Abstract
Objective:
To examine the association of nursing overtime, nursing provision and unit occupancy rate with medical incident rates in the neonatal intensive care unit (NICU) and the risk of mortality or major morbidity among very preterm infants.
Study design:
Single center retrospective cohort study of infants born within 23 to 29 weeks of gestational age or birth weight <1000 g admitted at a 56 bed, level III NICU. Nursing overtime ratios (nursing overtime hours/total nursing hours), nursing provision ratios (nursing hours/recommended nursing hours based on patient dependency categories) and unit occupancy rates were pooled for all shifts during NICU hospitalization of each infant. Log-binomial models assessed their association with the composite outcome (mortality or major morbidity).
Results:
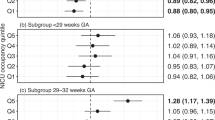
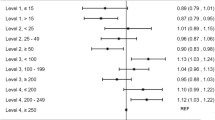
Of the 257 infants that met the inclusion criteria, 131 (51%) developed the composite outcome. In the adjusted multivariable analyses, high (>3.4%) relative to low nursing overtime ratios (⩽3.4%) were not associated with the composite outcome (relative risk (RR): 0.93; 95% confidence interval (CI): 0.86 to 1.02). High nursing provision ratios (>1) were associated with a lower risk of the composite outcome relative to low ones (⩽1) (RR: 0.81; 95% CI: 0.74 to 0.90). NICU occupancy rates were not associated with the composite outcome (RR: 0.98; 95% CI: 0.89 to 1.07, high (>100%) vs low (⩽100%)). Days with high nursing provision ratios (>1) were also associated with lower risk of having medical incidents (RR: 0.91; 95% CI: 0.82 to 0.99).
Conclusion:
High nursing provision ratio during NICU hospitalization is associated with a lower risk of a composite adverse outcome in very preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Shah PS, Lui K, Sjors G, Mirea L, Reichman B, Adams M et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr 2016; 177: 144–152.e146.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 2015; 314 (10): 1039–1051.
Chen F, Bajwa NM, Rimensberger PC, Posfay-Barbe KM, Pfister RE . Thirteen-year mortality and morbidity in preterm infants in Switzerland. Arch Dis Child Fetal Neonatal Ed 2016; 101 (5): F377–F383.
Watson SI, Arulampalam W, Petrou S, Marlow N, Morgan AS, Draper ES et al. The effects of a one-to-one nurse-to-patient ratio on the mortality rate in neonatal intensive care: a retrospective, longitudinal, population-based study. Arch Dis Child Fetal Neonatal Ed 2016; 101 (3): F195–F200.
Rogowski JA, Staiger DO, Patrick TE, Horbar JD, Kenny MJ, Lake ET . Nurse staffing in neonatal intensive care units in the United States. Res Nurs Health 2015; 38 (5): 333–341.
Drebit S, Ngan K, Hay M, Alamgir H . Trends and costs of overtime among nurses in Canada. Health Policy 2010; 96 (1): 28–35.
Canadian Association of Paediatric Health Care Centers-Canadian Paediatric Decision Support NetworkBenchmarking report 2013. Ottawa, ON, Canada; 2013.
Berney B, Needleman J . Trends in nurse overtime, 1995–2002. Policy Polit Nurs Pract 2005; 6 (3): 183–190.
Berney B, Needleman J . Impact of nursing overtime on nurse-sensitive patient outcomes in New York hospitals, 1995–2000. Policy Polit Nurs Pract 2006; 7 (2): 87–100.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES . Nurse staffing, burnout, and health care-associated infection. Am J Infect Control 2012; 40 (6): 486–490.
Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G . Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind Med 2006; 49 (11): 964–971.
Bae SH, Fabry D . Assessing the relationships between nurse work hours/overtime and nurse and patient outcomes: systematic literature review. Nurs Outlook 2014; 62 (2): 138–156.
Stone PW, Mooney-Kane C, Larson EL, Horan T, Glance LG, Zwanziger J et al. Nurse working conditions and patient safety outcomes. Med Care 2007; 45 (6): 571–578.
Olds DM, Clarke SP . The effect of work hours on adverse events and errors in health care. J Safety Res 2010; 41 (2): 153–162.
Trinkoff AM, Johantgen M, Storr CL, Gurses AP, Liang Y, Han K . Nurses' work schedule characteristics, nurse staffing, and patient mortality. Nurs Res 2011; 60 (1): 1–8.
Rogowski JA, Staiger D, Patrick T, Horbar J, Kenny M, Lake ET . Nurse staffing and NICU infection rates. JAMA Pediatr 2013; 167 (5): 444–450.
Sherenian M, Profit J, Schmidt B, Suh S, Xiao R, Zupancic JA et al. Nurse-to-patient ratios and neonatal outcomes: a brief systematic review. Neonatology 2013; 104 (3): 179–183.
Hamilton KE, Redshaw ME, Tarnow-Mordi W . Nurse staffing in relation to risk-adjusted mortality in neonatal care. Arch Dis Child Fetal Neonatal Ed 2007; 92 (2): F99–F103.
Callaghan LA, Cartwright DW, O'Rourke P, Davies MW . Infant to staff ratios and risk of mortality in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2003; 88 (2): F94–F97.
Grandi C, Gonzalez A, Meritano J . Patient volume, medical and nursing staffing and its relationship with risk-adjusted outcomes of VLBW infants in 15 Neocosur neonatal network NICUs. Arch Argent Pediatr 2010; 108 (6): 499–510.
Tucker J . Group UKNSS. Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet 2002; 359 (9301): 99–107.
Shah PS, Mirea L, Ng E, Solimano A, Lee SK Canadian Neonatal Network. Association of unit size, resource utilization and occupancy with outcomes of preterm infants. J Perinatol 2015; 35 (7):522–529.
Berney B, Needleman J, Kovner C . Factors influencing the use of registered nurse overtime in hospitals, 1995-2000. J Nurs Scholarsh 2005; 37 (2): 165–172.
Griffiths P, Dall'Ora C, Simon M, Ball J, Lindqvist R, Rafferty AM et al. Nurses' shift length and overtime working in 12 European countries: the association with perceived quality of care and patient safety. Med Care 2014; 52 (11): 975–981.
Canadian Neonatal NetworkAbstarctor's Manual v2.1.2. Available at http://www.canadianneonatalnetwork.org/portal/CNNHome/Publications.aspx; 2014.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001; 108 (2): E35.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK . SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 2001; 138 (1): 92–100.
Fédération Interprofessionnelle de la Santé du QuébecConvention collective 2011–2015, article 19.01. Quebec, Canada.
Ministère de la Santé du QuébecCatégorisation des soins neonatals en centres tertiaries. Quebec, Canada; 2012..
Gouvernement du QuébecRapport 2014–2015 des incidents et accidents survenus lors de la prestation des soins et services de santé au Québec. Available at http://msss.gouv.qc.ca/. Accessed 29 May, 2017.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82 (4): 527–532.
Papile L, Burstein J, Burstein R, Koffier A . Incidence and evolution of subependymal and intraventricular hemorrhage in pre- mature infants: a study of infants <1500gms. J Pediatr 1978; 92: 529–534.
International Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Pediatrics 1984; 74 (1):127–133.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187 (1): 1–7.
Institute for Digital Education. Regression diagnostics, Ch. 2. In: Regression with SPSS. UCLA: Los Angeles, 2016 Available at http://www.ats.ucla/.edu/stat/spss/webbooks/reg/chapter2/spssreg2.htm. Accessed 12 November, 2016.
Rothman KJ . No adjustments are needed for multiple comparisons. Epidemiology 1990; 1 (1): 43–46.
Profit J, Petersen LA, McCormick MC, Escobar GJ, Coleman-Phox K, Zheng Z et al. Patient-to-nurse ratios and outcomes of moderately preterm infants. Pediatrics 2010; 125 (2): 320–326.
Castrodale V, Rinehart S . The golden hour: improving the stabilization of the very low birth-weight infant. Adv Neonatal Care 2014; 14 (1): 9–14.
Bonner KM, Mainous RO . The nursing care of the infant receiving bubble CPAP therapy. Adv Neonatal Care 2008; 8 (2): 78–95.
van Zanten HA, Tan RN, van den Hoogen A, Lopriore E, te Pas AB . Compliance in oxygen saturation targeting in preterm infants: a systematic review. Eur J Pediatr 2015; 174 (12): 1561–1572.
Donabedian A . Evaluating the quality of medical care. Milbank Mem Fund Q 1966; 44 (3 Suppl): 166–206.
Whitfield M, Chessex P . The need for public involvement when operating a regionalized neonatal care system at maximum capacity. Paediatr Child Health 2010; 15 (9): 573–575.
Acknowledgements
We thank the staff of the Canadian Neonatal Network (CNN) Coordinating Centre, for database support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Beltempo, M., Lacroix, G., Cabot, M. et al. Association of nursing overtime, nurse staffing and unit occupancy with medical incidents and outcomes of very preterm infants. J Perinatol 38, 175–180 (2018). https://doi.org/10.1038/jp.2017.146
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.146
This article is cited by
-
Neonatal intensive care unit occupancy rate and probability of discharge of very preterm infants
Journal of Perinatology (2023)
-
Using machine learning to predict nosocomial infections and medical accidents in a NICU
Health and Technology (2023)
-
Association of timing of birth with mortality among preterm infants born in Canada
Journal of Perinatology (2021)