Abstract
Hypertension is a major health burden worldwide. However, there is limited data on the status of hypertension-mediated organ damage (HMOD) and established cardiovascular (CV) disease in Chinese hypertensive patients. The aim of this study is to determine the prevalence of HMOD and established CV disease in a nationally representative population in China. A stratified multistage random sampling method was used in the China Hypertension Survey and 21,243 participants aged 35 or older were eligible for analysis in this study. For each participant, the demographic information and a self-reported medical history were acquired. Blood pressure was measured with the electronic device 3 times on the right arm, supported at heart level, after the participant was sitting at rest for 5 min. Samples of blood and urine were tested. 2-D and Doppler echocardiography were used to assess the heart’s function and structures. Sampling weights were calculated based on the 2010 China population census data. Overall, the weighted prevalence of asymptomatic HMOD was 22.1%, 28.9%, 23.1%, 6.4%, and 6.2% for wide pulse pressure, left ventricular hypertrophy, microalbuminuria, chronic kidney disease, and abnormal ankle-brachial index, respectively. For the established CV disease, the weighted prevalence was 1.8%, 1.3%, 2.0%, and 1.1% for stroke, coronary artery disease, heart failure, and atrial fibrillation, respectively. The prevalence of asymptomatic HMOD and established CV disease was greater with higher blood pressure level (P < 0.05), rather than ankle-brachial index. Compared to those with uncontrolled hypertension, the prevalence of asymptomatic HMOD was lower in patients with controlled hypertension. In summary, the prevalence of HMOD in Chinese people aged 35 or older was very common, indicating a substantial future burden of both morbidity and mortality from hypertension in China. Clinical trial registration number: ChiCTR-ECS-14004641.
Similar content being viewed by others
Introduction
The global prevalence of hypertension was estimated to be 1.13 billion in 2015, with an alarming number of 235 million in east Asia [1]. Hypertension prevalence has been rising in China in recent decades, with up to 23.2% prevalence in Chinese people aged 18 and older, or an estimated 244.5 million individuals [2], resulting in an increase of blood pressure (BP)-related morbidity and mortality [3]. If the definition of hypertension from the 2017 ACC/AHA guideline was adopted, the prevalence of hypertension would be double, suggesting a critical burden of elevated BP in China. Furthermore, the prevalence of hypertension is expected to continue increasing with rapid economic development, urbanization, and aging.
Hypertension is the leading cause of cardiovascular (CV) disease globally [4]. It is well known that the incidence of several CV diseases, including stroke, coronary heart disease, and peripheral artery disease, is closely linking to hypertension. Meanwhile, many patients with long-term elevated BP may present with hypertension-mediated organ damage (HMOD, previously termed target organ damage), and at first without symptoms [5], including left ventricular hypertrophy (LVH), microalbuminuria, and so on, many of which are usually markers of preclinical cardiovascular disease (CVD).
Identifying HMOD could help to estimate the burden of high-CV-risk populations in the hypertensive population. Furthermore, earlier screening and intervention in HMOD may lead to more effective therapeutic strategies and reduce future CV events [5,6,7]. Since the various classes of antihypertensive agents have protective actions on end-target organs [5, 8, 9], the distribution of HMOD and CVD may differ in hypertensive patients depending on whether they use antihypertensive drugs or not. However, there is limited data on the status of HMOD and established CVD in China and worldwide. Therefore, the aim of this study is to determine the prevalence of HMOD and established CVD in a nationally representative population in China.
Methods
Survey participants
The China Hypertension Survey was conducted between October 2012 and December 2015, and the design was published previously [10, 11]. Briefly, a stratified, multistage, random sampling method was used to obtain a nationally representative sample of the general Chinese population aged 15 years or older. All 31 provinces in mainland China were covered in this survey. For this sub-study, as previously published [12], all selected urban and rural areas were stratified into eastern, middle and western regions again according to both geographical locations as well as economic strata. Using a simple random sampling method, 16 cities and 17 counties were selected. Then, at least three communities or villages were randomly selected from each city/county. To meet the designed sample size of 35,000 participants aged ≥35 years and to take nonresponse into account in the survey, 56,000 subjects were randomly selected and invited. Among these, 34,994 responded positively with a response rate of 62.5%. All the participants were examined with blood samples, electrocardiograms, and echocardiograms data. However, 6150 participants were excluded due to missing echocardiographic data, 3757 participants due to missing data on biomarkers, and 3844 individuals due to missing data on educational attainment, coronary artery disease (CAD), diabetes, peripheral artery disease (PAD), heart failure (HF), and stroke. A total of 21,243 individuals were eligible for analysis. Supplementary Table 1 showed the differences between the participants who were included and those who were not included in the subsequent analyses.
Written informed consent was obtained from each participant before data collection. The ethics committee of Fuwai Hospital approved the study.
Measurements
A standardized questionnaire developed by the coordinating center, Fuwai Hospital (Beijing, China), was administered by trained staff to obtain information on demographic characteristics and socioeconomic factors. Height was measured without shoes using a standard right-angle device and a fixed measurement tape (to the nearest 0.5 cm), and weight was measured without heavy clothing using an OMRON body fat and weight measurement device (V-body HBF-371, OMRON, Kyoto, Japan). BMI was calculated as the weight divided by height squared (kg/m2) for each participant. BP was measured 3 times on the right arm supported at heart level with the OMRON HBP-1300 professional portable BP monitor (OMRON, Kyoto, Japan) after the participant was sitting at rest for 5 min, with 30 s between each measurement. The accuracy of the Omron HBP-1300 for BP measurement had been verified in our prior study [13]. The echocardiograms were obtained using a commercially available Doppler ultrasonography, with a 3.0 MHz transducer using M-mode, 2-dimensional, spectral Doppler, and color Doppler transthoracic echocardiography with participants in the supine position. It was performed by a certified sonographer, who received a 1-month training before the study on the standardization of quantifying cardiac chambers. For each participant, a self-reported history of CVD was acquired. Peripheral blood samples were collected after an 8–10 h overnight fast and stored at −80 °C, while urine samples in the morning were collected and stored at −25 °C. Albuminuria, blood glucose, and cholesterol were measured by professional medical testing institution.
Survey outcome definitions
Overweight was defined as a body mass index (BMI) between 24.0 kg/m2 and 27.9 kg/m2, and obese was defined as a BMI of 28.0 kg/m2 or more [14]. BP was categorized as normal (systolic BP (SBP) < 120 and diastolic BP(DBP) < 80), normal high (SBP 120–139 and/or DBP 80–89) in a normal population, Grade 1 (SBP 140–159 and/or DBP 90–99), Grade 2 (SBP 160–179 and/or DBP 100–109), and Grade 3 (SBP ≥ 180 and/or DBP ≥ 110) in patients with hypertension according to the 2010 Chinese guidelines [15]. Awareness of hypertension was defined as self-report of any previous diagnosis of hypertension by a doctor. Controlled hypertension was defined as SBP < 140 mmHg and DBP < 90 mmHg in patients. Participants with a fasting plasma glucose level ≥7.0 mmol/l and/or who were receiving antidiabetic medications were defined as having diabetes. Dyslipidemia was defined as meeting any one of the following four conditions: total cholesterol ≥6.2 mmol/L; triglycerides ≥2.3 mmol/L; low levels of high-density lipoprotein cholesterol <1.0 mmol/L); or high levels of low-density lipoprotein cholesterol ≥4.1 mmol/L [16].
Asymptomatic HMOD was defined by wide pulse pressure ≥60 mmHg in older adults (aged ≥ 65 years), LVH (left ventricular mass index >50 g/m2 in men and >47 g/m2 in women), microalbuminuria (urine albumin/creatine ratio between 30 and 300 mg/g), chronic kidney disease (CKD), or an abnormal ankle-brachial index (ABI) < 0.9. CKD was defined as either decreased estimated glomerular filtration rate (eGFR; eGFR < 60 ml/min/1.73 m2) or albuminuria (urinary albumin to creatinine ratio ≥300 mg/g) according to KDIGO guidelines [17]. Moderate CKD was defined as eGFR between 30 and 59 mL/min/1.73 m2 and severe CKD was defined as as GFR < 30 mL/min/1.73 m2.
CV events, including stroke, CAD, HF and atrial fibrillation (AF), were defined based on self-reported history, which was verified with medical or hospital records. The stroke included subarachnoid hemorrhage, or a hemorrhagic or ischemic lesion in the brain. CAD was defined as previous having a myocardial infarction, or surgery for coronary revascularization. Heart failure was diagnosed according to the recommendations of the European Society of Cardiology [18, 19], with minor modifications, and defined as follows: patients with a self-reported history of HF; ejection fraction (EF) <50% and at least 6 HF symptoms; or EF ≥ 50% with moderate/severe diastolic dysfunction and at least six HF symptoms [11]. AF is diagnosed by the electrocardiograph (ECG) report or a verified AF history (possible paroxysmal AF) [20].
Statistical analysis
Variables were summarized using means for continuous data, and with frequencies, percentages, and proportions for categorical data. Two-tailed Student’s t tests and ANOVA were used to compare continuous variables and chi-square tests were used to compare categorical variables. All 95% confidence intervals (CI) for the parameters were estimated. A two-sided P < 0.05 was considered significant. Two multiple logistic regression analyses were performed to identify factors associated with HMOD and CVD. In each analysis, the following independent variables were included: age group (with 10-year intervals), sex, education, urban/rural, BMI, diabetes, dyslipidemia, and the control status of hypertension. Only the characters with β ≥ 0.5 were shown in the forest plot. Statistical analyses were conducted with SAS version 9.4 (SAS Institute INC, Cary, NC, USA) and Stata 14 (STATA Corp., TX, USA).
To represent the national population, sampling weights were calculated based on the 2010 China population census data, and the sampling scheme included an oversampling for specific age or geographic subgroups, nonresponse, and other demographic or geographic differences between the sample and the total population [21]. Adjustment for differential probabilities of selection and the complex sampling design was used to enhance the representativeness of the survey sample population. A comparison was made between participants included and excluded (Supplementary Table 1), and a sensitivity analysis under the missing at random assumption was carried out using multiple imputation.
Results
A total of 21,243 participants aged 35 years or older (50.2% women and 64.8% from rural areas) were included in the analysis. The hypertensive patients on antihypertensive medications tended to be older, women, overweight/obesity, with higher education levels, and with more complications (Table 1).
Among Chinese adults with hypertension, the weighted prevalence of asymptomatic HMOD was 22.1%, 28.9%, 23.1%, 6.4%, and 6.2% for wide pulse pressure, LVH, microalbuminuria, CKD, and abnormal ABI, respectively. For established CVD, the weighted prevalence was 1.8%, 1.3%, 2.0%, and 1.1% for stroke, CAD, HF, and AF, respectively. The prevalence of HMOD, especially for wide pulse pressure, LVH, and CKD were significantly higher in women, however, the prevalence of established CV disease was higher in men. There was no significant difference between residents living in an urban or rural area for asymptomatic HMOD and established CVD (Table 2). As expected, the prevalence of asymptomatic HMOD, as well as established CVD, was greater with older age (P < 0.05, Supplementary Tables 2, 3).
Overall, the prevalence of asymptomatic HMOD, as well as established CVD, was significantly higher in participants with hypertension. The patients who were aware of having hypertension had a higher prevalence of established CVD compared to those who were not aware of having hypertension (8.7% vs. 2.7%, P < 0.001). Furthermore, among the patients who were aware of having hypertension, the prevalence of established CVD was higher in those with antihypertensive medicines than those without antihypertensive medicines (9.5% vs. 4.7%, P < 0.001). The details of the prevalence of asymptomatic HMOD and established CV disease were presented in Table 3. Sensitivity analysis based on multiple imputation remained the similar (Supplementary Table 4).
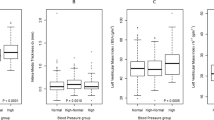
The prevalence of asymptomatic HMOD, as well as established CVD, was greater for them with higher BP level (P < 0.05), except for ABI (Fig. 1). Compared to those whose BP was not under control, the prevalence of wide pulse pressure, LVH, and microalbuminuria were lower in patients whose BP was under control (24.1% vs. 10.8%, 29.5% vs. 25.5%, and 23.3% vs. 21.8%, respectively; all P < 0.05). The difference of CKD (6.2% vs. 7.5%; P = 0.148) and abnormal ABI (6.1% vs. 6.2%; P = 0.929) did not reach the statistically significant between controlled and uncontrolled hypertension groups. For those with established CVD, we found that only the prevalence of HF was lower in patients with controlled hypertension compared to those with uncontrolled hypertension (2.0% vs. 1.9%; P = 0.936, Fig. 2).
A The weighted prevalence of hypertension-mediated organ damage in hypertensive patients by hypertension grades. B The weighted prevalence of cardiovascular diseases in hypertensive patients by hypertension grades. PP pulse pressure, LVH left ventricular hypertrophy, CKD chronic kidney disease, ABI ankle-brachial index, CAD coronary artery disease, HF heart failure, AF atrial fibrillation. Blood pressure was categorized as normal (SBP < 120 and DBP < 80), normal high (SBP 120–139 and/or DBP 80–89) in normal population, Grade 1 (SBP 140–159 and/or DBP 90–99), Grade 2 (SBP 160–179 and/or DBP 100–109), and Grade 3 (SBP ≥ 180 and/or DBP ≥ 110) in patients with hypertension according to the 2010 Chinese guidelines [15].
A The weighted prevalence of hypertension-mediated organ damage in hypertensive patients by blood pressure control status. B The weighted prevalence of cardiovascular diseases in hypertensive patients by blood pressure control status. PP pulse pressure, LVH left ventricular hypertrophy, CKD chronic kidney disease, ABI anklebrachial index, CAD coronary artery disease, HF heart failure, AF atrial fibrillation. Hypertension control was defined as SBP < 140 mmHg and DBP < 90 mmHg in patients.
The characteristics significantly associated with HMOD and CVD were different, as shown in Fig. 3. Older adults were more likely to have HMOD.
Discussion
This study reported the nationally representative estimates of HMOD and established CVD in hypertensive patients. Our study showed that the presence of HMOD in Chinese adults aged 35 or older was common, especially LVH and microalbuminuria. HF was the most common disease complicated with hypertension. Overall, the prevalence of asymptomatic HMOD was lower in patients with controlled hypertension than those with uncontrolled hypertension.
LVH is the most frequent end-organ damage associated with high BP, and it increases the risk of congestive heart failure, sudden cardiac arrest, angina pectoris, myocardial infarction, and cerebrovascular disease [22, 23]. In a meta-analysis of 30 studies on echocardiographic LVH prevalence found that, among 37,700 patients with hypertension, the prevalence of LVH was ~36% of the pooled population according to a conservative criteria [24]. In previous regional studies in China, the prevalence of LVH was between 20.2 and 42.8% among the community-based hypertensive population [25, 26]. Our study showed that the prevalence of LVH was in line with the previous studies (28.9%) and therefore suggests there may be benefitted to widely screening for LVH in hypertensive patients by ECG or, preferably, echocardiography. If necessary, antihypertensive drugs could be used to lower BP and attenuate LVH, for example angiotensin-converting enzyme inhibitors and angiotensin receptor blockers [8].
Microalbuminuria has been recognized as an early sign of renal damage, and increased microalbuminuria indicates endothelial dysfunction or developing atherosclerosis, and predicts end-organ damage, major CV events, and death [27,28,29]. The prevalence of microalbuminuria in patients with hypertension was less consistent among different study populations [30]. The result was comparable with our previous study [31]. However, the China National Diabetes and Metabolic Disorders Study reported that the prevalence of microalbuminuria in patients with hypertension, but without diabetes, was 37.4% in men and 42.7% in women [32], which was higher than our study. Shandong-Ministry of Health Action on Salt and Hypertension (SMASH) project reported that microalbuminuria was only present in 8.1% of individuals with hypertension [33]. The National Health and Nutrition Examination Survey showed that the average prevalence of microalbuminuria in US adults was 4.5% for normal BP, 6.3% for prehypertension, 12.4% for stage 1 hypertension, 25.3% for stage 2 hypertension, and 11.3% among those with treated, controlled hypertension between 1999 and 2006 [34]. The inconsistent prevalence might be caused by the population structure, definitions of microalbuminuria, and different methods of measurement. Hypertension is a major risk factor for the development and progression of CKD. One meta-analysis showed a significant reduction in all-cause mortality following BP reduction in patients with CKD [35].
The pulsatile component is pulse pressure, which depends on ventricular ejection, arterial stiffness, and timing of wave reflections. Pulse pressure has been shown as an independent risk factor for mortality or CV events in several studies in screening populations or hypertensive patients [36, 37].
Epidemiologic studies have established a strong linear relation between BP and CVD, and randomized trials have documented that BP reductions by antihypertensive drugs against HMOD and established CV disease [38, 39]. Although recent studies have fueled the debate over optimal BP targets in individuals at high-CV risk, they all confirmed the benefits of achieving the target of <140/90 mmHg [40]. Previous studies [41, 42] reported some differences between BP-lowering regimens in their effects on outcomes, and some regimens might be of greater or lesser benefit for patients with established diseases. Taken together, an increasingly important area of hypertension treatment is to identify exiting HMOD or related disease and prescribe an appropriate therapy that could reduce BP and improve patients’ symptoms and prognosis.
We found no significant difference between residents living in urban and rural areas for asymptomatic HMOD and established CV disease in this study. However, the prevalence of wide pulse pressure, CKD, and abnormal ABI were significantly higher in women, while the prevalence of established CVD was higher in men. This finding is in line with majority of previous studies [13, 24, 43].
The current results revealed that the prevalence of HMOD and CVD was higher in the patients on medication. Probably, the medicine use is related to more severe disease, possibly indicating a lack of early screening or late medical intervention in these hypertensive patients. It also may explain the higher prevalence of CVD in patients with controlled hypertension. However, it was not too late that BP control could not play a role in secondary prevention. On the contrary, HMOD was inversely related with BP controlled. It meant early intervention, even without medicine, could delay the progress of damage on the great vessels and the kidney.
This study provided significant contemporary data on the epidemiology of HMOD and established CVD in hypertensive patients in China based on a representative population. One major limitation was that the explanation of the difference between hypertensive patients taking antihypertensive medicines and those not taking antihypertensive medicines should be cautious because we were unable to identify the course of hypertension and severity of hypertension. Another limitation was that the CV events were obtained based on the self-reported history and verified with medical or hospital records, which might lead to underestimation. In addition, the cross-sectional design could not prove a causal relationship. However, as a large survey on HMOD and established CV disease in hypertensive patients, this study still provided significant epidemiological knowledge gaps for middle-income countries.
Conclusion
In summary, our study showed that the presence of HMOD in Chinese people aged 35 or older was very common. The findings suggest a substantial future burden of both morbidity and mortality from hypertension in China. National strategies should aim at reducing HMOD and established CVD in the population through improving the detection, treatment, and control of hypertension, and through population-based public health interventions to address upstream determinants of health.
Summary table
What is known about topic
-
Identifying HMOD could help to estimate the burden of high-CV-risk populations in the hypertensive population.
-
Earlier screening and intervention in HMOD may lead to more effective therapeutic strategies and reduce future CV events.
What this study adds
-
Determine the prevalence of HMOD and established CVD in a nationally representative population in China.
References
Collaboration NCDRF. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012-2015. Circulation. 2018;137:2344–56.
Bundy JD, He J. Hypertension and related cardiovascular disease burden in China. Ann Glob Health. 2016;82:227–33.
Mortality GBD, Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Kardiol Pol. 2019;77:71–159.
Katholi RE, Couri DM. Left ventricular hypertrophy: major risk factor in patients with hypertension: update and practical clinical applications. Int J Hypertens. 2011;2011:495349.
Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45:198–202.
Ruilope LM, Schmieder RE. Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens. 2008;21:500–8.
Sim JJ, Shi J, Kovesdy CP, Kalantar-Zadeh K, Jacobsen SJ. Impact of achieved blood pressures on mortality risk and end-stage renal disease among a large, diverse hypertension population. J Am Coll Cardiol. 2014;64:588–97.
Wang Z, Zhang L, Chen Z, Wang X, Shao L, Guo M, et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J Cardiol. 2014;174:721–3.
Hao G, Wang X, Chen Z, Zhang L, Zhang Y, Wei B, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015. Eur J Heart Fail. 2019;21:1329–37.
Wang Z, Wang X, Hao G, Chen Z, Zhang L, Shao L, et al. A national study of the prevalence and risk factors associated with peripheral arterial disease from China: The China Hypertension Survey, 2012-2015. Int J Cardiol. 2019;275:165–70.
Chen Z, Wang X, Wang Z, Zhang L, Hao G, Dong Y, et al. Assessing the validity of oscillometric device for blood pressure measurement in a large population-based epidemiologic study. J Am Soc Hypertens. 2017;11:730–6.
Zhou B, Coorperative Meta-Analysis Group Of China Obesity Task F. Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23:5–10.
Liu LS, Writing Group of Chinese Guidelines for the Management of H. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615.
Guideline Jcf. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15:1–29.
Holden RM, Mustafa RA, Alexander RT, Battistella M, Bevilacqua MU, Knoll G, et al. Canadian Society of Nephrology Commentary on the Kidney Disease Improving Global Outcomes 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder. Can J Kidney Health Dis. 2020;7:1–23.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur J Heart Fail. 2016;18:891–975.
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10:933–89.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr., et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:1–76.
Census Office of The State Council of China, Division of Population and Employment Statistics, National Bureau of Statistics of China. Tabulation on the 2010 population census on the People’s Republic of China. Beijing: China Statistics Press; 2012. http://www.Stats.Gov.Cn/tjsj/pcsj/rkpc/6rp/indexch.htm.
Bluemke DA, Kronmal RA, Lima JA, Liu K, Olson J, Burke GL, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55.
Devereux RB, Wachtell K, Gerdts E, Boman K, Nieminen MS, Papademetriou V, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004;292:2350–6.
Cuspidi C, Sala C, Negri F, Mancia G, Morganti A, Italian Society of H. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012;26:343–9.
Wang SX, Xue H, Zou YB, Sun K, Chun-Yan FU, Wang H, et al. Prevalence and risk factors for left ventricular hypertrophy and left ventricular geometric abnormality in the patients with hypertension among Han Chinese. Chin Med J. 2012;125:21–6.
Li H, Pei F, Shao L, Chen J, Sun K, Zhang X, et al. Prevalence and risk factors of abnormal left ventricular geometrical patterns in untreated hypertensive patients. BMC Cardiovasc Disord. 2014;14:1–7.
Volpe M. Microalbuminuria screening in patients with hypertension: recommendations for clinical practice. Int J Clin Pract. 2008;62:97–108.
Schmieder RE, Schrader J, Zidek W, Tebbe U, Paar WD, Bramlage P, et al. Low-grade albuminuria and cardiovascular risk: what is the evidence? Clin Res Cardiol. 2007;96:247–57.
Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation. 2004;110:32–5.
Zeeuw D, Parving HH, Henning RH. Microalbuminuria as an early marker for cardiovascular disease. J Am Soc Nephrol. 2006;17:2100–5.
Hao G, Wang Z, Zhang L, Chen Z, Wang X, Guo M, et al. Prevalence of microalbuminuria among middle-aged population of China: a multiple center cardiovascular epidemiological study. Angiology. 2015;66:49–56.
Xiao J, Xing X, Lu J, Weng J, Jia W, Ji L, et al. Prevalence and associated factors of microalbuminuria in Chinese individuals without diabetes: cross-sectional study. BMJ Open. 2013;3:1–10.
Yan L, Ma J, Guo X, Tang J, Zhang J, Lu Z, et al. Urinary albumin excretion and prevalence of microalbuminuria in a general Chinese population: a cross-sectional study. BMC Nephrol. 2014;15:1–9.
Ogunniyi MO, Croft JB, Greenlund KJ, Giles WH, Mensah GA. Racial/ethnic differences in microalbuminuria among adults with prehypertension and hypertension: National Health and Nutrition Examination Survey (NHANES), 1999-2006. Am J Hypertens. 2010;23:859–64.
Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5 a systematic review and meta-analysis. Jama Intern Med. 2017;177:1498–505.
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. Is pulse pressure useful in predicting risk for coronary heart Disease? The Framingham heart study. Circulation. 1999;100:354–60.
Benetos A, Rudnichi A, Safar M, Guize L. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32:560–4.
Flint AC, Conell C, Ren X, Banki NM, Chan SL, Rao VA, et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med. 2019;381:243–51.
Bohm M, Schumacher H, Teo KK, Lonn E, Mahfoud F, Mann JFE, et al. Achieved diastolic blood pressure and pulse pressure at target systolic blood pressure (120-140 mmHg) and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Eur Heart J. 2018;39:3105–14.
Wyatt CM, Cheung AK. How low can you go? Achieved blood pressure and cardiovascular outcomes. Kidney Int. 2017;92:536–9.
Boulouis G, Morotti A, Goldstein JN, Charidimou A. Intensive blood pressure lowering in patients with acute intracerebral haemorrhage: clinical outcomes and haemorrhage expansion. Systematic review and meta-analysis of randomised trials. J Neurol Neurosurg Psychiatry. 2017;88:339–45.
Lv J, Neal B, Ehteshami P, Ninomiya T, Woodward M, Rodgers A, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS Med. 2012;9:1–9.
Skurnick JH, Aladjem M, Aviv A. Sex differences in pulse pressure trends with age are cross-cultural. Hypertension. 2010;55:40–7.
Acknowledgements
We thank all the colleagues involved in the survey. The authors are grateful to OMRON Corporation, Kyoto, Japan, for supporting the BP monitor (HBP-1300) and body fat and weight measurement device (V-body HBF-371); Henan Huanan Medical Science & Technology Co., Ltd, China, for digital ECG device (GY-5000); and Microlife, Taipei, Taiwan, for the automated ABI device (Watch BP Office device). Finally, the authors are thankful to BUCHANG PHARMA, Xian, China; Kinglian Technology, Guangzhou, China; Merck Serono; Pfizer, China; and Essen Technology (Beijing) Company Limited for their support funding the project.
Funding
The study was supported by the National Key R&D Program of China during the Thirteen Five-Year Plan Period (2018YFC1315303), the CAMS Innovation Fund for Medical Sciences (2017-I2M-1-004), China National Science & Technology Pillar Program (2011BAI11B01), the National Health and Family Planning Commission, China (201402002).
Author information
Authors and Affiliations
Contributions
WZ, GR: conceived and designed the study; HG, CL, YY, and SL: drafted the paper; WX, ZL, CZ, LS, ZH, Zheng C, KY: conducted the research; WZ: revised the paper. All authors interpreted data, contributed to critical revisions, and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the Ethics Committee of Fuwai Cardiovascular Hospital (Beijing, China).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Hao, G., Chen, L. et al. Hypertension-mediated organ damage and established cardiovascular disease in patients with hypertension: the China Hypertension Survey, 2012–2015. J Hum Hypertens 36, 1092–1098 (2022). https://doi.org/10.1038/s41371-021-00635-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00635-z
This article is cited by
-
Hypertensive organ damage: the vulnerable heart of women
Journal of Human Hypertension (2023)