Abstract
Objective
Aim to reduce healthcare utilization (HU) for infants at risk of neonatal opioid withdrawal syndrome (NOWS) by 30% in 1 year and sustain for 2 years.
Study design
Baseline data from three Level I & II newborn nurseries from January 2016 to June 2018 informed PDSA cycles from August 2018 to December 2021. Shewhart process control charts evaluated length of stay (LOS), pharmacologic treatment (PT) rates, direct cost (DC), process, and balancing measures for special cause variation (SCV).
Results
Two hundred and seventeen infants showed downward SCV in LOS (12.6 to 4.4 days), PT (53% to 17%) and DC ($12593.82 to $5219.17). Onset of the COVID-19 pandemic coincided with reversible SCV. DC varied by provider specialty.
Conclusion
Transition from MFNASS to ESC led to decrease in healthcare utilization for infants at risk of NOWS. QI methodology identified persistent drivers of variability, including the COVID-19 pandemic and provider specialty.
Similar content being viewed by others
Available knowledge and rationale
Infants affected by Neonatal Opioid Withdrawal Syndrome (NOWS) are a growing patient population cared for by a variety of provider specialties [1] with costly healthcare utilization (HU) in the United States [2,3,4]. Between 2004–2014, the proportion of US births affected by neonatal withdrawal increased five-fold, to a rate of one affected infant born every 15 minutes [5]. The price of the hospital stay for a baby born with NOWS is over eight times that of an average newborn hospitalization [6, 7], and the majority of these infants are covered by Medicaid [5, 7,8,9]. Innovations to standardize and improve inpatient care of these infants, namely the introduction of the Eat, Sleep, and Console™ (ESC) bundle of care by Grossman et al. in 2017, have demonstrated reduced HU in quality improvement (QI) analyses across a variety of institutional contexts [10,11,12,13,14,15,16,17,18,19].
Local problem
Inspired by this growing body of literature, we reviewed our hospital system practice across three newborn nurseries staffed by four different provider specialties. Then, we collaborated to prioritize high-value care for NOWS-affected families during their birth hospitalization. We hypothesized that holistic analysis of system drivers with longitudinal outcomes analysis, including analysis of the direct cost of the birth hospitalization, would facilitate identification of high-yield interventions to reduce HU for infants at risk of neonatal withdrawal.
Specific aims
The primary aims of this quality improvement project were to reduce both the length of stay (LOS) and morphine exposure by 30% in one year for infants at risk of NOWS and then sustain these reductions for at least two years. A secondary aim was to determine direct cost of NOWS birth hospitalizations to inform future PDSA cycles.
Patients and methods
Context
This longitudinal QI initiative aimed to improve care for infants at risk of NOWS who were cared for during their birth hospitalization at one of three newborn nurseries in our hospital system. Site 1 is an academic level I & II nursery with an average of 3000 births per year during the study period. At Site 1, infants admitted to the newborn nursery are assigned to the care of general pediatricians, family practice physicians, or neonatologists based on the provider service schedule. Site 2 is a community level I & II nursery with an average of 770 births per year, where infants are cared for by general pediatricians, family medicine physicians or neonatologists based on a provider service schedule. Finally, Site 3 is a community Level I nursery with an average of 640 births per year, where infants are cared for by nurse practitioners, general pediatricians, or neonatologists based on a provider service schedule. At Sites 1 and 2, infants are admitted to the Level II nursery if their gestational age is less than 35 weeks or their clinical acuity warrants continuous monitoring or supplemental oxygen. At Site 3, infants are transferred to the regional Level IV NICU if they require continuous monitoring or supplemental oxygen. At each site, providers of all specialties attend to infants at all levels of care.
Prior to and throughout this quality improvement initiative, some components of the care of NOWS-affected families remained the same. Birth parents were screened for prenatal substance exposure with history questions prenatally and postnatally. If risks were identified prenatally, the birth parent was offered toxicology testing. If a positive prenatal toxicology test, prenatal opioid exposure, a history of substance abuse in the past two years, or less than four total prenatal visits were identified, urine and meconium toxicology testing of the infant was recommended postnatally. Of note, the provider chose to initiate monitoring for neonatal withdrawal based upon history and physical exam, and toxicology results were considered collateral rather than diagnostic information. Families were admitted to private rooms at all three hospital sites. If a parent was discharged before an infant was medically ready for discharge, the parent had the option to stay as a “guest” on the postpartum unit until the infant’s discharge. First-line pharmacologic management for neonatal withdrawal was oral liquid morphine with birthweight-based dosing. Infants were not discharged until they were no longer receiving morphine therapy. Upon the onset of the first wave of the COVID-19 pandemic in our region in late March 2020, infection prevention and COVID-related care policies for newborns were implemented systemwide across all three hospitals.
Interventions
In January of 2018, a multidisciplinary group of newborn care providers from these nursery sites formed a collaborative with the aim to improve care for infants at risk of NOWS systemwide. The multidisciplinary group included general pediatricians, neonatologists, obstetricians/gynecologists, family practice providers, advanced practice providers, nursing educators, bedside nurses, lactation consultants, and social workers. A key driver diagram built upon each site’s prior efforts to standardize care for this patient population and identified opportunities for systemwide change (Fig. 1). Review of baseline data from January 2016 to June 2018 informed the selection of systemwide interventions. A description of care for NOWS-affected infants during this baseline period, utilizing the Modified Finnegan Neonatal Abstinence Scoring System (M-FNASS), is provided in Supplement 1.
From July 2018 to December 2021, systemwide changes were undertaken using a PDSA framework. Iterative review of outcomes amongst stakeholders informed the selection of future PDSA cycles and allowed for root cause analysis (RCA) of unexpected changes. Interventions were adopted or abandoned by stakeholder consensus. Specifically, interventions were abandoned if they negatively impacted the project aim, increased balancing measures, or were supplanted by a new intervention.
PDSA cycles denoted as Change A, B, C, D, F and G were planned by our QI workgroup and implemented across all three nursery sites simultaneously (Table 1). Our workgroup also acknowledged other externally driven changes to the system that impacted patient care, notably the addition of more general pediatric providers and the commensurate reduction of neonatologist coverage at Site 1 (Change α) as well as the COVID-19 pandemic (Change Ɛ). A description of care for NOWS-affected infants at the conclusion of the study period (after Change G) is provided in Supplement 2.
Measures
We wanted to track outcomes for all infants that providers considered to be at risk of NOWS during their birth hospitalization. Therefore, providers and staff identified eligible infants as they were encountered in clinical care, and then inclusion was confirmed using the I2B2 Cohort Discovery Tool [20] to query problem and billing diagnoses representing substance exposure, symptomatic withdrawal, or both (coding query methodology included in Supplement 3). Patient chart data extraction was performed using Honest Broker [21]. To complete data collection, the authors manually reviewed each included clinical chart.
Infants were included if they were admitted for their birth hospitalization to Site 1, 2 or 3 between January 1, 2016 and December 31, 2021, had suspected prenatal exposure to opioids, and were postnatally monitored for neonatal withdrawal using the Modified Finnegan Neonatal Abstinence Scoring System (M-FNASS) [22] or Eat Sleep Console (ESC) [10]. Infants were excluded from outcomes analysis if they were transferred to another institution (i.e., our regional Level IV NICU) during their birth hospitalization.
Primary measures of HU for infants at risk of NOWS were LOS, utilization of pharmacologic treatment, and direct cost of the birth hospitalization. LOS was measured as admission date subtracted from discharge date.
Need for pharmacologic treatment referred to any exposure to morphine for the management of withdrawal symptoms during the infant’s birth hospitalization. Before August of 2018, three consecutive M-FNASS scores of greater than 8 or two greater than 12 were considered criteria for morphine pharmacotherapy (see Supplement 1 for M-FNASS-based management algorithm). After August of 2018, two consecutive ESC scores containing at least one “no” prompted a huddle to discuss options, including morphine pharmacotherapy (see Supplement 2 for ESC-based management algorithm).
The direct cost of a NOWS-affected birth hospitalization was tracked as a holistic measure of change impact. We did not apply a hospital-wide cost-to-charge ratio to a total newborn hospitalization charge due to the concern that newborn nurseries are unique “cost centers” within larger institutions [23, 24]. Instead, charges and clinically relevant information were extracted from the electronic health record (EHR) Epic (Epic Systems Corporation, Verona, WI) [25], McKesson Cost Accounting (McKesson Provider Technologies, Alpharetta, GA) [26] and Health Catalyst (Health Catalyst, South Jordan, Utah) [27] were used to calculate costs incurred in the provision of direct patient care. For example, the cost of nursing services, medical supplies, diagnostic imaging, rehabilitation, and food services are included in “direct cost.” “Indirect cost” or “overhead” was not included, such as the cost of hospital administration, maintenance of health records, information technology, physical plant and maintenance, human resources, volunteer services, and capital expenses. Purchased medical services (i.e., the cost to the hospital system for contracting with a particular provider group’s presence at a particular hospital site) were excluded from direct cost in this analysis, given that each site had unique financial and contractual obligations for physician coverage. Direct costs were not adjusted for inflation.
Process measures tracked throughout the study included site of admission, specialty of the discharging provider, number of morphine doses received, and highest morphine dose received. Process measures that were tracked for a portion of the study but not the complete study period included parental presence at the infant’s bedside (not documented in the EHR until after August 2018), provider compliance with morphine weaning algorithm, and presence or absence of social work consult. Additionally, the rate of infants born at risk of NOWS/100 live births across the three nurseries, regardless of subsequent admission or transfer to a higher level of care, was tracked on a U’ Chart to inform subgrouping of other process control charts.
Balancing measures included clinical concern for seizure activity, adverse medication events (defined as apnea, bradycardia, or desaturation suspected to be due to medication dose administration), and readmission for NOWS within 30 days of birth hospitalization discharge. In addition, transfers to a higher level of care were also tracked as a balancing measure, although these patients’ outcomes were not included in the remainder of the study analysis. This ensured that any potential change in patient transfer patterns after the implementation of nursery process changes would be recognized.
Analysis
The care of infants between January 2016 and June 2018 provided baseline data, at which point control limits were fixed on Shewart process control charts enabling us to look for special cause variation (SCV) over time [28]. Once SCV was identified, control limits were re-calculated to detect significant subsequent change. Primary outcome, process, and balancing measures were trended quarterly on process control charts for the overall study population and by provider specialty using Excel QI Macros (KnowWare International Inc, Denver, CO) [29]. Montgomery rules were used to define special cause variation (SCV) [30]. Outliers were excluded from analysis when the result exceeded the upper or lower control limit and was determined by group consensus to represent a unique situation not applicable to the remainder of the data.
Ethics
This project was deemed in accordance with the Declaration of Helsinki by our institutional review board (IRB), and informed consent was waived.
Results
We identified 239 infants, and 217 were included in outcomes analysis. Two infants were excluded due to lack of withdrawal scoring after birth. Twenty infants were excluded due to transfer to another institution. The most common reason for transfer was respiratory distress or failure, which is consistent with the transfer pattern for our system’s entire newborn population. Supplement 4 characterizes the study cohort.
Table 1 shows changes initiated by this project and those driven by external forces which impacted this patient population. All project-led interventions were ultimately beneficial to project aims and adopted. Simply educating multidisciplinary staff regarding ESC (Change A) before ESC implementation (Change B) was followed by downward SCV in LOS. Transition from scheduled to PRN morphine dosing (Change C) was the most effortful culture change for our hospital system, and did require re-education and re-emphasis in the management algorithm (Change F) prior to successful adoption.
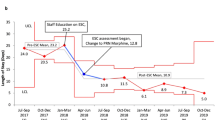
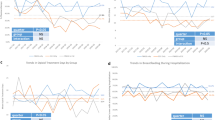
Through these iterative systemwide changes, this patient population experienced a 65% reduction in LOS (Fig. 2A, B), a 36% reduction in infants receiving morphine for treatment of neonatal withdrawal (Fig. 2C), and a 59% reduction in direct cost of the birth hospitalization (Fig. 2D, E) from baseline HU rates. Sustained reduction in HU was interrupted by reversible SCV coinciding with the onset of COVID-19 in our region (Ɛ). Before, during and after COVID-19-related process changes, reduction in HU varied by provider specialty.
A X-bar chart shows average quarterly LOS for infants at risk of NOWS across all three nursery sites from Jan 2016-Dec 2021. SCV occurred (A and D). B S Chart shows standard deviation in quarterly average LOS. SCV occurred (B and D). C P-chart of proportion of NOWS-affected infants who received pharmacologic management. SCV occurred (B). D X-bar chart shows average direct cost per birth hospitalization for infant at risk of NOWS. SCV occurred (D). E S chart shows standard deviation in quarterly average direct cost per birth hospitalization. SCV occurred (D). A multidisciplinary education regarding ESC; B ESC management implemented; C PRN morphine introduced; D MFNASS removed; Ɛ First wave of COVID-19 in our region (outlier); F Scheduled morphine removed; G Exposure-specific monitoring period.
As seen in Fig. 2A, systemwide LOS during the baseline data collection period was 12.6 days. Downward SCV in LOS occurred with education about ESC (Change A) to 7.9 days, and again to 4.4 days after removal of M-FNASS scoring from the EHR (Change D). Standard deviation in LOS demonstrated downward SCV with implementation of ESC (Change B) and removal of M-FNASS from the EHR (Change D) (Fig. 2B). For infants at risk of NOWS cared for by general pediatricians, downward SCV in LOS occurred after implementation of ESC (Change B). No sustained shifts in LOS occurred for other provider specialties throughout the study period (Fig. 3; Supplement 5).
A Quarterly Average Length of Stay (LOS) for infants at risk of NOWS plotted by Provider Specialty Jan 2016-Dec 2021. B Percent of Infants at Risk of NOWS treated pharmacologically plotted quarterly by provider specialty. C Average direct cost of a birth hospitalization for an infant at risk of NOWS plotted quarterly by provider specialty. A multidisciplinary education regarding ESC; B ESC management implemented; C PRN morphine introduced; D MFNASS removed; Ɛ First wave of COVID-19 in our region; F Scheduled morphine removed; G Exposure-specific monitoring period.
The percentage of infants at risk of NOWS who received morphine during their birth hospitalization averaged 53% during the baseline data collection period and demonstrated downward SCV after implementation of ESC (Change B) to an average of 17%. For infants at risk of NOWS cared for by general pediatricians, downward SCV in percentage treated pharmacologically occurred after implementation of ESC (Change B). No sustained shifts in pharmacologic utilization occurred for infants cared for by other specialties (Fig. 3; Supplement 5).
Direct cost per birth hospitalization for an infant at risk of NOWS averaged $12,593.82 with an average standard deviation of $13,227.75 during the baseline data collection period. There was significant variability in average direct cost during the baseline data collection period, evidenced by the average standard deviation of direct cost exceeding the average direct cost (Fig. 2D, E). Both direct cost and variability in direct cost decreased after implementation of systemwide interventions, ultimately demonstrating downward SCV with removal of M-FNASS from the EHR (Change D) to an average direct cost of $5219.17 ± $1518.04. For infants cared for by general pediatricians, downward SCV occurred after general pediatrics faculty expansion at Site 1 (α). No sustained shifts in direct cost occurred for infants cared for by other specialties (Fig. 3; Supplement 5). Notably, 213 (98%) of birth hospitalizations had definitive direct cost data extracted. The direct cost for four infants was estimated based upon manual chart review and contemporary comparables. All four of these birth hospitalizations occurred during the baseline data period.
Systemwide LOS, percent receiving morphine, and direct cost of the birth hospitalization all demonstrated unexpected SCV in April-June 2020, after the onset of the COVID-19 pandemic in our region (demarcated as Ɛ in Fig. 2). This unanticipated change prompted a RCA, targeted re-education, and inspired selection of the subsequent PDSA “Change F.” After sequential review of outcomes, Apr-June 2020 was determined to be an outlier and was removed from center line calculations for overall LOS, pharmacologic treatment and direct cost.
Notably, infants cared for by general pediatricians across all sites experienced downward SCV in primary outcomes and did not experience an Apr-June 2020 (Ɛ) increase in HU. This is demonstrated in Fig. 3, which displays quarterly averages of each primary outcome by specialty of the discharging provider. For specialty-specific process control charts, see Supplement 5.
Throughout this quality improvement initiative, an increase in number or frequency of balancing measures was not detected (Table 2). However, downward SCV in number of at-risk infants born within our health system coincided with onset of the COVID-19 pandemic (Supplement 6).
Discussion
Iterative improvement efforts to prioritize nonpharmacologic care for families at risk of NOWS accomplished our aim of sustained HU reduction across three Level I and II nursery sites and multiple provider groups. A longitudinal examination of LOS, pharmacologic treatment utilization, and direct cost per birth hospitalization allowed us to distinguish which interventions impacted each marker of HU. It also identified variability across provider specialties and an unexpected increase in HU coinciding with the COVID-19 pandemic, revealing additional lessons that may be relevant to other centers embarking upon this work.
Our analysis corroborates the experience of other authors and institutions who have documented marked reduction in HU for infants at risk of NOWS by centering nonpharmacologic management and implementing ESC [10, 12,13,14,15,16,17,18,19, 23, 31,32,33,34,35]. The need for pharmacologic management prolongs LOS [36, 37], and LOS is often assumed to correlate with birth hospitalization cost for infants affected by NOWS. In our data, these variables are clearly related. Infants who required pharmacologic management comprised 38.7% of the study patient population but accounted for 69.1% of the total LOS and 71% of the total direct cost. However, our data contradict the assumption that these outcomes are concurrently responsive to the same interventions. LOS demonstrated downward SCV after education regarding ESC (Change A), while the need for pharmacologic treatment demonstrated SCV after implementation of ESC (Change B). Direct cost did not show SCV until removal of M-FNASS from the EHR. We postulate that direct cost is a more holistic indicator of HU compared to LOS or pharmacologic use, encompassing not only NOWS-related clinical decisions but also factors such as management of co-morbidities and billing practices, and that this may have delayed its reduction in comparison to other healthcare outcomes. Other institutions could consider removing prior scoring systems from their EHR to effectively standardize and reduce HU for infants at risk of NOWS.
HU for infants at risk of NOWS varied between provider specialties, even after systemwide PDSA cycles. Other authors have reported a reduction in NICU transfers associated with prioritization of nonpharmacologic management, rooming-in practices, and implementation of ESC [10,11,12,13,14, 23]. However, we are unaware of prior studies questioning how provider specialty may impact the care of infants within newborn nursery settings.
General pediatricians cared for an increasing proportion of infants at risk of NOWS over the study period. Throughout our study, infants cared for by general pediatricians experienced a reduction in HU, which exceeded the project aim with the least variability of all provider specialties. In addition, HU for infants cared for by general pediatricians demonstrated downward SCV in all primary outcomes over the study period and did not experience upward SCV after the onset of the COVID-19 pandemic, in contrast to infants cared for by other specialties (Fig. 3; Supplement 5).
We do not believe this reflects an inherent or unique ability among individual general pediatricians; instead, this suggests that providers of different specialties may experience different barriers to providing high-value care to NOWS-affected infants in our health system. For example, the continued use of scheduled morphine rather than PRN morphine by neonatology providers after Change C was identified during Spring 2020 RCA as a potential contributor to unexpectedly high HU outcomes. Ultimately, this driver of variability responded to targeted re-education and algorithm modification (Change F removed any reference to scheduled morphine in the systemwide algorithm). Additionally, an unintentional source of downward SCV in direct cost occurred after the expansion of general pediatrics providers at Site 1 decreased neonatology provider presence at that site (α), likely also reflecting a provider specialty influence on HU. Clearly, opportunity remains to understand practice variation between specialties within the newborn nursery provider population. Provider specialty may be a valuable process measure for other institutions engaged in similar QI projects, and an interesting lens with which to examine barriers to high-value care.
The longitudinal nature of this QI initiative also captured the impact of the COVID-19 pandemic on HU for NOWS-affected infants. Our hospital system had achieved a significant and sustainable decrease in HU for NOWS-affected infants until April to June of 2021. At that time, dramatic and unintended upward SCV in all three primary outcomes was noted.
We identified multiple factors disrupting high-quality nonpharmacologic care for NOWS-affected infants during this time within our hospital system. For example, parents of NOWS-affected infants faced unprecedented challenges to remain in the hospital with their infant for the duration of their infant’s stay, including securing childcare for other children at home, abiding by infection control prevention measures at the birth hospital as well as inpatient and outpatient substance use treatment facilities, and obtaining transportation to and from the hospital. Our hospital system also underwent significant change, with multiple general pediatric and family medicine practitioners temporarily transferring the care of their newborn patients to in-house neonatal hospitalist or neonatologist care teams to reduce traffic within the hospital. Each of these factors was identified by our project stakeholders as potential contributors to increased HU for infants at risk of NOWS.
HU outcomes recovered to at, or lower than, pre-pandemic levels in July-September 2020 after Change F and have sustained with low variability through December 2021. Due to this pattern, we ultimately deemed April-June 2020 to be an outlier in our data during a time of significant system flux. If excluding consideration of April–June 2020 as an outlier, we can more clearly appreciate the impact of removal of the M-FNASS from the EHR (Change D) and PRN morphine dosing (Change C and F). These changes were followed by outcome measures, and variability in outcome measures, at their lowest levels yet systemwide. It should be noted that this reduction of HU and variability also coincided with the highest proportion of infants at risk of NOWS cared for by general pediatricians seen throughout the study period.
Limitations
The incremental framework of quality improvement must acknowledge the overlapping impact of multiple interventions. In our project, infants were scored with both M-FNASS and ESC from August 2018 until December 2019, but ESC guided provider management decisions. In the process control charts for this study, we have counted this time as “ESC implemented.” This overlap revealed the impact of removing M-FNASS from the EHR after ESC was already implemented, which was followed by downward SCV indirect cost. This information may be useful to other institutions transitioning from one scoring system to another.
We appreciated differing levels of HU variability across provider specialties. Therefore, we must acknowledge that having a greater proportion of at-risk infants cared for by general pediatricians as the study period progressed may have contributed to overall decreased HU in addition to the impact of individual PDSA cycle interventions. While a minority of the infants in our study were cared for by specialties other than pediatrics, particularly in the later years of our study, strength of QI methodology is that it allows us to learn from rather than disregard these less frequent but persistent drivers of variability. We did not examine differences in the co-morbidities of individual patients or the clinical acuity between specialties because we aimed to improve systemwide processes for all infants at risk of neonatal withdrawal. Marked differences would be unlikely given that all infants were cared for in the same Level I and II nurseries.
Throughout our study period, the number of births of infants at risk of NOWS has vacillated. After the onset of the COVID-19 pandemic in March 2020, the rate demonstrated unanticipated downward SCV (Supplement 6). The reason for a decrease in NOWS-affected births after the onset of COVID-19 is unknown, and worthy of further study. It is unknown if this reflects an actual decrease in the incidence of this pathology or perhaps under-detection of at-risk infants because of disruptions to the healthcare of pregnant people after onset of the COVID-19 pandemic.
Finally, we did not have patient representation in a decision-making capacity on our project leadership team, which may have impaired our ability to perceive patient-centered opportunities to improve.
Conclusion
QI methodology provided an enduring framework for our hospital system to reduce HU for infants at risk of NOWS, and recognize drivers of persistent variability in care. Attention to practice variation between newborn nursery provider specialties, and unintended impacts of COVID-19-related hospital processes, deserve attention in future studies of this patient population.
Data availability
The dataset compiled and analyzed in this project is not publicly available to safeguard patient privacy.
References
Keels EL, Goldsmith JP. AAP COMMITTEE ON FETUS AND NEWBORN. Neonatal Provider Workforce. Pediatrics. 2019;144:e20193147. https://doi.org/10.1542/peds.2019-3147.
Ramphul K, Mejias SG, Joynauth J. An update on the burden of neonatal abstinence syndrome in the United States. Hosp Pediatr. 2020;10:181–4. https://doi.org/10.1542/hpeds.2019-0221.
Hageman JR. The magnitude of the opioid epidemic and what we can do to help. Pediatr Ann. 2018;47:e381–2. https://doi.org/10.3928/19382359-20180919-04.
Ko JY, Patrick SW, Tong VT, Patel R, Lind JN, Barfield WD. Incidence of neonatal abstinence syndrome - 28 States, 1999-2013. MMWR Morb Mortal Wkly Rep. 2016;65:799–802. https://doi.org/10.15585/mmwr.mm6531a2.
National Institute on Drug Abuse. Dramatic Increases in Maternal Opioid Use and Neonatal Abstinence Syndrome. United States of America: National Institutes of Health; 2019 January. Available from https://archives.drugabuse.gov/trends-statistics/dramatic-increases-in-maternal-opioid-use-neonatal-abstinence-syndrome.
Centers for Disease Control and Prevention. Data and Statistics about Opioid Use During Pregnancy. United States of America: Department of Health and Human Services; 2021 July 16. Available from https://www.cdc.gov/pregnancy/opioids/data.html.
Healthcare Cost and Utilization Project. HCUP Fast Stats - Neonatal Abstinence Syndrome (NAS) Among Newborn Hospitalizations. United States of America Department of Health and Human Services: Agency for Healthcare Research and Quality; 2021 September 8. Available from https://www.hcup-us.ahrq.gov/faststats/NASServlet.
Strahan AE, Guy GP Jr, Bohm M, Frey M, Ko JY. Neonatal abstinence syndrome incidence and health care costs in the United States, 2016. JAMA Pediatr. 2020;174:200–2. https://doi.org/10.1001/jamapediatrics.2019.4791.
Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and costs of neonatal abstinence syndrome among infants with medicaid: 2004-2014. Pediatrics. 2018;141:e20173520. https://doi.org/10.1542/peds.2017-3520.
Grossman MR, Berkwitt AK, Osborn RR, Xu Y, Esserman DA, Shapiro ED, et al. An initiative to improve the quality of care of infants with neonatal abstinence syndrome. Pediatrics. 2017;139:E20163360. https://doi.org/10.1542/peds.2016-3360.
Ryan KS, Moyer A, Glait M, Yan K, Dasupta M, Saudek K, et al. Correlating scores but contrasting outcomes for eat, sleep console versus modified finnegan. Hospital Pediatr. 2021;11:350–7. https://doi.org/10.1542/hpeds.2020-003665.
Achilles JS, Castaneda-Lovato J. A Quality Improvement Initiative to Improve the Care of Infants Born Exposed to Opioids by Implementing the Eat, Sleep, Console Assessment Tool. Hosp Pediatr. 2019;9:624–31. https://doi.org/10.1542/hpeds.2019-0144.
Wachman EM, Grossman M, Schiff DM, Philipp BL, Minear S, Hutton E, et al. Quality improvement initiative to improve inpatient outcomes for Neonatal Abstinence Syndrome. J Perinatol. 2018;38:1114–22. https://doi.org/10.1038/s41372-018-0109-8.
Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A Novel Approach to Assessing Infants With Neonatal Abstinence Syndrome. Hosp Pediatr. 2018;8:1–6. https://doi.org/10.1542/hpeds.2017-0128.
Dodds D, Koch K, Buitrago-Mogollon T, Horstmann S. Successful Implementation of the Eat Sleep Console Model of Care for Infants With NAS in a Community Hospital. Hosp Pediatr. 2019;9:632–8. https://doi.org/10.1542/hpeds.2019-0086
MacMillan KDL. Neonatal Abstinence Syndrome: Review of Epidemiology, Care Models, and Current Understanding of Outcomes. Clin Perinatol. 2019;46:817–32. https://doi.org/10.1016/j.clp.2019.08.012.
MacVicar S, Kelly LE. Systematic mixed-study review of nonpharmacological management of neonatal abstinence syndrome. Birth. 2019;46:428–38. https://doi.org/10.1111/birt.12427.
Minear S, Wachman EM. Management of Newborns with Prenatal Opioid Exposure: One Institution’s Journey. Clin Ther. 2019;41:1663–8. https://doi.org/10.1016/j.clinthera.2019.07.001.
Parlaman J, Deodhar P, Sanders V, Jerome J, McDaniel C. Improving Care for Infants With Neonatal Abstinence Syndrome: A Multicenter. Community Hospital-Based Study Hosp Pediatr. 2019;9:608–14. https://doi.org/10.1542/hpeds.2019-0083.
i2b2 Cohort Discovery Tool [software], Version 1.7.12. Boston, MA: Partners HealthCare System, Boston, MA; released Dec 2019. https://www.i2b2.org/.
Honest Broker [software], Version 2.0. Clinical and Translational Science Institute of Southeast Wisconsin Bioinformatics Team, Milwaukee, Wisconsin; released Oct 2019. https://ctsi.mcw.edu/ctri/resources/bmi-links/.
Finnegan LP. Neonatal abstinence syndrome: assessment and pharmacotherapy. In: Nelson N, editor. Current therapy in neonatal-perinatal medicine. 2 ed. Ontario: BC Decker. 1990:262–70.
Holmes AV, Atwood EC, Whalen B, Beliveau J, Jarvis JD, Matulis JC, et al. Rooming-In to Treat Neonatal Abstinence Syndrome: Improved Family-Centered Care at Lower Cost. Pediatrics. 2016;137:e20152929. https://doi.org/10.1542/peds.2015-2929.
Sun Y, Friedman B. Tools for More Accurate Inpatient Cost Estimates with HCUP Databases, 2009. HCUP Methods Series Report # 2011-04. ONLINE October 29, 2012. Errata added October 25, 2012. U.S. Agency for Healthcare Research and Quality. Available from: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
Epic [software]. Verona, WI: Epic Systems Corporation; last institutional update Nov 2021. https://www.epic.com/software.
McKesson Business Analytics [software], Version 22.0. Alpharetta, GA: McKesson Provider Technologies; Released 2019. https://mms.mckesson.com/content/our-services-solutions/financial-services/.
Health Catalyst [software], Version 14.28. South Jordan, Utah: Health Catalyst; Released 2021. https://www.healthcatalyst.com/.
Provost LP, Murray SK. The Health Care Data Guide: Learning from Data for Improvement. San Francisco: Jossey-Bass; 2011. pp. 113.
QI Macros for Excel [software], Version 2022.04. Denver, CO: KnowWare International Inc; Released Apr 2022. https://www.qimacros.com/.
Montgomery, DC Introduction to Statistical Process Control, 4th edition. John Wiley & Sons; 2007. pp 172–5.
Blount T, Painter A, Freeman E, Grossman M, Sutton AG. Reduction in Length of Stay and Morphine Use for NAS With the “Eat. Sleep, Console” Method Hosp Pediatr. 2019;9:615–23. https://doi.org/10.1542/hpeds.2018-0238.
Tobon AL, Habecker E, Forray A. Opioid Use in Pregnancy. Curr Psychiatry Rep. 2019;21:118. https://doi.org/10.1007/s11920-019-1110-4.
Grisham LM, Stephen MM, Coykendall MR, Kane MF, Maurer JA, Bader MY. Eat, Sleep, Console Approach: A Family-Centered Model for the Treatment of Neonatal Abstinence Syndrome. Adv Neonatal Care. 2019;19:138–44. https://doi.org/10.1097/ANC.0000000000000581.
Thiessen P. Neonatal abstinence syndrome – a better way. Paediatr Child Health. 2018;23:428. https://doi.org/10.1093/pch/pxy092.
Howard MB, Schiff DM, Penwill N, Si W, Rai A, Wolfgang T, et al. Impact of Parental Presence at Infants’ Bedside on Neonatal Abstinence Syndrome. Hosp Pediatr. 2017;7:63–9. https://doi.org/10.1542/hpeds.2016-0147.
Wachman EM, Minear S, Hirashima M, Hansbury A, Hutton E, Shrestha H, et al. Standard Fixed-Schedule Methadone Taper Versus Symptom-Triggered Methadone Approach for Treatment of Neonatal Opioid Withdrawal Syndrome. Hosp Pediatr. 2019;9:576–84. https://doi.org/10.1542/hpeds.2018-0165.
Zankl A, Martin J, Davey JG, Osborn DA. Opioid treatment for opioid withdrawal in newborn infants. Cochrane Database Syst Rev. 2021;Issue 7:CD002059. https://doi.org/10.1002/14651858.CD002059.pub4.
Acknowledgements
The authors thank Jean Lambert, RN, PMP, MBA of Froedtert Health, for her assistance with collection and interpretation of direct cost data.
Funding
No funding was secured for this study. Data collection tools used in this project were funded in part by the Advancing a Healthier Wisconsin endowment at the Medical College of Wisconsin and the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 5UL1TR001436-02. Contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
The authors of this manuscript (MG, AM, KS, EC, and KR) conceptualized and designed this quality improvement study, designed the data collection instruments, collected and analyzed the data, iteratively shared data with multidisciplinary stakeholders, drafted, reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Glait, M., Moyer, A., Saudek, K. et al. Addressing drivers of healthcare utilization for neonatal opioid withdrawal syndrome. J Perinatol 43, 392–401 (2023). https://doi.org/10.1038/s41372-022-01533-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01533-z