refractive surgeons noting a similar or lower pachymetry in a patient should be very cautious in performing a weakening procedure like excimer laser ablation on such a cornea. This caution should be maintained even in the absence of any overt keratometric signs at the time of examination.
Difference in the CCT and MCT is also an important sign to be considered, as was proven by its association with the keratometric criteria independent of the MCT. The outcomes of the current study suggest that a cornea having a difference between CCT and MCT >27 μm lies beyond the mean plus 2SD cutoff (97.5% data being less than this value, for a one-tailed assessment), and has only a 2.5% chance of being normal and not a keratoconus suspect or worse. Furthermore, a cornea having a difference between CCT and MCT >32 μm has only a 2.5% chance of being a keratoconus suspect and not a frank keratoconus. For the normalized pachymetric difference index, a value of >5.1 should raise a similar suspicion for difference between normal and suspect, and a value of >7.1 is very likely to be associated with frank keratoconus and not keratoconus suspect.
This set of cutoffs can also be used to monitor the progression from keratoconus suspect status, which has traditionally been done by only keratometric changes. For example, suppose that the mean K of a suspect changes from 48.5 to 48.8 D; however, the MCT worsens from 460 to 420 μm. The minimal change in the mean K would be possible false reassurance, in spite of a progressive pathology. The use of these parameters could be useful to quantify such a change.
Many ophthalmologists, especially those without a topographic/keratometric facility available to them, shall be more comfortable with a more sensitive criterion for pachymetry. Thus, we have added additional criteria (∼16% based on 1SD cutoff compared with 2.5% based on 2SD cutoff) to aid in such a situation (Table 1). These more sensitive criteria would have a higher false-positive rate compared with the more specific criteria, and may be useful as an initial screening test. Therefore, a general ophthalmologist or a non-refractive subspecialist who does not have an advanced keratometric test available but would not like to miss a case of forme fruste or subclinical keratoconus incidentally coming to them would like to use the sensitive cutoffs based on 1SD (Table 1).
Further prospective studies on the longitudinal behavior of keratoconus incorporating both keratometric and pachymetric criteria may establish further safety checks like the current study does for diagnostic screening.
In conclusion, the current study suggests that pachymetric diagnostic cutoffs can be used as adjuncts to the existing keratometric criteria to screen keratoconus suspects and keratoconic patients presenting for refractive surgery. However, the above-mentioned criteria should not be used as a replacement for the keratometric criteria.

References
Rabinowitz YS . Keratoconus. Surv Ophthalmol 1998; 42 (4): 297–319.
Rabinowitz YS, Rasheed K . KISA% index: a quantitative videokeratography algorithm embodying minimal keratometric criteria for diagnosing keratoconus. J Cataract Refract Surg 1999; 25 (10): 1327–1335.
Dastjerdi MH, Hashemi H . A quantitative corneal topography index for detection of keratoconus. J Refract Surg 1998; 14 (4): 427–436.
Smolek MK, Klyce SD . Current keratoconus detection methods compared with a neural network approach. Invest Ophthalmol Vis Sci 1997; 38 (11): 2290–2299.
Maeda N, Klyce SD, Smolek MK . Comparison of methods for detecting keratoconus using videokeratography. Arch Ophthalmol 1995; 113 (7): 870–874.
Melki SA, Azar DT . LASIK complications: etiology, management, and prevention. Surv Ophthalmol 2001; 46: 95–116.
Alió JL, Piñero DP, Alesón A, Teus MA, Barraquer RI, Murta J et al. Keratoconus-integrated characterization considering anterior corneal aberrations, internal astigmatism, and corneal biomechanics. J Cataract Refract Surg 2011; 37 (3): 552–568.
Piñero DP, Alio JL, Barraquer RI, Michael R, Jiménez R . Corneal biomechanics, refraction, and corneal aberrometry in keratoconus: an integrated study. Invest Ophthalmol Vis Sci 2010; 51 (4): 1948–1955.
McMahon TT, Szczotka-Flynn L, Barr JT, Anderson RJ, Slaughter ME, Lass JH et al. CLEK Study Group. A new method for grading the severity of keratoconus: the Keratoconus Severity Score (KSS). Cornea 2006; 25 (7): 794–800.
Alió JL, Shabayek MH . Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg 2006; 22 (6): 539–545.
Rabinowitz YS, Rasheed K, Yang H, Elashoff J . Accuracy of ultrasonic pachymetry and videokeratography in detecting keratoconus. J Cataract Refract Surg 1998; 24 (2): 196–201.
Watters GA, Owens H . Evaluation of mild, moderate, and advanced keratoconus using ultrasound pachometry and the EyeSys videokeratoscope. Optom Vis Sci 1998; 75 (9): 640–646.
Pflugfelder SC, Liu Z, Feuer W, Verm A . Corneal thickness indices discriminate between keratoconus and contact lens-induced corneal thinning. Ophthalmology 2002; 109 (12): 2336–2341.
Li Y, Meisler DM, Tang M, Lu AT, Thakrar V, Reiser BJ et al. Keratoconus diagnosis with optical coherence tomography pachymetry mapping. Ophthalmology 2008; 115 (12): 2159–2166.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Prakash, G., Agarwal, A., Mazhari, A. et al. A new, pachymetry-based approach for diagnostic cutoffs for normal, suspect and keratoconic cornea. Eye 26, 650–657 (2012). https://doi.org/10.1038/eye.2011.365
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.365