Abstract
Purpose
To evaluate the baseline and post-vitrectomy lens densitometry values by a Scheimpflug camera in eyes with epiretinal membrane that were treated with 27-G microincision vitrectomy surgery (MIVS) without tamponade and to compare the results with those in fellow healthy eyes.
Patients and methods
Prospective case series. The lens densitometry measurements of 24 patients, who underwent 27-G MIVS without any tamponade for the treatment of epiretinal membrane, were taken preoperatively and on the first week, first month, and third month postoperatively with Pentacam HR-Scheimpflug imaging system.
Results
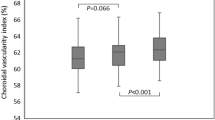
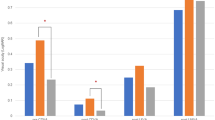
The mean lens densitometry values at Zone 1 and average lens densitometry values significantly increased in the study eyes on the first month when compared with the preoperative values (P=0.011, P=0.033, respectively). Additionally, there were statistically significant differences regarding the mean lens densitometry values of Zone 1 and Zone 2, and also average lens densitometry values between the preoperative and third month postoperative values (P=0.003, P=0.021, P=0.009, respectively). However, the densitometry values of fellow eyes were similar at preoperatively and all the postoperative follow-up periods (P>0.05 for all).
Conclusions
This study suggests that 27-G MIVS might cause post-surgical lens density changes even in early postoperative months and vitreous may play an important role in protecting the transparency of the lens.
Similar content being viewed by others
Introduction
In the present day, microincision vitrectomy surgery (MIVS) with 23-gauge (G) and 25-G instrumentation is mostly used instead of traditional 20-G pars plana vitrectomy (PPV). Additionally, in 2010, Oshima et al1 firstly described the initial feasibility and safety of a novel 27-G instrument system, reporting excellent visual and anatomic outcomes. It has been well documented in the literature that utilization of smaller-diameter instruments with self-sealing, transconjunctival scleral wounds provide some advantages such as decreased postoperative pain and inflammation, decreased induced astigmatism, and improved patient comfort.2, 3, 4, 5 On the other hand, despite these improvements, some complications are still available following PPV in which cataract development or acceleration is one of the most common.
Vitrectomy-related cataractogenesis is commonly reported following 20-G PPV with an incidence rate varying from 12.5 to 80%.6, 7, 8 It was reported that 23-G and 25-G MIVS systems are potentially less risky than standard 20-G PPV system since the reduced balanced solution consumption, lower intravitreal fluid flow, decreased surgical time, and ocular manipulations.9, 10 The cataract rates in most of these aforementioned studies rely on the data of clinical examinations, not quantitative analyses.
A quantitative analysis of lens transparency is crucial to objectively determinate the effect of risk factors for cataractogenesis and to document the progression of cataract level during the follow-up period. The optimal system to determinate the lens transparency must be objective and reproducible. Recent developments of the Scheimpflug topography systems have enabled quantitative measurements of the lens transparency. The Pentacam HR (Oculus, Wetzlar, Germany) that uses a rotating Scheimpflug camera to image the anterior ocular segment from the anterior corneal surface to the posterior lens surface provides anterior and posterior corneal topography and three-dimension anterior chamber analysis.11, 12, 13 It can also provide precise and reproducible data related to lens densitometry, that is a quantitative and objective method to assess the lens transparency.14, 15 The Pentacam HR reveals a three-dimension image of the crystalline lens and a measurement of the lens density in the chosen area, that ranges from 0 (no lens clouding-completely clear) to 100 (completely opaque). This system also has high intra-observer and inter-observer repeatability rates in eyes with and without cataract.15, 16, 17
In this study, we aimed to evaluate the baseline and post-vitrectomy lens densitometry values in eyes with epiretinal membrane that were treated with 27-G MIVS without tamponade, and to compare the results with those in fellow healthy eyes.
Patients and methods
Study design and patient selection
This prospective longitudinal study was performed at the retina unit of Ulucanlar Eye Training and Research Hospital from January 2015 to February 2016. The study protocol was approved by Ankara Numune Training and Research Hospital and the study was carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from each individual participant.
Twenty-four patients who underwent 27-G MIVS without any tamponade for the treatment of epiretinal membrane were enrolled. To be included in the study, each subject was required to meet all the following criteria: fundoscopic and optical coherence tomographic proven epiretinal membrane, the best corrected visual acuity (BCVA) was equal or less than 0.4 logMAR in the affected eye, no previous intervention for epiretinal membrane, and phakic crystalline lens status in both eyes. Moreover, the patients with any of the following conditions were excluded: ocular surface problems such as corneal scar, haze, and degeneration, glaucoma, uveitis, a history of ocular surgery or trauma, the patients who require tamponade usage at the end of the surgery, and those who were not sufficiently cooperative for Pentacam-HR examinations. The patients were excluded if they were pseudophakic in one or both eyes. Additionally, phakic patients with a cortical, anterior or posterior subcapsular, or advanced nuclear cataract were not included from the study since they may affect the reliability of lens densitometry measurements.
All patients underwent a comprehensive ophthalmic examination including BCVA testing using the Snellen chart, intraocular pressure (IOP) measurement with Goldman applanation tonometry, anterior segment examination with slit lamp biomicroscopy, dilated fundoscopy, optical coherence tomography, and Pentacam HR examination preoperatively. In order to calculate and compare visual acuity, Snellen acuity was converted to logMAR.
Lens densitometry measurements
Pentacam analysis to determine the lens densitometry was performed by the same experienced masked clinician using the same Pentacam HR-Scheimpflug imaging system and all measurements were taken under standard dim-light conditions. The automatic release mode was used to reduce operator dependent variables. In this mode, the instrument automatically determines when correct focus and alignment with the corneal apex are achieved and then performs a scan. In less than 2 s, the rotating camera captures up to 25 slit images of the anterior segment. Three measurements were performed per eye, and the one with the best alignment and fixation was selected for data analysis. Distorted images caused by high reflection that were not eligible for evaluation were not included in the analysis. The measurements were performed after an enough pupil dilatation. To induce pupil dilation, two drops of cyclopentolate hydrochloride 1% were administered 5 min apart and measurements were taken approximately 45 min after the last drop. Three-dimensional scan modes were used for the measurement of lens density.18 The densitometry was analyzed using densitometry zones of the Pentacam device. As illustrated in Figure 1, the mean value was calculated in predefined 3D zones centred around the pupil centre (zone 1: 2.0 mm, zone 2: 4.0 mm, and zone 3: 6.0 mm).
These lens densitometry measurements were taken preoperatively and on the first week, first month, and third month postoperatively.
Surgical technique
In each case, the 27-g MIVS was performed under local anaesthesia by retrobulbar injection. All surgeries were performed using the Constellation Vitrectomy 27+ Total Plus Pak vitrectomy system (Alcon Laboratories, Fort Worth, Texas, USA) by the same surgeon (KS). Cannulas were inserted in the inferotemporal, superotemporal, and superonasal quadrants 3.0–4 mm posterior to the limbus. The conjunctiva and tenon capsule were displaced over the sclera to avoid communication between conjunctival and scleral entry sites. Trocar cannulas were inserted tangentially at an angle of approximately 30°, parallel to the limbus. All eyes underwent core vitrectomy followed by removal of the posterior hyaloid membrane and vitreous traction. After vitrectomy, the surgeon used end-gripping microforceps to peel the epiretinal membrane from the macular surface within the vascular arcades. No intraocular tamponade including gas or silicon oil was used. At the end of the surgery, microcannulas were removed from the eye. The infusion line was clamped during removal of the microcannula and then unclamped after removal. The conjunctiva overlying the sclerotomy was slightly displaced to disrupt the alignment between both entry sites. Passage of the 27-G instruments through the microcannula was found to be uncomplicated and no sutures were needed to close the scleral or conjunctival openings. No intra-operative complications occurred in any eye.
Postoperative follow-up
All patients used postoperative topical antibiotic and steroid for two months with tapering dose. The BCVA, IOP measurement, slit lamp microscopy, and dilated fundus examinations were repeated on the first week, first month, and third month postoperatively. Patients with any sign of abnormal inflammation (overmuch anterior chamber and vitreous cells), iatrogenic lens or posterior capsule damage, an increase in IOP higher than 20 mm Hg were excluded from the study.
Statistical analysis
The study data were analysed using the Statistical Package for Social Sciences (SPSS) for Windows version 22.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were presented as mean±standard deviation, frequency distribution, and percentages. Normal distribution of the variables was tested by visual (histogram and probability graphs) and analytical methods (Kolmogorov–Smirnov/Shapiro–Wilk Test). For inter-group and intra-group comparisons, the paired samples t-tests were used for normally distributed variables and Wilcoxon signed rank tests were used for those that were not normally distributed. The statistical significance was set at P<0.05.
Results
This study included 24 patients who underwent 27-G MIVS without any tamponade and followed-up at least 3 months. Overall, 15 (62.5%) of the patients were female and 9 (37.5%) were male. The mean age of the patients was 64.55±7.80 (range: 42–76) years. The mean operation time was 34.7 min (range 20–43 min).
The mean preoperative BCVA was 0.74±0.27 (range: 1.3–0.4) logMAR. The mean overall BCVA was 0.38±0.21 (range: 0.80–0.10) on the first week, 0.22±0.18 (range: 0.70–0.00) on the first month, and 0.10±0.11 (range: 0.40–0.00) on the third months postoperatively. There was a statistically significant improvement in the BCVA on the first week, first month, and third months compared to the preoperative BCVA (P<0.05, for all).
As illustrated in Table 1, the first week postoperative lens densitometry values in the study eyes and healthy fellow eyes were similar to preoperative lens densitometry values in all lens zones (P>0.05 for all). Table 2 demonstrates the lens densitometry values in the study and fellow eyes preoperatively and on the first month postoperatively. The mean lens densitometry values at Zone 1 and average lens densitometry values statistically significantly increased in the study eyes on the first month when compared with the preoperative values (P=0.011, P=0.033, respectively). Additionally, there were statistically significant differences regarding the mean lens densitometry values of Zone 1 and Zone 2, and also average lens densitometry values between the preoperative and third month postoperative values (P=0.003, P=0.021, P=0.009, respectively) (Table 3). On the other hand, the densitometry values of fellow eyes were similar at preoperatively and all the postoperative follow-up periods (P>0.05 for all).
Discussion
Despite the technical advances in retina and vitreous surgery, cataract remains as the most common postoperative complication and reduces visual acuity benefits of vitrectomy. Apparently, up to 80–90% of patients would require post-vitrectomy cataract surgery within 2 years after surgery.8, 19 This factor has led most of the previous vitrectomy reports for epiretinal membranes to potentially underestimate the benefits of vitreous surgery.
Regarding the rapid increase in lens density after PPV, there might be several possible mechanisms: intraoperative light toxicity,6, 20 intraoperative oxidation of lens proteins,21 surgery-introduced changes of the lens’ biochemical microenvironment, and postoperative factors (IOP, intraocular inflammation, and lens’ biochemical microenvironment).22, 23 It was thought that crystalline lens exposure to ultraviolet light from the microscope during vitrectomy might produce nuclear sclerotic cataracts. Observation of cataract formation in mice exposed to ultraviolet light supports this hypothesis.24 However, Taylor et al25 reported that the ultraviolet radiation detected in human eyes exposed to high cumulative solar exposure, which exceeds that of the operating microscope did not cause increased nuclear sclerosis. If intraoperative light toxicity or oxidation of lens proteins is an important factor, longer operation time should lead to faster lens density progression and higher grade cataracts. However, Cheng et al23 reported that although vitrectomy is a risk factor for nuclear sclerosis progression, the duration of vitrectomy does not increase the risk. In our study, cases with the same aetiology were selected, and operations were performed by the same surgeon to eliminate the differences that the surgical duration could create.
A study of 21 eyes using ‘nonvitrectomizing’ vitreous surgery for epiretinal membranes in patients older than age 50 years showed no increased nuclear sclerosis in surgical eyes compared with fellow eyes during a mean follow-up of 9.7 months.26 A second study including longer follow-up of the 21 eyes in their prior study was reported no significant difference in nuclear sclerosis or myopic shift between the surgical and fellow eyes after a mean follow-up of 22 months by the same authors.27 The two studies suggest that the increase in nuclear sclerosis after vitrectomy might be directly or indirectly related to the removal of vitreous gel.
The human crystalline lens exists in a relatively hypoxic state, a condition hypothesized to be important in preserving the clarity of lens.28 The oxygen in the avascular lens is provided by diffusion which means that the surrounding oxygen content is very important for the oxygen content within the lens and, consequently, for the formation of reactive oxygen species. In the absence of the vitreous gel since the vitreous is lacking as a diffusion barrier for the oxygen, molecular oxygen from the retinal vasculature reaches the lens, where it promotes oxidative damage of the lens nucleus, an increase in light scattering, and nuclear sclerotic cataract.19 In support of this theory, Holekamp et al29, 30 also showed that postvitrectomy lens density was significantly lower in patients with ischemic diabetic retinopathy than with non-ischemic eyes, possibly associated with lower partial oxygen pressure in the vitreous cavity of ischemic eyes. In addition, when the vitreous is eliminated during vitrectomy, the level of ascorbate, which is a vitreous antioxidant that could neutralize the excess of oxygen in the vitreous cavity, decreases.31
Feng et al10 found no significant difference in the rate of cataract extraction between 20-G and small G PPV. Almony et al32 also reported that the disruption and removal of the vitreous gel itself, and not the gauge of vitrectomy, is associated with the significant progression of nuclear sclerotic cataract. Even so, only cases that underwent 27-G vitrectomy were included to present study to avoid differences that could be caused by gauge of vitrectomy.
Various lens opacity grading systems have been developed for grading cataracts. The Lens Opacity Classification System II (LOCS II) uses colour lens photograph standards that are compared with the patient lens that is graded on a scale from 0 to 4 by comparison with these standards.33 The LOCS III, which is a more quantitative version of the LOCS II scale, uses slit-lamp photographs of the lens for each patient in the study with grading of nuclear colour and opalescence on a scale from 0.1 (clear) to 6.9 (very opaque) by masked graders rather than by the physician examiner.34 Another different approach is to measure lens autofluorescence by fluorophotometry. Scheimpflug cataract imaging system, that is an objective cataract grading method using a modified slit beam, has been used to study the ocular lens for the past three decades.35, 36
The changes in lens densities after vitrectomy were investigated with the above-mentioned techniques. Ogura and associates21 evaluated autofluorescence in the lens at the centre along the ocular axis by fluorophotometry and found more autofluorescence in operated eyes than in fellow eyes 2 years after vitrectomy for idiopathic epimacular proliferation, which indicated an accumulation of fluorescent materials in the lens. Thompson et al37 graded lenses by using the Chylack LOCS II lens grading scale of nuclear sclerosis and reported that the increase in nuclear sclerosis in the vitrectomized eye compared with the fellow eyes was about sixfold to sevenfold in all patient age ranges after vitrectomy. Melberg et al38 reported that 79% of patients older than 50 years of age developed significant lens opacity in the surgical eye compared with the nonsurgical eye by using LOCS III. Ibán∼ ez-Ruiz et al39 found a significantly higher linear optical density obtained utilizing the Scheimpflug camera of the Oculus-Pentacam device in the 81 vitrectomized phakic eyes when compared to the non-vitrectomized eyes. Because the early stages of cataract are difficult to differentiate by using clinical classifications such as LOCS II, LOCS III, we used lens densitometry analysis of Pentacam HR-Scheimpflug imaging system, which is a quantitative and objective method providing precise and reproducible data related to lens clarity.17
To our knowledge, this is the first study to evaluate lens densitometry by densitometry analysis of Pentacam HR-Scheimpflug imaging system that enables an objective measurement method for progression of cataract after vitrectomy. The strengths of our study include the following: because of its prospective design, cases with similar surgical procedures and duration were included to the study. The surgeries were performed by the same surgeon and lens densitometry measurements were performed on the same postoperative days. And also the data collection was done with standardized imaging modality. The important limitations of this study are relatively small sample-size and short follow-up after vitrectomy.
This study suggests that 27-G MIVS vitrectomy might cause post-surgical lens density changes even in early postoperative months and vitreous may play an important role in protecting the transparency of the lens. Densitometry analysis of Pentacam HR-Scheimpflug imaging system is a quantitative and objective measurement method that can detect changes in the lens density that cannot be clinically determined and can help predict longitudinal cataract progression after vitrectomy.

References
Oshima Y, Wakabayashi T, Sato T, Ohji M, Tano Y . A 27-gauge instrument system for transconjunctival sutureless microincision vitrectomy surgery. Ophthalmology 2010; 117: 93–102.
Lakhanpal RR, Humayun MS, de Juan E Jr, Lim JI, Chong LP, Chang TS et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology 2005; 112: 817–824.
Fabian ID, Moisseiev J . Sutureless vitrectomy: evolution and current practices. Br J Ophthalmol 2011; 95: 318–324.
Khan MA, Shahlaee A, Toussaint B, Hsu J, Sivalingam A, Dugel PU et al. Outcomes of 27 gauge microincision vitrectomy surgery for posterior segment disease. Am J Ophthalmol 2016; 161: 36–43.
Tekin K, Sonmez K, Inanc M, Ozdemir K, Goker YS, Yilmazbas P . Evaluation of corneal topographic changes and surgically induced astigmatism after transconjunctival 27-gauge microincision vitrectomy surgery. Int Ophthalmol 2017. e-pub ahead of print 30 Mar 2017 doi:10.1007/s10792-017-0507-5.
Cherfan GM, Michels RG, de Bustros S, Enger C, Glaser BM . Nuclear sclerotic cataract after vitrectomy for idiopathic epiretinal membranes causing macular pucker. Am J Ophthalmol 1991; 111: 434–438.
Hsuan JD, Brown NA, Bron AJ, Patel CK, Rosen PH . Posterior subcapsular and nuclear cataract after vitrectomy. J Cataract Refract Surg 2001; 27: 437–444.
Panozzo G, Parolini B . Cataracts associated with posterior segment surgery. Ophthalmol Clin North Am 2004; 17: 557–568.
Rizzo S, Genovesi-Ebert F, Murri S, Belting C, Vento A, Cresti F et al. 25-gauge, sutureless vitrectomy and standart 20-gauge pars plana vitrectomy in idiopathic epiretinal membrane surgery: a comparative pilot study. Graefes Arch Clin Exp Ophthalmol 2006; 244: 472–479.
Feng H, Adelman RA . Cataract formation following vitreoretinal procedures. Clin Ophthalmol 2014; 8: 1957–1965.
Konstantopoulos A, Hossain P, Anderson DF . Recent advances in ophthalmic anterior segment imaging: a new era for ophthalmic diagnosis? Br J Ophthalmol 2007; 91: 551–557.
Belin MW, Ambrósio R . Scheimpflug imaging for keratoconus and ectatic disease. Indian J Ophthalmol 2013; 61: 401–406.
Piñero DP . Technologies for anatomical and geometric characterization of the corneal structure and anterior segment: a review. Semin Ophthalmol 2015; 30: 161–170.
Lim DH, Kim TH, Chung ES, Chung TY . Measurement of lens density using Scheimpflug imaging system as a screening test in the field of health examination for age-related cataract. Br J Ophthalmol 2015; 99: 184–191.
Grewal DS, Brar GS, Grewal SP . Correlation of nuclear cataract lens density using Scheimpflug images with Lens Opacities Classification System III and visual function. Ophthalmology 2009; 116: 1436–1443.
Kirkwood BJ, Hendicott PL, Read SA, Pesudovs K . Repeability and validity of lens densitometry measured with Scheimpflug imaging. J Cataract Refract Surg 2009; 35: 1210–1215.
Weiner X, Baumeister M, Kohnen T, Bühren J . Repeatability of lens densitometry using Scheimpflug imaging. J Cataract Refract Surg 2014; 40: 756–763.
Magalhães FP, Costa EF, Cariello AJ, Rodrigues EB, Hofling-Lima AL . Comparative analysis of the nuclear lens opalescence by the Lens Opacities Classification System III with nuclear density values provided by Oculus Pentacam: a cross-section study using Pentacam Nucleus Staging software. Arq Bras Oftalmol 2011; 74: 110–113.
Holekamp NM, Shui YB, Beebe DC . Vitrectomy surgery increases oxygen exposure to the lens: a possible mechanism for nuclear cataract formation. Am J Ophthalmol 2005; 139: 302–310.
de Bustros S, Thompson JT, Michels RG, Enger C, Rice TA, Glaser BM . Nuclear sclerosis after vitrectomy for idiopathic epiretinal membranes. Am J Ophthalmol 1988; 105: 160–164.
Ogura Y, Takanashi T, Ishigooka H, Ogino N . Quantitative analysis of lens changes after vitrectomy by fluorophotometry. Am J Ophthalmol 1991; 111: 179–183.
Thompson JT, Glaser BM, Sjaarda RN, Murphy RP . Progression of nuclear sclerosis and long-term visual results of vitrectomy with transforming growth factor beta-2 for macular holes. Am J Ophthalmol 1995; 119: 48–54.
Cheng L, Azen SP, El-Bradey MH, Scholz BM, Chaidhawangul S, Toyoguchi M . Duration of vitrectomy and postoperative cataract in the vitrectomy for macular hole study. Am J Ophthalmol 2001; 132: 881–887.
Michael R . Development and repair of cataract induced by ultraviolet radiation. Ophthalmic Res 2000; 32: 1–44.
Taylor HR, West SK, Rosenthan FS, Muñoz B, Newland HS, Abbey H et al. Effect of ultraviolet radiation on cataract formation. N Engl J Med 1989; 319: 1429–1433.
Saito Y, Lewis JM, Park I, Ikuno Y, Hayashi A, Ohji M et al. Nonvitrectomy vitreous surgery: a strategy to prevent postoperative nuclear sclerosis. Ophthalmology 1999; 106: 1541–1545.
Sawa M, Saito Y, Hayashi A, Kusaka S, Ohji M, Tano Y . Assessment of nuclear sclerosis after nonvitrectoming vitreous surgery. Am J Ophthalmol 2001; 132: 356–362.
Eaton JW . Is the lens canned? Free Radic Biol Med 1991; 11: 207–213.
Holekamp NM, Shui YB, Beebe D . Lower intraocular oxygen tension in diabetic patients: possible contribution to decreased incidence of nuclear sclerotic cataract. Am J Ophthalmol 2006; 141: 1027–1032.
Holekamp NM, Bai F, Shui YB, Almony A, Beebe DC . Ischemic diabetic retinopathy may protect against nuclear sclerotic cataract. Am J Ophthalmol 2010; 150: 543–550.
Shui YB, Holekamp NM, Kramer BC, Crowley JR, Wilkins MA, Chu F et al. The gel state of the vitreous and ascorbate-dependent oxygen consumption: relationship to the etiology of nuclear cataracts. Arch Ophthalmol 2009; 127: 475–482.
Almony A, Holekamp NM, Bai F, Shui YB, Beebe D . Small-gauge vitrectomy does not protect against nuclear sclerotic cataract. Retina 2012; 32: 499–505.
Chylack LT Jr, Leske C, McCarthy D, Khu P, Kashiwagi T, Sperduto R . Lens opacity classification system II (LOCS II). Arch Ophthalmol 1989; 107: 991–997.
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 1993; 111: 831–836.
Vivino MA, Chintalagiri S, Trus B . Development of a Scheimpflug slit lamp camera system for quantitative densitometric analysis. Eye (Lond) 1993; 7: 791–798.
Datiles MB, Magno BV, Freidlin V . Study of nuclear cataract progression using the National Eye Institute Scheimpflug system. Br J Ophthalmol 1995; 79: 527–534.
Thompson JT . The role of patient age and intraocular gases in cataract progression following vitrectomy for macular holes and epiretinal membranes. Trans Am Ophthalmol Soc 2003; 101: 485–498.
Melberg NS, Thomas MA . Nuclear sclerotic cataract after vitrectomy in patients younger than 50 years of age. Ophthalmology 1995; 102: 1466–1471.
Ibáñez-Ruiz MA, Beneyto-Martin P, Pérez-Martínez MT . Lens density measurement with Scheimpflug camera in vitrectomised eyes. Arch Soc Esp Oftalmol 2016; 91: 385–390.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We would like to thank Dr Onder Aydemir from the Department of Public Health, Gazi University Faculty of Medicine for his assistance in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tekin, K., Inanc, M., Ozdemir, K. et al. The quantitative assessment of alterations in lens transparency after transconjunctival 27-gauge microincision vitrectomy surgery. Eye 32, 515–521 (2018). https://doi.org/10.1038/eye.2017.234
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.234
This article is cited by
-
An objective evaluation of lens transparency after vitrectomy surgery with different intravitreal tamponades
International Ophthalmology (2022)