Abstract
Purpose
To report the outcomes and surgical difficulties during rhegmatogenous retinal detachment (RRD) repair in patients with albinism.
Methods
Retrospective analysis of 10 eyes of 9 patients with albinism that underwent RRD repair was performed. Collected data included demographic details, preoperative examination details, surgical procedure, surgical difficulties, anatomical, and visual outcomes. Outcome measures were retinal reattachment and visual acuity at the last follow-up.
Results
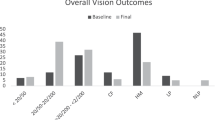
Mean preoperative best-corrected visual acuity (BCVA) was logMAR (Logarithm of the Minimum Angle of Resolution) 2.15 (range 0.9–3.0) with preoperative localization of causative break in six eyes. One eye had proliferative vitreoretinopathy grade C1 preoperatively. Four eyes underwent scleral buckling (SB) and six underwent 20G pars plana vitrectomy (PPV) with silicone oil injection. Intraoperative complication as iatrogenic retinal break occurred in four eyes. For retinopexy during vitrectomy, endolaser delivery was possible in three out of six eyes, whereas three eyes had cryopexy. The mean follow-up was 12 months in SB group (range 1–12; median 12 months) and 5.33 months (range 1–12; median 3 months) in PPV group. Among vitrectomized eye, two eyes had recurrence at 3 months with oil in situ. Rest of the eyes had attached retina at last follow-up. Mean BCVA at last follow-up was logMAR −1.46 (range 0.7–2.0) with mean improvement of −0.57 logMAR.
Conclusions
Identification of break, induction of posterior vitreous detachment, and endolaser delivery may be difficult during RRD repair in patients with albinism. The incidence of PVR appeared less in these eyes. Both SB and PPV were efficacious and appear to be good surgical techniques for use in this patient population.
Similar content being viewed by others

Introduction
Subjects with oculocutaneous albinism and ocular albinism are often encountered in ophthalmology as having low vision, nystagmus, and glare that needs management in a low vision clinic and sometimes in the strabismus services. Because of lack of pigments especially in iris and choroid, diagnosis and surgical interventions of posterior segment diseases could be challenging. However, challenges and outcomes of various intraocular surgeries on such eyes are rarely reported.
Rhegmatogenous retinal detachment (RRD) in albinism is infrequently reported, only as isolated cases.1, 2 It has been reported that visualization of retinal breaks could be challenging as the contrast between retina and choroid would be poor. Trypan blue dye has been used to improve contrast and localize retinal breaks during surgery.3 Other intraoperative difficulties could be application of endolaser in presence of proliferative diabetic retinopathy and RRD in patients with albinism.1, 4 The efficacy of creating chorioretinal adhesions in eyes that lack pigment would be difficulty, as most techniques using laser or crypopexy are dependent on uptake by the pigment in the retinal pigment epithelium or choroid.
Our study aims to identify retinal detachment characteristics, outcomes, and intraoperative difficulties of retinal detachment surgery in patients with albinism.
Materials and methods
A retrospective chart review of consecutive patients with ocular or oculocutanous albinism who underwent retinal detachment repair, between January 1986 and March 2012 at L V Prasad Eye Institute, Hyderabad, India, was performed. Prior approval was obtained from the Institutional Review Board and informed consent was obtained from each subject for diagnostic and therapeutic procedures.
Data retrieved included demographics, details of the ocular and systemic exam, surgical details including complications and difficulties, and the final outcome. The best-corrected visual acuity (BCVA) was assessed using Snellen’s chart and was converted to logMAR (Logarithm of the Minimum Angle of Resolution) for statistical analysis. All participants underwent a comprehensive ocular examination, including dilated fundus examination with slit-lamp biomicroscopy at baseline, at 1 month and as per physician’s discretion during follow-up visits.
Surgical procedure
Pars plana vitrectomy
20G Vitrectomy was performed using the Alcon Accurus platform and instrument packs (Alcon Inc., Fort Worth, TX, USA). A 360° encircling buckle (#240; MIRA Inc., Uxbridge, MA, USA) was placed in all cases. The cutter had a maximum speed of 2500 cuts per minute. All cases were performed either using the BIOM wide-angle viewing system or hand-held wide-angle contact lens. In one case, triamcinolone acetonide was used to visualize the vitreous and in another case, Trypan blue was used to localize the break using dye diffusion technique. Internal drainage was performed in all cases through a posterior retinotomy over the detached retina, and after fluid–air exchange, laser photocoagulation was performed around all the breaks. Transcleral cryotherapy was performed if the laser photocoagulation was not satisfactory. Silicone oil injection was performed through the infusion cannula in the viscous fluid control mode, with a pressure of 50 mm Hg. All cases were checked for wound leak at the end of the surgery.
Scleral buckling
After 360° conjunctival opening, all 4 recti were tagged with 4-0 silk suture. Breaks were localized using indirect ophthalmoscope and cryotherapy was performed. Scleral buckles, size per physician’s discretion, were passed through preplaced 5-0 polyester (Dacron) suture (MIRA Inc.). Encirclage (band # 240) was placed over the buckle through partial thickness scleral tunnels. None of the eyes underwent external drainage of the subretinal fluid. Retinal examination was performed at the end of the surgery to rule out any intraoperative complications.
Intraoperative difficulties including visualization of detached retina, identification of breaks, and endolaser application were noted from the surgical notes.
Results
A total of 807 patients with oculocutaneous and ocular albinism presented to our institution from January 1986 to March 2012. Out of these, 11 eyes of 9 patients were found to have RRD. One patient who had bilateral involvement decided to undergo retinal detachment repair only in one eye. Therefore, 10 eyes of 9 patients with RRD who underwent retinal detachment repair surgery were included in the present study. The baseline characteristics, operative procedure, and postoperative finding are given in Table 1. The primary surgery included scleral buckling (SB) using transscleral cryopexy and explants in four eyes and vitrectomy procedures with silicone oil tamponade (PPV) in six eyes. The mean duration of follow-up was 12 months in SB group (range 1–12; median 12 months) and 5.33 months (range 1–12; median 3 months) in PPV group. Preoperatively, the break could be localized in six eyes (60%). PVR grade C1 was present in only one eye (10%) in a patient, who underwent SB procedure. Iatrogenic break occurred in four of the six eyes (66.66%) due to inadvertent cutting of the mobile retina by the vitrectomy cutter because of poor contrast of retinal tissue during vitrectomy. Endolaser delivery was successfully visualized and completed in three out of six PPV eyes (50%), whereas three eyes needed cryopexy owing to the failure in detecting the laser reaction. All the surgeons mentioned difficulty in visualizing the tissues while doing PPV surgery as they experienced significant glare back from the albinotic tissues, which made the surgery difficult to perform.
At the end of the follow-up, all eyes in the SB group had complete retinal reattachment and no recurrences or complications. The retina was reattached in four out of six eyes in PPV group. In one PPV case, there was persistence of inferior shallow subretinal fluid under silicone oil with attached macula was noted, for which the patient and the surgeon opted for observation till the last follow-up. In the other case, recurrence inferiorly with attached macula was noted at 5 months postoperatively. In this eye, the primary RRD repair was done for a posterior break, following globe perforation during peribulbar anesthesia for cataract surgery. Resurgery with silicone oil exchange failed to reattach the inferior retina completely and further surgery was not considered because of poor prognosis.
Mean BCVA change in study eyes improved from preoperative logMAR 2.15 (Snellen’s equivalent 20/2825, approximately counting fingers close to face) to logMAR 1.24 (Snellen’s equivalent 20/350). In SB group, mean BCVA improved from preoperative logMAR 1.59 (Snellen’s equivalent 20/800; range 0.9–2.69) to logMAR 0.97 (Snellen’s equivalent 20/160; range 0.69–1.0). In PPV group, mean BCVA improved from preoperative logMAR 2.63 (Snellen’s equivalent 20/8000, approximately hand motions; range 2.3–3.5) to 1.35 (Snellen’s equivalent 20/400; range −0.77 to 2.3). The fellow eyes also had low vision in all cases and till last follow-up examination, none of the fellow eyes developed retinal detachment.
Discussion
Our large database of ocular and oculocutaneous albinism shows that RRDs are quite uncommon in such patients, with prevalence of ~1.2% (10 out of 807 patients) noted in our tertiary care center. The lack of significant reports in literature supports the less prevalence of this condition. Although the condition is associated with significant myopia, the retinal detachment rates are low. Except for isolated case reports, there is no comprehensive case series of this rare clinical situation in the literature. Our case series can give some insight into the difficulties and outcomes in the management of RRD in albinism.
The identification of retinal breaks both preoperatively and intraoperatively appears as the first challenging task. Hiroshi et al5 reported difficulty in finding a hole because of ‘red fundus’ in albinism with RRD. We could detect breaks in 6 out of 10 eyes (60%) preoperatively and in the rest of the four eyes, break was detected intraoperatively. However, this was with difficulty and took time as per surgical notes. Whether any tiny breaks were missed in the two failed surgical cases, was not possible to ascertain due to poor contrast. Various techniques of break detection such as subretinal trypan blue injection has been reported.3 In one of our case, subretinal trypan blue was used to localize the break.
The lack of pigment causing difficulties with efficient visualization of laser burns and lack of ‘coagulation and adhesive’ effect could be one of the main theoretical difficulties. The effect of photocoagulation uptake in albinotic fundus is variable in the few reports available.4 In a case report by Yang et al,2 in a 44-year-old man undergoing vitrectomy for RRD in an albinotic eye, cryopexy was needed as laser burns could not be achieved. Recently, Huang et al suggested that initially argon yellow laser at high powers and increased duration could be attempted so as to coagulate hemoglobin within the choriocapillaries and indirectly lead to retinal adhesion effect in eyes with oculocutaneous albinism. Endocryopexy or transscleral cryopexy was suggested as a secondary step if laser uptake was not visualized.1 Hiroshi et al5 were able to get adequate krypton red laser burns and achieve reattachment. In our study, it was possible to get visible 532 green argon laser in three out of six eyes using power of 200–400 MW and duration of 150–300 ms. Rest of the three eyes undergoing PPV, visible laser marks could not be achieved even after increasing the power and duration of laser, and hence cryopexy was needed.
Duration >6 months is considered as one of the poor prognostic factor in rhegmatogenous retinal detachment in normal eyes. In our series, out of four eyes with more than 6 months duration of retinal detachment, three eyes had successful anatomical outcome. The severity of the PVR was almost same in both the groups, with only one eye with PVR C1 underwent buckling procedure.
The risk of PVR in eyes with albinism is unknown. It was interesting that although 5 out of the 10 eyes presented beyond 3 months of onset of symptoms of RRD, only one eye showed the presence of early PVR preoperatively. It could be that lack of pigmented cells causes reduced incidence of PVR in albinism-associated clinical RRD. Experimental PVR in albinotic rabbits is reported to be significantly less after intravitreal injection of human platelet-rich plasma.6 In our study, only one eye with post-iatrogenic needle injury and RRD developed recurrent PVR and failed to reattach completely.
Iatrogenic breaks were common during PPV (in 66.6%) in albinotic fundus due to lack of contrast between the retina and choroid, and also because of the ‘red fundus’ appearance. Difficulty, if any, in occurrence or creation of PVD in such eyes is not reported in the literature, however, occurrence of breaks suggests difficulty in OVD induction. Although it was difficult to get good contrast between the retina and choroid, however, it was possible to identify the causative break intraoperatively in three of six vitrectomy cases. In our series, in one case, triamcinolone acetonide was used to visualize the vitreous. Silicone oil was used in all of the vitrectomy cases for internal tamponade. From the surgeons’ perspective, the significant glare and ‘bright red reflex’ back from the tissues made visualization of tissues difficult in all cases, but especially so while performing vitrectomy, where one is used to not ‘seeing’ the iris or choroidal vasculature during surgery. None of the successfully reattached eyes developed any postoperative complications such as hypotony or glaucoma.
Our results regarding attachment of posterior pole at the end of 3 months as 100% assures us that even with difficulties before and during surgery for RRD in albonotic eyes, it is possible to get satisfactory anatomical outcome. The anatomical outcomes were comparable to a large study with various grades of PVR (71%) in normal eyes with RRD done at our center.7 As most eyes with albinism may not have normal visual acuity due to nystagmus and foveal hypoplasia,8 comparison with visual outcomes with non-albinotic cases would be irrelevant. At the last follow-up, all eyes showed improvement or stabilization of vision.
Limitations of the study include small sample size and retrospective nature. Three patients had only 1 month follow-up, therefore the mean follow-up was only 7 months. We are unable to comment on the surgical outcomes in albinism using advanced surgical instrumentation in present ‘modern vitrectomy’ era. Future study with larger sample size and longer follow-up, using recent vitrectomy instrumentation, may provide robust evidence.
In conclusion, identifying break and endolaser delivery may be difficult in RRD in albinism. Inadvertent damage to retina due to lack of contrast could be common intraoperative complication. The incidence of PVR appeared less in these eyes with good anatomical success. Both SB and PPV were efficacious and appear to be good surgical techniques for use in this patient population.

References
Huang XY, Wang Y, Wang R, He GG, Gabrielian A, MacCumber MW . Diagnostic and therapeutic challenges. Retina 2012; 32 (2): 399–402.
Yang JW LS, Kang SB, Park YH . A case of retinal detachment surgery in albinism patient. J Korean Ophthalmol Soc 2008; 49 (5): 840–844.
Jackson TL, Kwan AS, Laidlaw AH, Aylward W . Identification of retinal breaks using subretinal trypan blue injection. Ophthalmology 2007; 114 (3): 587–590.
Hanson RJ, Rubinstein A, Bates RA . Therapeutic challenges in the management of proliferative diabetic retinopathy in oculo-cutaneous albinism. Invest Ophthal Vis Sci 2005; 46: 346.
Hiroshi MHM . A case of ocular albinism with rhegmatogenous retinal detachment. Japanese Rev Clin Ophthalmol 1999; 93 (6): 861–864.
Baudouin C, Khosravi E, Pisella PJ, Ettaiche M, Elena PP . Inflammation measurement and immunocharacterization of cell proliferation in an experimental model of proliferative vitreoretinopathy. Ophthalmic Res 1998; 30 (6): 340–350.
Jalali S, Yorston D, Shah NJ, Das T, Majji AB, Hussain N et al. Retinal detachment in south India-presentation and treatment outcomes. Graefes Arch Clin Exp Ophthalmol 2005; 243 (8): 748–753.
Dijkstal JM, Cooley SS, Holleschau AM, King RA, Summers CG . Change in visual acuity in albinism in the early school years. J Pediatr Ophthalmol Strabismus 2012; 49 (2): 81–86; quiz 87.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sinha, M., Chhablani, J., Shah, B. et al. Surgical challenges and outcomes of rhegmatogenous retinal detachment in albinism. Eye 30, 422–425 (2016). https://doi.org/10.1038/eye.2015.245
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.245
This article is cited by
-
Long-term anatomical and functional findings of solar maculopathy
Irish Journal of Medical Science (1971 -) (2024)