Abstract
Purpose
To report and to analyze the efficacy of horizontal rectus muscle transposition and inferior oblique muscle weakening in terms of pattern correction for patients with V pattern.
Methods
The review of the medical files identified 55 patients who had esotropia (ET) or exotropia (XT) with V pattern. The primary outcome measure was the amount of V pattern collapse (Δ).
Results
Of the 55 patients (mean age 22.1±9.5 years), 27 (49.1%) were males and 28 (50.9%) were females. The type of deviations was XT in 30 patients (54.5%) and ET in 25 patients (45.5%). Inferior oblique muscle weakening was performed in 43 (78.2%) patients, whereas horizontal muscle transposition was carried out in 12 (21.8%) patients in addition to recession-resection procedures. The amount of pattern was significantly reduced in both groups (P=0.01 for the horizontal offset group and P<0.01 for the oblique muscle weakening group).
Conclusion
Oblique muscle weakening surgery and horizontal muscle offset are effective in the correction of V pattern when the amount of pattern is under 30Δ.
Similar content being viewed by others
Introduction
The amount of deviation in strabismic patients may change in upgaze and downgaze apart from straight ahead primary position and may increase or decrease in regard with coexistent strabismus type. This difference has been named as A and V patterns.1 The A-pattern has been described when the difference of horizontal deviation between upgaze and downgaze is more than 10Δ, and V pattern has been described when this difference is more than 15Δ.2 The overall reported prevalence of patterns in strabismic patients ranges between 12.5 and 87.7% in different studies.2, 3, 4 Many theories have been suggested to clarify the aetiology of patterns consisting of orbital factors such as craniofacial anomalies or heterotopia of muscle pulleys, anomalies of extraocular muscles, and disruption of fusion.2, 5, 6, 7 The generally accepted surgical correction of patterns includes oblique muscle weakening when there is evident oblique muscle overaction, and horizontal muscle transposition when there is not. However, both procedures may be performed together in cases with large patterns.
Many surgical attempts have been made in order to reduce the amount of patterns by weakening the inferior oblique muscle such as inferior oblique graded anteriorization, recession8, 9 or by changing the insertion of horizontal muscles.10, 11, 12
In the present study, we aimed to report the clinical features of V pattern, its surgical management in our clinic and to report the outcomes of horizontal rectus muscle transposition and oblique muscle weakening surgery in regard with the collapse of the V pattern.
Materials and methods
A retrospective review of the medical files of patients who underwent strabismus surgery for the correction of V pattern was carried out in Strabismus Unit upon approval of Institutional Ethics Committee. The study followed the tenets of the Declaration of Helsinki. The data included the type and amount of deviation and pattern, and the type of surgery and its outcomes. Among patients who underwent surgery, only ones who had postoperative follow-up visit at 3 months after the surgery were eligible for the study. Furthermore, patients who had previous surgeries and dissociated vertical deviations were all excluded.
All patients underwent a complete orthoptic evaluation including the measurement of deviation in primary position, in upgaze and downgaze with prism cover test (Δ). Oblique overaction was graded between +1 to +4. Oblique muscle surgery was preferred for patients who had equal or more than +2 overaction of inferior oblique muscle. The type of surgery for the correction of V pattern was noted. Patients who underwent horizontal muscle vertical offset were considered as group 1, whereas patients who underwent inferior oblique muscle weakening were categorized in group 2. The amount of horizontal muscle offset was half tendon width for all patients in group 1. Tenotomy was the most common procedure for inferior oblique weakening.13, 14 Inferior oblique muscle anterotransposition was graded according to the amount of inferior oblique muscle overaction. Myectomy was preferred when inferior oblique muscle overaction was +4. All patients underwent simultaneous recession-resection procedure in order to correct the horizontal deviation in primary position as well.
SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistics. P-value under 0.05 was considered as significant. Independent samples t-test, Mann-Whitney U-test, Wilcoxon test and Pearson chi-square test were performed for the analysis.
Results
The retrospective analysis identified a total of 55 patients with a mean age of 22.1±9.5 years. Of the 55 patients, 27 (49.1%) were males (mean age 20.3±7.6 years) and 28 (50.9%) were females (mean age 23.5±10.7 years) (P=0.23). Thirty patients (54.5%) had exodrift, whereas 25 patients (45.5%) had esodrift. None of the patients had associated systemic or neurological disorders.
Among 55 patients, 43 (78.2%) underwent inferior oblique muscle surgery and 12 (21.8%) had horizontal muscle transposition for the correction of V pattern.
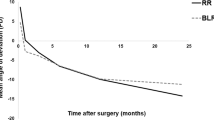
The most common inferior oblique weakening procedure was tenotomy in 32 patients (74.4%), followed by inferior oblique anteriorization in 10 patients (23.25%) and inferior oblique myectomy in 1 patient (2.34%). There was no statistically significant difference between three types of inferior oblique weakening surgery in terms of pattern correction (P=0.45). The comparison of preoperative and postoperative amount of horizontal deviations and pattern correction is described in detail in Table 1. There was no statistical difference of preoperative amount of horizontal near and distance deviation between two types of surgical procedures (P=0.79 and P=0.66, respectively). The analysis of postoperative near and distance deviations revealed no significant difference as well among two groups (P=0.22 and P=0.77 respectively). The median amount of pattern correction was similar in group 1 and 2 (P=0.34). There was no significant difference of V pattern collapse among patients with eso- or exodeviations (P>0.05).
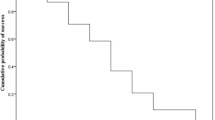
V pattern collapse was obtained in 66.7% of patients in group 1 (N=8) and in 86.1% of patients (N=37) in group 2, and 10 patients (18.1%) required further surgery in order to correct the residual pattern.
Discussion
The alphabetical patterns should be recognized in patients with strabismus because they may lead over- or undercorrections when left undiagnosed. The recognition of the pattern does not only cause a change in the surgical plan but also prevents unnecessary surgeries and disappointing surgical outcomes. Since there is a general preference of surgical management as ‘oblique muscle surgery for patients with noticeable oblique muscle overaction and horizontal muscle transposition for whom who don’t have’, we aimed with the present study to report our surgical experience in patients with V pattern and to analyze the outcomes of inferior oblique muscle weakening and horizontal muscle vertical offset.
There are several studies reporting the clinical features of patients with pattern strabismus. Dickmann et al15 evaluated the prevalence of neurological and/or systemic problems associated with A and V patterns comparing with a control group of patients who had concomitant strabismus without patterns. They detected that neurological and systemic abnormalities were significantly more frequent in strabismic patients with patterns. In the present study, none of the patients with V pattern had associated neurological problems.
Many surgical attempts have been made in order to weaken the inferior oblique muscle force in V pattern. Akar et al8 investigated that the effect of bilateral graded anterotransposition of inferior oblique muscle in a study population of 69 patients with V pattern and concluded that this technique was succesful in correction of the pattern. Kumar et al9 reported that hang back recession is a preferrable technique that may offer further adjustment. In the present study, the most preferred technique was inferior oblique tenotomy, and the efficacies of three techniques were found to be similar. However, it should be kept in mind that the number of patients was not equal in three groups of surgery.
Dickmann et al10 evaluated the dose-response relation of vertical displacement in bilateral medial rectus recessions in pattern strabismus. They found that there was an increased relationship particularly in A pattern. In the present study, we found that horizontal muscle half tendon width transposition did significantly decrease the amount of V pattern.
Mostafa et al11 compared the outcomes of bilateral medial rectus slanting recession with half tendon width downward transposition in V pattern esotropia. They showed that both procedures were equally effective without significant difference in reducing the amount of pattern as well as manifest deviation in primary position. They found that the transposition provides the collapse of V pattern of 22Δ, whereas it was almost 14Δ in our study.
Oya et al12 found that horizontal muscle full tendon vertical offsets in V pattern exotropia without oblique muscle dysfunction corrected the pattern significantly in their retrospective series of 11 patients. In the present study, patients with V pattern who underwent vertical offset of horizontal muscles had significant reduction in the amount of pattern almost as much as whom who had oblique muscle surgeries.
Sharma et al16 compared the effects of 8 mm offset with 5 mm offset and determined that two techniques had similar success in terms of vertical incomitance, although the former caused more horizontal incomitance. In the present study, all patients in group 1 underwent a 5 mm vertical offset.
Ten patients underwent further surgery for the correction of residual pattern. The choice for the second procedure was made in regard with the primary surgery and the presence of inferior oblique muscle overaction. The reasons for the surgical failure might be overlooked inferior oblique overaction, the factors related to the surgical technique, or underestimation of the magnitude of the pattern preoperatively.
The present study should be reviewed in the context of some limitations. This study may bring all the disadvantages related to retrospective studies. The results reflect the surgical preference of a single centre, although a diversity of surgical techniques exists among strabismus surgeons in terms of pattern correction. The amount of torsion induced by horizontal muscle transposition or oblique muscle weakening was not evaluated, but it might be a valuable data that might change the surgical plans. There might be a selection bias regarding patients who had equal or more than +2 inferior oblique underwent inferior oblique muscle weakening. The amounts of recession or resection were variable. The results of the present study cannot be extrapolated to all patients with V pattern. The number of patients in group 1 was smaller compared to group 2 and this may influence the comparison. Larger groups may yield different outcomes. The lack of the data regarding the underlying aetilogy of the pattern including the insertional characteristics of the extraocular muscles, orbital factors, and anatomical features highlighted by orbital imaging is another limitation of the study. Further larger prospective randomized studies are needed in order to emphasize the mentioned limitations.
In conclusion, patterns seemed to be corrected whether by horizontal muscle vertical transposition or oblique muscle surgery, particularly when the amount of pattern is under 30Δ, as long as the preoperative orthoptic evaluation is accurate and the presence of a pattern is recognized, but the possibility of further surgery should be borne in mind.

References
Albert DG . Personal communication. In Parks MM: Annual review: Strabismus. Arch Ophthalmol 1957; 152: 58.
Knapp P . A and V patterns. In: Symposium on Strabismus. Transactions of the New Orleans Academy of Ophthalmology. Mosby-Year Book: St Louis, MO, USA, 1971 p 242.
von Noorden GK, Campos EC . A and V patterns. In: Lampert R, Cox K, Burke D (eds). Binocular vision and ocular motility: theory and management of strabismus 6th edn Mosby, Inc.: St Louis, MO, USA, 2002 pp 396–413.
Maggi C . Sendromi A V e oftalmoplegie congenite. Boll Ocul 1963; 42: 354.
Urist MJ . The etiology of the so-called A and V syndromes. Am J Ophthalmol 1958; 46: 835–844.
Clark RA, Miller JM, Rosenbaum AL, Demer JL . Heterotopic muscle pulleys or oblique muscle dysfunction? J AAPOS 1998; 2: 17–25.
Kushner BJ . Effect of ocular torsion on A and V patterns and apparent oblique muscle overaction. Arch Ophthalmol 2010; 128: 712–718.
Akar S, Gokyigit B, Yılmaz OF . Graded anterior transposition of the inferior oblique muscle for V-pattern strabismus. J AAPOS 2012; 16: 286–290.
Kumar K, Prasad HN, Monga S, Bhola R . Hang-back recession of inferior oblique muscle in V-pattern strabismus with inferior oblique overaction. J AAPOS 2008; 12: 401–404.
Dickmann A, Petroni S, Salerni A, Parrilla R, Savino G, Battendieri R et al. Effect of vertical transposition of the medial rectus muscle on primary position alignment in infantile esotropia with A- or V-pattern strabismus. J AAPOS 2011; 15: 14–16.
Mostafa AM, Kassem RR . A comparative study of medial rectus slanting recession versus recession with downward transposition for correction of V-pattern esotropia. J AAPOS 2010; 14: 127–131.
Oya Y, Yagasaki T, Maeda M, Tsukui M, Ichikawa K . Effects of vertical offsets of the horizontal rectus muscles in V-pattern exotropia without oblique dysfunction. J AAPOS 2009; 13: 575–577.
Dyer JA . Tenotomy of the inferior oblique muscle at its scleral insertion. An easy and effective procedure. Arch Ophthalmol 1962; 68: 176–181.
Jones TW Jr, Lee DA, Dyer JA . Inferior oblique surgery. Experience at the Mayo Clinic from 1960 to 1981. Arch Ophthalmol 1984; 102: 714–716.
Dickmann A, Parrilla R, Aliberti S, Perrotta V, Salerni A, Savino G et al. Prevalence of neurological involvement and malformative/systemic syndromes in A- and V-pattern strabismus. Ophthalmic Epidemiol 2012; 19: 302–305.
Sharma P, Halder M, Prakash P . Effect of monocular vertical displacement of horizontal recti in A V phenomena. Indian J Ophthalmol 1995; 43: 9–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The study was conducted in Hacettepe University Faculty of Medicine, Department of Ophthalmology, Ankara, Turkey. The material was partially presented in the Turkish National Congress of Ophtalmology, 17-21 October 2012, Antalya, Turkey.
Rights and permissions
About this article
Cite this article
Sekeroglu, H., Turan, K., Uzun, S. et al. Horizontal muscle transposition or oblique muscle weakening for the correction of V pattern?. Eye 28, 553–556 (2014). https://doi.org/10.1038/eye.2014.16
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.16