Abstract
Purpose
To assess outcomes of surgical management of malignant glaucoma in terms of re-formation of anterior chamber
Methods
This was a retrospective analysis of consecutive patients who underwent surgical treatment for malignant glaucoma between January 1995 and December 2013 at a tertiary care ophthalmic institute, with a minimum follow up of 2 months.
Results
Fifty eight eyes of 58 patients were included. Fifty two (89.7%) patients had primary angle closure glaucoma. The majority had undergone glaucoma filtration surgery earlier (n=53, 91.4%). Lensectomy and anterior vitrectomy was performed in 15 (25.9%) eyes (Group 1). Vitrectomy and anterior chamber re-formation was performed in 27 (46.6%) eyes (Group 2). Vitrectomy-phacoemulsification-vitrectomy was performed in 16 (27.6%) eyes (Group 3). Communication between the two segments of eye through anterior hyaloid, lens capsule complex and/or iris was achieved in all groups. The median follow-up (Inter-quartile range) was 30 (71.5) months. Anterior chamber re-formation was achieved in 56 (96.5%) eyes at final visit. The improvement in mean±SD LogMAR visual acuity (1.1±1 to 0.7±0.8) and reduction in number ±SD of anti-glaucoma medications (2.1±1.1 to 1±1.6) between onset and final visit were significant (P=0.02 and <0.01, respectively). The intraocular pressure (mm Hg) at onset and at final visit was 30.7±17.4 and 14±6.2, 32.8±12.6 and 15.3±7.4, and 27.2±14 and 10.9±3 in groups 1–3, respectively (all P<0.01).
Conclusion
Our anatomical success rate was high. The key element in achieving this outcome was the establishment of a patent communication between the vitreous cavity and the anterior chamber.
Similar content being viewed by others
Introduction
Aqueous misdirection syndrome, more commonly referred to as malignant glaucoma, is a term used to describe a spectrum of disorders with several common features which typically include a shallow or flat anterior chamber with elevated, normal, or occasionally low intraocular pressure at some point during the course of the disease in the presence of a patent peripheral iridectomy with no retinal pathology such as suprachoroidal hemorrhage or choroidal effusion.1, 2, 3 Eyes with primary angle closure disease appear to be particularly susceptible to develop this condition.4, 5 The phenomenon commonly follows an intraocular surgery, most commonly glaucoma filtering surgery, or laser procedures such as laser iridotomy, laser cyclophotocoagulation, laser posterior capsulotomy and laser suture lysis, and in rare instances has been reported to occur spontaneously as well.6, 7, 8, 9, 10, 11, 12 Several mechanisms have been described to explain the pathogenesis of this phenomenon.1, 13 The key element appears to be a barrier in the forward movement of aqueous due to cilio-lenticular block in phakic eyes, or irido-cilio-vitreal block in aphakic or pseudophakic eyes. Disproporortionately large crystalline lenses in small eyes leading to increased cilio-lenticular apposition may predispose these eyes to the development of malignant glaucoma. The mechanism in aphakic and psedophakic eyes is thought to be an increased flow resistance through the vitreous gel resulting in compression of the anterior hyaloid and high resistance to aqueous flow, thereby creating a vicious cycle. Moreover, choroidal expansion has been hypothesiszed to initiate the condition by reducing the movement of aqueous across the condensed vitreous gel.14
The initial treatment of malignant glaucoma is the use of cycloplegia to move the lens-iris diaphragm backwards and widen the middle segment of the eye, aqueous suppressants to reduce the flow of aqueous into the vitreous cavity and hyper osmotic agents to reduce vitreous volume.1, 2 Topical steroids are used to reduce inflammation. Laser treatment in the form of laser capsulotomy with anterior hyaloidotomy to incise the thickened anterior hyaloid or cyclophotocoagulation to shrink the ciliary processes and thereby to break the ciliary block are attempted if medical treatment remains ineffective in pseudophakic or aphakic eyes.15, 16 Surgical modalities are resorted to, if the first two steps fail. The primary goal of surgical treatment is to re-establish a communication between the posterior and anterior segments of the eye. The various approaches reported in the literature include vitreous incision and aspiration of the trapped aqueous, pars plana vitrectomy, vitrectomy-phacoemuslification-vitrectomy in phakic eyes, vitrectomy with hyaloido-zonulectomy and peripheral iridectomy, and vitrectomy with insertion of a glaucoma drainage device.17, 18, 19, 20, 21, 22
The primary aim of this study was to assess the outcomes of surgical management of malignant glaucoma in terms of re-formation of the anterior chamber. Secondary outcome measures included changes in visual acuity, intraocular pressure (IOP) control, the number of IOP lowering medication(s) being used, recurrence rate, complications and re-operations required for IOP control.
Materials and methods
The medical records of consecutive patients who had been diagnosed with malignant glaucoma between January 1995 and December 2013 and who underwent surgical treatment for the same, were reviewed. The study was approved by the Institutional Review Board and Ethics committee. Diagnostic criteria for malignant glaucoma included a flat or uniformly shallow anterior chamber following an intraocular surgery with a patent peripheral iridectomy, irrespective of the level of IOP. Patients with other forms of secondary angle closure glaucoma such as pupillary block glaucoma or glaucoma following suprachoroidal hemorrhage in the early post-operative period, patients in whom suprachoroidal effusion was detected either by indirect ophthalmoscopy or by B-scan echography, as well as patients with less than eight weeks of follow up were excluded.
Data collection
The following details were extracted from chart review: age, gender, type of pre-existing glaucoma, visual acuity measurement, details of slit lamp examination, applanation tonometry readings and details of fundus evaluation. Visual acuity measurements were obtained using the Snellen chart and were converted to LogMAR (logarithm of the reciprocal of the minimal angle of resolution) for the purpose of statistical analysis. Details of surgeries performed prior to development of aqueous misdirection were noted. The duration of aqueous misdirection was calculated from the time of diagnosis or presentation until the reversal of the condition by treatment. Some patients did undergo ultrasound biomicroscopy to verify the diagnosis and details of the same were noted. Details of surgical treatment performed and intra- and post-operative complications were also noted. Follow up data including number of IOP lowering medications being used, visual acuity, anterior segment examination, IOP measurement, laser or surgical re-interventions performed, and recurrences and management of the same were noted up to the final follow up visit.
Management protocol for malignant glaucoma
The standard practice at our institute involves a stepped up regimen of care for the condition. Medical treatment was attempted first, consisting of cyclopegics i.e either atropine sulfate 1% or homatropine hydrochloride 2%, topical steroid, topical aqueous suppressant(s) and systemic acetazolamide. Intravenous injection of 20% solution of Mannitol was administered at the discretion of the treating ophthalmologist. Reversal of aqueous misdirection was defined as re-formation of the central anterior chamber with IOP≤18 mm Hg with or without medication(s). If reversal did not occur within a period of five to seven days, laser intervention in the form of Yttrium Aluminum Garnet (YAG) laser capsulotomy with anterior hyaloidotomy was performed in aphakic or pseudophakic eyes (Visulas YAG III, Carl Zeiss Meditech, Dublin, CA, USA). The laser was used to clear any fibrin suspected of blocking the pre- existing iridotomy or to enlarge it, or to gain access to the posterior capsule and anterior hyaloid in that area. Diode cyclophotocoagulation (Iridex Corporation, Oculight SLx., Mountain view, CA, USA) was performed in eyes with poor visual potential due to advanced glaucomatous damage or in those who refused surgical therapy. Surgical treatment was reserved for those who did not respond to medical and/or laser therapy.
Surgical procedures
The surgical techniques were aimed at reversing aqueous misdirection by providing a communication between the vitreous cavity and the anterior chamber.
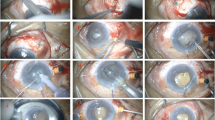
Group I
Pars plana lensectomy with vitrectomy was performed in phakic eyes before the technique of phacoemulsification became popular at our institution. After placing an infusion cannula in the infero-temporal quadrant, lensectomy and anterior vitrectomy were performed without vitreous base excision, accompanied by a peripheral iridectomy. Anterior synechiolysis was done under viscoelastic cover for persistent peripheral anterior synechiae, if any using an iris spatula.
Group II
Pars plana vitrectomy with anterior chamber re-formation was performed in pseudophakic or aphakic eyes. A clear communication was established between the vitreous cavity and anterior chamber by cutting through the lens capsule and the peripheral iris using the vitreous cutter from a posterior approach.
Group III
The technique of phacoemulsification was introduced subsequently to deal with the crystalline lens. A partial anterior vitrectomy was done at the outset to de-bulk the vitreous. The anterior chamber was then reformed using sodium hyaluronate through a paracentesis. Phacoemulsification was performed through a clear corneal incision and a foldable hydrophobic lens was implanted in the capsular bag. A peripheral iridectomy with zonulo-capsulo-hyaloidotomy was performed through the pars plana route. Patency of this communication was verified by introducing the cutter through the peripheral iridectomy from the posterior segment into the anterior chamber. The sclerotomies were placed at 3 to 3.5 mm from the limbus in all eyes.
Post-operative medications included cyclopegics, topical and/or systemic steroids, topical antibiotics, and aqueous suppressants. Steroids as well as aqueous suppressants were tapered over a period of 6–8 weeks at the discretion of the treating ophthalmologist. Patients were followed up at 1 day, 1 week, and 6 weeks after surgery and at varied interval thereafter until the final visit.
Definitions
Anatomical success
Re-formation of the central anterior chamber on slit lamp biomicroscopic examination was defined as anatomical success. This was also the primary outcome measure.
Complete success
An IOP of ≥6 mm Hg and ≤18 mm Hg without IOP lowering medication, with a well formed central anterior chamber, with either improvement in visual acuity or visual acuity measurements within three lines of the presenting visual acuity, and no suprachoroidal hemorrhage.
Qualified success
The above criteria with IOP≤18 mm Hg with IOP lowering medication(s).
Recurrence
Detection of a shallow or flat anterior chamber with or without elevated IOP after initial recovery with surgical treatment, at any point in time after the treatment was instituted.
Statistical analysis
The Kolmogorov-Smirnov test was applied to check the distribution of the data. Comparison of continuous data was done by independent samples Student’s t-test for normally distributed data. The Mann–Whitney test and the Wilcoxon signed- rank test were applied to non-normally distributed data. χ2- and Fisher’s exact tests were used, as appropriate, to analyze categorical data. A P value of less than 0.05 was considered to be statistically significant. Cumulative probability of survival was depicted using Kaplan–Meier survival analysis. The Cox proportional hazards model was used to assess risk factors for failure and for corneal decompensation. Statistical analysis was performed with commercial software (SPSS version 14, SPSS, Inc., Chicago, IL, USA: released 2007).
Results
The medical records of 58 consecutive patients who had been diagnosed with aqueous misdirection syndrome between January 1995 and December 2013 and necessitated surgical treatment for the same, were reviewed. Baseline demographic data are depicted in Table 1. There were no significant differences in the baseline demographics between the three surgical groups apart from age and type of previous surgery. (Supplementary Table 1). Majority of the eyes (52; 89.7%) had been diagnosed with primary angle closure disease. Thirty one (53.4%) eyes did develop the condition following an intraocular surgery at our institution.
Precipitating events were identified by their temporal relationship with the onset of glaucoma in 12 (20.6%) eyes. These included laser suture lysis, wound leak, and posterior vitreous detachment in one eye each, over-filtration with shallow anterior chamber in five eyes, valsalva’s maneuver caused by an episode of vomiting in one eye, YAG laser capsulotomy in one eye and ocular trauma in two eyes.
Forty five patients (77.5%) underwent ultrasound biomicroscopic examination to confirm the diagnosis of malignant glaucoma. This revealed shallow or flat anterior chamber with anterior rotation of the ciliary body in 38 eyes (84.4%). This was accompanied by supraciliary effusion in 6 eyes (13.3%). The clinical features, details of surgical treatment, and outcome of these six patients are depicted in Table 2. Choroidal detachments were not detected either by ophthalmoscopic or by B-scan echography, nor was suprachoroidal fluid detected while performing sclerotomies during surgical management of malignant glaucoma, in any of these eyes. The trabeculectomy stoma was blocked by ciliary processes in one eye (1.7%).
The distribution of patients into three groups of surgical technique was as follows. Lensectomy and anterior vitrectomy was performed in 15 (25.9%) eyes (Group 1). Vitrectomy with peripheral iridectomy, capsulotomy and anterior chamber re-formation was performed in 27 (46.6%) eyes (Group 2). Vitrectomy-phacoemulsification-vitrectomy with zonulo-hyaloidotomy and peripheral iridectomy was performed in 16 (27.6%) eyes (Group 3).
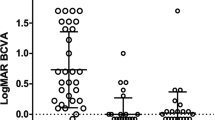
Anatomical success was achieved in 13 eyes (86.6%) in Group I, 27 eyes (100%) in group II and 16 eyes (100%) in Group III (P=0.05). There were no significant differences in the post-operative outcome at the final visit, between the three groups in terms of visual acuity, intraocular pressure and complication rates (Supplementary Table 2). However, patients in Group I were less likely to achieve anatomical success and needed re-operation for IOP control more frequently. Overall, there was a significant improvement in the mean±Standard Deviation LogMAR visual acuity at the final visit (0.7±0.8) compared to the mean visual acuity at the onset (1.1±1, P=0.02). The IOP at the onset and that at the final visit was 30.7±17.4 and 14±6.2 mm Hg, 32.8±12.6 and 15.3±7.4 mm Hg, and 27.2±14 and 10.9±3 mm Hg in groups 1–3, respectively (all P-values <0.01, Figure 1). Comprehensively, the mean number of IOP lowering medications decreased from 2.1±1.1 at the onset to 1±1.6 at the final visit (P<0.01).
Complications of surgery included severe inflammation in 3 eyes (5.1%), hyphema in one eye (1.7%), vitreous hemorrhage in one eye (1.7%), corneal decompensation in 10 eyes (17.2%) and suprachoridal hemorrhage in one eye (1.3%).
Complete and qualified success was achieved in 19 (32.8%) and 30 (51.7%) eyes, respectively at the final follow-up. The remaining 9 (15.5%) eyes were failures. The reasons for failure included elevated IOP in 2 (3.4%) eyes, loss of vision by more than three lines in 5 (8.6%) eyes, and inability to form the anterior chamber with elevated IOP in 2 (3.4%) eyes. Cumulative probability of complete success by Kaplan–Meier survival analysis was 80% at 12 months, 69% at 36 months and 66% at the end of 60 months (Figure 2a). Similarly, the probability of qualified success was 91% at 12 months, 83% at 36 months and 44% at the end of 60 months (Figure 2b).
Recurrence of aqueous misdirection occurred in 5 (8.6%) eyes. The precipitating factors for recurrence included wound leak in 1 (1.7%) eye, fibrin reaction blocking the peripheral iridectomy in 3 (5.2%) eyes, and discontinuation of systemic Acetazolamide therapy in 1 (1.7%) eye. Time to recurrence varied from 5-120 (median 60, inter-quartile range of 90) days. Recurrences were successfully managed by conservative treatment (anti-inflammatory medication(s) and re-institution of treatment with systemic Acetazolamide) in 4 (6.8%) eyes and performance of YAG laser iridotomy in 1 (1.7%) eye.
Risk factors analyzed for failure of surgical treatment using the Cox proportional hazard model included age, gender, type of previous surgery, IOP at the onset of malignant glaucoma, lens status, and recurrence. None of them were found to be significant.
Risk factors assessed for corneal decompensation included age, gender, IOP at the onset of malignant glaucoma, duration of malignant glaucoma, type of surgery for malignant glaucoma and follow-up period. Increasing age was found to be a significant risk factor (HR 1 (95% CI 1, 1.1 (p=0.04). There was no significant difference between the LogMAR visual acuity at the onset of malignant glaucoma (1.69±0.55) and the visual acuity recorded at the final visit (1.56±1.17), in these eyes (P=0.27).
Re-operation was required to achieve IOP control in 9 (15.5%) eyes. Trabeculectomy with Mitomycin C was performed in 2 (3.4%) eyes, Ahmed glaucoma valve implant in 5 (8.6%) eyes and Diode cyclophotocoagulation in 2 (3.4%) eyes.
Discussion
We analyzed the outcome of surgical treatment of malignant glaucoma when the condition could not be relieved by other measures. We could achieve anatomical success in over 96% eyes. The key element in a successful outcome appears to be the establishment of a patent communication between the posterior and the anterior chambers of the eye.
Majority of eyes (50; 89.7%) in our series had been diagnosed to have angle closure disease, which is consistent with the existing literature.1, 2 The factors which have been earlier reported to precipitate aqueous misdirection are wound leak, laser suture lysis, use of miotics, withdrawal of cycloplegic drugs, and needling of the trabeculectomy bleb.1, 2, 23, 24, 25 Some of these precipitating factors were identified in about a fifth of our patients as well.
Ultrasound biomicroscopic features in eyes with malignant glaucoma were first described by Trope et al26 in two phakic eyes. UBM revealed anterior rotation of the ciliary processes, supraciliary effusion and obstruction of the trabeculectomy stoma in the both eyes. One of the patients underwent pars plana vitrectomy six days following the development of malignant glaucoma. No fluid was detected at the sclerotomy site. Peripheral annular choroidal detachment following trabeculectomy resulting in uniform shallowing of the anterior chamber in a manner similar to aqueous misdirection was described by Liebmann et al27 in six eyes. The detachment was confirmed with UBM.27 Clinical features were suggestive of malignant glaucoma in these eyes. Choroidal effusion had not been detected by either ophthalmoscopy or by B-scan echography. Four of these eyes settled with medical treatment while two required surgery to drain the choroidal effusion. The authors admit that the presence of the supraciliary effusion does not exclude some degree of aqueous misdirection in these eyes.
While anterior rotation of the ciliary processes and shallow or flat anterior chamber was seen in the majority of our patients who underwent UBM examination, only 10% were found to have supraciliary effusion, which was not detected either by clinical examination or by B-scan echography. Suprachoroidal fluid was not detected while performing sclerotomies, in any of these eyes. The volume of fluid may have been insufficient to be detected either by ophthalmoscopy or echography. These cases demonstrate that aqueous misdirection may be precipitated by supraciliary effusion in eyes predisposed to developing this condition. Ciliary bodies which were thinner and more anteriorly rotated have also been described in eyes with malignant glaucoma as well as their fellow eyes when compared to a control group, in eyes with primary angle closure disease.28 The role of anterior segment optical coherence tomography in the diagnosis and management of this condition has also been described.29
Surgical treatment for malignant glaucoma was first described by Chandler. He used a 17-guage needle to perform fluid vitreous aspiration through a sclerotomy placed in the bed of a scleral flap, 2 mm behind the limbus.17 This technique gradually evolved with pars plana vitrectomy becoming the mainstay of the procedure. Higher success rates of 67 to 100% could be achieved in pseudophakic eyes in which the posterior capsule and anterior vitreous were breached.18, 19, 20, 21 In contrast, the success rates were lower to the magnitude of 25% in phakic eyes, despite de-bulking of the vitreous.30 These observations reveal the importance of achieving a patent communication between the vitreous cavity and the anterior chamber. The various surgical modalities described since the year 2000 emphasize the importance of producing this communication by performing an adequate peripheral iridectomy, capsulotomy and hyaloido zonulotomy either by the anterior or by the pars plana route (Table 3)31, 32, 33, 34, 35 In addition, conventional vitrectomy, when performed alone, did result in a relapse rate as high as 75%, supporting the concept.30 Hosada et al36 describe two cases of malignant glaucoma which occurred following complete pars plana vitrectomy and ultimately resolved following peripheral iridectomy with or without local zonulectomy.36
Phacoemuslification combined with posterior capsulorhexis and anterior vitrectomy following IOL implantation was described as a surgical technique in the management of twenty five phakic eyes with malignant glaucoma.37 None of the eyes developed a recurrence, nor were there any significant complications apart from IOP elevation requiring topical medications in 5 eyes. Phacoemulsification in this setting, without performing a core vitrectomy to soften the eye, can be an extremely challenging technique, however.
Our rationale in combining lens removal, anterior vitrectomy and a peripheral iridectomy, that included excision of the anterior hyaloid and capsular remnants as well, was to ensure a patent communication between the vitreous cavity and the anterior chamber. We could achieve anatomical success in over 96% eyes and control of IOP in over 84% eyes. Nevertheless, the technique may be ineffective if the flow of aqueous into the anterior chamber is blocked by the residual anterior hyaloid, fibrin or inflammatory debris. We experienced three recurrences attributable to severe inflammation with blockage of the communication between the posterior and the anterior segments of the eye. Similar report of aqueous misdirection developing in eyes which had undergone vitrectomy for retinal pathology, does exist in the literature.38
Our techniques did include removal of the crystalline lens in phakic eyes in order to facilitate this communication. Simon et al39 have described a technique which avoids damage to the crystalline lens in phakic eyes, while removing the impervious anterior vitreous gel, using videoendoscpic guided pars plana vitrectomy with staining of the vitreous gel using 20% sodium fluorescein to facilitate this process.39
The refractory nature of malignant glaucoma in our series is reflected by the fact that only about a third (32.8%) eyes achieved complete resolution of aqueous misdirection without a need for IOP lowering medications, 15% needed re-operation for IOP control and 17% developed corneal decompensation due to prolonged irido-corneal touch. These eyes were not considered as failures as their visual acuity, IOP control and the central anterior chamber depth were maintained.
Our study has several limitations. We did include only those patients in whom aqueous misdirection developed after an intraocular surgery. Therefore, our observations are not applicable when the condition develops after laser procedures or spontaneously. Also, we cannot comment on the resolution of the condition with medical and/or laser therapy. Inherent biases of retrospective studies are applicable to our study as well. Although every effort was made to identify all case records of patients who were diagnosed with malignant glaucoma and were treated surgically, some of the case records might have been missed. Nevertheless, ours is one of the largest series reported, spanning a period of almost two decades, giving us the opportunity to review the results of changing trends in management of malignant glaucoma.
In conclusion, surgical management of aqueous misdirection is effective. The most important element in a successful outcome appears to be the establishment of a patent communication between the posterior and the anterior chambers of the eye.

References
Luntz MH, Rosenblatt M . Malignant glaucoma. Surv Ophthalmol 1987; 32: 73–93.
Ruben S, Tsai J, Hitchings R . Malignant glaucoma and its management. Br J Ophthalmol 1997; 81: 163–167.
Burgansky-Eliash Z, Ishikawa H, Schuman JS . Hypotonous malignant glaucoma: Aqueous misdirection with low intraocular pressure. Ophthalmic Surg Lasers Imaging 2008; 39: 155–159.
Simmons RJ .‘ Malignant glaucoma’. Br J Ophthalmol 1951; 56 (3): 263–272.
Chandler PA .‘ Malignant glaucoma’. Am J Ophthalmol 1951; 34: 993–1000.
Tomey KF, Senft SH, Antonios SR, Shammas IV, Shihab ZM, Traverso CE . Aqueous misdirection and flat anterior chamber after posterior chamber implants with and without trabeculectomy. Arch Ophthalmol 1987; 105: 770–773.
Brooks AMV, Harper CA, Gillies WE . Occurrence of malignant glaucoma after laser iridotomy. Br J Ophthalmol 1989; 73: 617–620.
DiSclafani M, Liebman JM, Ritch R . Malignant glaucoma following argon laser release of scleral flap sutures after trabeculectomy. Am J Ophthalmol 1989; 108: 597–598.
Azuara-Blanco A, Dua HS . Malignant glaucoma after diode laser cyclophotocoagulation. Am J Ophthalmol 1999; 127: 467–469.
Arya SK, Sonika, Kochlar S, Kumar S, Kang M, Sood S . Malignant glaucoma as a complication of Nd;YAG laser posterior capsulotomy. Ophthalmic Surg Lasers Imaging 2004; 35: 248–250.
Jarade EF, Dirani A, Jabbour E, Antoun J, Tomey KF . Spontaneous simultaneous bilateral malignant glaucoma of a patient with no antecedent history of medical or surgical eye disease. Clin Ophthalmol 2014; 8: 1047–1050.
Varma DK, Belovay GW, Tam DY, Ahmed IIK . Malignant glaucoma after cataract surgery. J Cataract Refrac Surgery 2014; 40: 1843–1849.
Ng WT, Morgan W . Mechanisms and treatment of primary angle closure: a review. Clin Exp Ophthalmol 2012; 40: e218–e228.
Quigley HA, Friedmann DS, Congdon NG . Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma 2003; 12: 167–180.
Epstein DL, Steniert RF, Puliafito CA . Neodymium YAG laser therapy to the anterior hyaloid in aphakic (ciliovitreal block) glaucoma. Am J Ophthalmol 1984; 98: 137–143.
Herschler J . Laser shrinkage of the ciliary processes. A treatment for malignant (ciliary block) glaucoma. Ophthalmology 1980; 87: 1155–1159.
Chandler PA . A new operation for malignant glaucoma: a preliminary report. Trans Am Ophthalmol Soc 1964; 62: 408–419.
Lynch MG, Brown RH, Michels RG, Pollack IP, Stark WJ . Surgical vitrectomy for malignant glaucoma. Am J Ophthalmol 1986; 102: 149–153.
Byrnes GA, Leen MM, Wong TP, Benson WE . Vitrectomy for ciliary block (malignant) glaucoma. Ophthalmology 1995; 102: 1308–1311.
Debrouwere V, Stalmans P, Van Calster J, Spileers W, Zeyen T, Stalmans I . Outcomes of different management options for malignant glaucoma: a retrospective study. Graefes Arch Clin Exp Ophthalmol 2012; 250: 131–141.
Lois N, Wong D, Groenewald C . New surgical approach in the management of pseudophakic malignant glaucoma. Ophthalmology 2001; 108: 780–783.
Azuara-Blanco A, Katz LJ, Gandham SB, Spaeth GL . Pars plana tube insertion of aqueous shunt with vitrectomy in malignant glaucoma. Arch Ophthalmol 1998; 116: 808–810.
Mathur R, Gazzard G, Oen E . Malignant glaucoma following needling of a trabeculectomy bleb. Eye 2002; 16: 667–668.
Chandler PA, Grant WM . Mydriatic-cycloplegic treatment in malignant glaucoma. Arch Ophthalmol 1962; 68: 353–359.
Rieser JC, Schwarz B . Miotic induced malignant glaucoma. Arch Ophthalmol 1972; 87: 706–712.
Trope GE, Pavlin CJ, Bau A, Baumal CR, Foster FS . Malignant glaucoma. Clinical and ultrasound biomicroscopic features. Ophthalmology 1994; 101: 1030–1035.
Liebmann JM, Wienreb RN, Ritch R . Angle-closure glaucoma associated with occult annular ciliary body detachment. Arch Ophthalmol 1998; 116: 731–735.
Wang Z, Huang J, Lin J, Liang X, Cai X, Ge J et al. Quantitative measurement of the ciliary body in eyes with malignant glaucoma after trabeculectomy using ultrasound biomicroscopy. Ophthalmology 2014; 121: 862–869.
Wirbelauer C, Karandish A, Haberle H, Pham DT . Optical coherence tomography in malignant glaucoma following filtration surgery. Br J Ophthalmol 2003; 87: 952–955.
Tsai JC, Barton KA, Miller MH, Khaw PT, Hitchings RA . Surgical results in malignant glaucoma refractory to medical or laser treatment. Eye 1997; 11: 677–681.
Sharma A, Sii F, Shah P, Kirkby GR . Vitrectomy-phacoemulsification-vitrectomy for the management of aqueous misdirection syndromes in the phakic eyes. Ophthalmology 2006; 113: 1968–1973.
Bitrian E, Caprioli J . Pars plana anterior vitrectomy, hyaloido-zonulectomy and iredectomy for aqueous humor misdirection. Am J Ophthalmol 2010; 150: 82–87.
Dave P, Senthil S, Rao HL, Garudadri CS . Treatment outcomes in malignant glaucoma. Ophthalmology 2013; 120: 984–990.
Zhou C, Qian S, Yao J, Tang Y, Qian J, Luyt Y et al. Clinical analysis of 50 chinese patients with aqueous misdirection syndrome; a retrospective hospital- based study. J Int Med Res 2012; 40: 1569–1579.
He F, Quian Z, Jiang J, Fan X, Wang Z, Xu X . Clinical efficacy of modified partial pars plana vitrectomy combined with phacoemulsification for malignant glaucoma. Eye 2016; 30: 1094–1100.
Hosada Y, Akagi T, Yoshimura N . Two cases of malignant glaucoma unresolved by pars plana vittrectomy. Clin Ophthalmol 2014; 8: 677–679.
Liu X, Li M, Cheng B, Mao Z, Zhong M, Wang D et al. Phacoemuslification combined with posterior capsulorhexis and anterior viterctomy in the management of malignant glaucoma in phakic eyes. Acta Ophthalmol 2013; 91: 660–665.
Massicotte EC, Schumann JS . A malignant glaucoma-like syndrome following pars plana vitrectomy. Ophthalmology 1999; 106: 1375–1379.
Simon DM, Salmon JF . Videoendoscopic- guided fluorescein assisted vitrectomy for phakic malignant glaucoma. Arch Ophthalmol 2005; 123: 1419–1421.
Acknowledgements
We thank Natarajan Viswanathan for statistical assistance. Drs Shantha Balekudaru and Nikhil Choudhari contributed equally to the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Balekudaru, S., Choudhari, N., Rewri, P. et al. Surgical management of malignant glaucoma: a retrospective analysis of fifty eight eyes. Eye 31, 947–955 (2017). https://doi.org/10.1038/eye.2017.32
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.32
This article is cited by
-
Impact of improved minimally invasive anterior vitrectomy on the prognosis of patients with malignant glaucoma
BMC Ophthalmology (2024)
-
Aqueous misdirection syndrome: clinical outcomes and risk factors for treatment failure
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Incidence and characteristics of aqueous misdirection after glaucoma surgery in Chinese patients with primary angle-closure glaucoma
Eye and Vision (2023)
-
Clinical efficacy of inferior peripheral irido-capsulo-hyaloidotomy for pseudophakic malignant glaucoma
International Ophthalmology (2021)
-
Current Concepts on Aqueous Misdirection
Current Ophthalmology Reports (2020)