Abstract
Objective
Routine blood gas measurements are common in infants with severe bronchopulmonary dysplasia (sBPD) and are a noxious stimulus. We developed a guideline-driven approach to evaluate the care of infants with sBPD without routine blood gas sampling in the chronic phase of NICU care (after diagnosis at 36 weeks PMA).
Study design
We examined blood gas utilization and outcomes in our sBPD inpatient care unit using data collected between 2014 and 2020.
Results
485 sBPD infants met inclusion criteria, and 303 (62%) never had a blood gas obtained after 36 weeks PMA. In infants who had blood gas measurements, the median number of total blood gases per patient was only 4 (IQR 1–10). We did not identify adverse effects on hospital outcomes in patients without routine blood gas measurements.
Conclusions
We found that patients with established BPD could be managed without routine blood gas analyses after 36 weeks PMA.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is the most common complication of preterm birth, affecting approximately 50% of infants born < 30 weeks gestation [1, 2]. BPD is defined as a need for respiratory support at 36 weeks post-menstrual age (PMA) in infants born at < 32 weeks gestation [3]. Severity of disease is described by 3 grades, where grades 2 and 3 are considered severe BPD due to the need for positive pressure respiratory support at 36 weeks PMA [3]. Advances in neonatal intensive care have improved survival in very low birthweight (VLBW) and extremely preterm (EP) infants [4, 5]. However, as survival has increased, the rates of BPD have also increased [1]. These increases have occurred despite the development of multiple interventions that have been associated with reduced risk of BPD, including non-invasive respiratory support, surfactant, gentle invasive ventilation, and skin-to-skin care [6,7,8].
BPD is associated with increased mortality and long-term morbidities, including neurodevelopmental impairment (NDI) [9, 10]. The mechanisms underlying the association between BPD and NDI are controversial, but may include exposure to inflammation, hypoxia, infection, and illness severity [11, 12]. Additionally, infants with BPD have longer neonatal intensive care unit (NICU) length of stay (LOS) and are exposed to greater numbers of noxious stimuli, more neurosedative medications, and fewer positive interactions than those without BPD [13]. Typical NICU patients endure significant numbers of painful procedures [14] and recent evidence suggests that exposure to noxious stimuli is independently associated with NDI [15]. Contemporary chronic care models in the NICU for severe BPD emphasize reducing exposure to noxious stimuli to reduce the risk of NDI [16,17,18]. The most frequent noxious stimuli that preterm infants experience is the heel lance, often to obtain blood gases [17], and some studies in preterm infants suggest that blood gas sampling is painful, costly, and potentially inaccurate [19, 20]. However, routine blood gas sampling is a common NICU practice with some centers reporting universal routine blood gas screening of patients with BPD after 36 weeks PMA [21, 22].
We have developed a multidisciplinary guidelines-driven treatment approach built on the principles of chronic care for patients with established severe BPD that emphasizes: (1) chronic phase ventilation, (2) nutrition, and (3) optimizing neurodevelopment by minimizing exposures that interfere with brain development [17, 18]. One way to minimize noxious stimuli that we have adopted is elimination of routine blood gas measurements after 36 weeks PMA. There are no accepted standards for when a blood gas measurement is clinically indicated in established severe BPD, therefore blood gases are ordered for clinical indications at the discretion of the attending physician in our BPD NICU. In our BPD NICU these clinical indications may involve an unexpected clinical change, prolonged non-response to therapies, and/or at the request of sub-specialty consultants, but there are no established protocols or guidelines in our BPD NICU for obtaining clinically indictated blood gases. The objective of this observational study was to (1) determine how the elimination of routine blood gas measurements has affected our use of “clinically indicated” blood gases in infants with severe BPD after admission to our BPD NICU and (2) to compare clinical outcomes in sBPD infants without routine blood gas measurements to those with clinically indicated blood gases.
Methods
Study population
The Nationwide Children’s Hospital (NCH) institutional review board approved this study with a waiver of consent. We performed an observational study of infants admitted to the BPD intensive care unit at NCH [10, 17, 18]. We included infants with established BPD as defined by the NICHD Neonatal Research Network [3] who were admitted between January 1, 2014 and May 30, 2020. We excluded infants with major congenital malformations or genetic syndromes. Data gathered from study subjects included demographics, birth characteristics, and clinical characteristics at 36 weeks PMA and at discharge.
Study location
The BPD NICU at NCH is a specialized 24-bed referral unit for infants with BPD. Patients are referred to our BPD NICU after the diagnosis of BPD is made at 36 weeks PMA. Patient care in the BPD NICU is informed by a guideline-driven multidisciplinary approach that emphasizes chronic phase ventilation, nutrition, and neurodevelopment care that includes minimizing exposures to noxious stimuli [10, 17, 18]. As such, our practice has evolved to eliminate routine blood gas measurements in patients with established BPD, even in those patients supported with invasive mechanical ventilation or non-invasive positive airway pressure (i.e., nasal constant positive airway pressure (CPAP), high-flow nasal cannula, non-invasive positive pressure ventilation (nIPPV)). In place of routine blood gas measurements, we assess the respiratory status of our BPD patients using serial physical exam assessments (specifically chest rise, breath sounds, and baseline work of breathing), growth parameters, tolerance of developmental therapies, and FiO2 requirements. Although, we rely primarily on these assessments, other non-invasive assessments are sometimes also used including but not limited to ventilator data (such as tidal volumes, flow-volume loops, flow scalars, etc.), respiratory severity score, and SpO2/FiO2 ratio. Respiratory support is adjusted if needed based on these non-invasive evaluations [18]. Our guidelines permit blood gas sampling for clinical indications at the discretion of the attending physician.
Study outcomes
We assessed the number of blood gas measurements done in our population after 36 weeks PMA. We also assessed the number of blood gases per patient for the entire hospitalization in the BPD NICU and the cost of blood gas measurements on the patients that had blood gases done. We also examined in-hospital outcomes including mortality, tracheostomy, and death or tracheostomy. The discharge status of survivors was recorded including LOS, PMA at discharge, discharged on room air, supplemental oxygen, positive pressure, and/or gastrostomy.
We also compared our clinical outcomes with other cohorts of BPD patients wherein care practices included blood gas sampling; we identified published cohorts that also included similar outcome metrics. Interestingly, there are a relative paucity of published cohorts of infants with established BPD. Most larger cohort studies in neonatology related to BPD have been studies on preterm infants to examine the factors associated with the development of BPD, given that these cohorts include both patients with and without BPD these data are difficult to compare to our data. However, we did find four recent publications [2, 3, 23, 24] that described similar outcomes in cohorts of infants with established BPD. Finally, to compare our results in a cohort of infants with established BPD who had no blood gases done to a cohort of infants who had routine blood gas sampling, we identified two studies [22, 25] in infants with established BPD wherein routine blood gas sampling was specified.
Statistical analysis
We analyzed descriptive statistics for demographics and clinical characteristics at 36 weeks PMA and at discharge using median and interquartile ranges [IQR] for continuous variables and number and percentages for categorical variables. The Mann-Whitney rank-sum test was used to compare continuous data and the chi-square test was used to compare categorical variables. The cost of blood gas studies were determined via the laboratory billing department. Statistical analysis was performed using R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria). All p-values are two-tailed and considered significant if p < 0.05.
Results
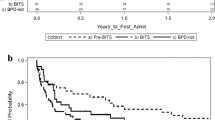
A total of 485 infants with BPD met inclusion criteria (Fig. 1). Following our guidelines to eliminate routine blood gas sampling, 303 (62% of the cohort) never had a blood gas obtained after admission to the BPD NICU. The remaining 182 (38%) infants had at least 1 clinically indicated blood gas obtained after admission to the BPD NICU. In those 182 infants with at least one clinically indicated blood gas, the median number of total blood gases obtained throughout the BPD unit hospitalization per infant was only 4, with a significant left skew of the data as demonstrated by the IQR of 1–10. In those patients that had at least one clinically indicated blood gas drawn the total additional cost of blood gas sampling was $247,860, or an average total cost for blood gases of $1362 per patient.
As expected, this cohort of infants with established BPD had relatively severe illness. They were born extremely preterm, with a median gestational age (GA) of 26 weeks [24–27 weeks] and with extremely low birth weights (BW), with a median BW of 770 grams [615–975 grams] (Table 1). Most of the cohort received antenatal steroids, were delivered by cesarean section, were intubated in the delivery room, and received postnatal surfactant (Table 1). Most patients were admitted to the Level IV NICU at NCH before reaching 36 weeks PMA (Table 1); and were then transferred to the BPD NICU at time of diagnosis of BPD at or after 36 weeks PMA. Grade 3 BPD was diagnosed in 110 infants (23%).
Outcomes for the cohort are given in Table 2. The relative disease severity in this cohort is also demonstrated by mortality rate, tracheostomy rate, and the combined outcome death or tracheostomy (Table 2). In this cohort, 20% of survivors were discharged on room air, while nearly 70% of the infants were discharged on supplement oxygen and 3% were on positive pressure at discharge (Table 2). The median LOS was 125 days [IQR, 90–188] with a median PMA of 47 weeks [IQR, 42–56] at discharge (Table 2).
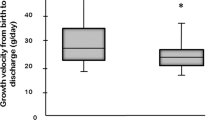
We examined differences in demographics and clinical characteristics between the infants in this cohort that never had a blood gas measurement and those infants that had at least one clinically indicated blood gas measurement as shown in Table 3. The infants that had at least one blood gas obtained may have had greater disease severity than those infants who never had a blood gas done, as suggested by the birth weight, proportion that were small for gestational age (SGA), and the proportion with grade 3 BPD (Table 3). The outcomes were also consistent with the idea that the infants that had at least one blood gas done were relatively sicker than those that never had a blood gas done as demonstrated by group differences in mortality, tracheostomy, length of stay, and PMA at discharge (Table 3).
As shown in Table 4, there were no fundamental differences in mortality, PMA at discharge, LOS, tracheostomy, or Grade 3 BPD compared to 4 other cohorts of patients with BPD described by the Children’s Hospitals Neonatal Consortium (CHNC), the NICHD Neonatal Research Network (NRN), the Vermont Oxford Network (VON), and the BPD Collaborative [2, 3, 23, 24]. It should be remembered that NCH is part of these networks. Finally, as shown in Table 5, our LOS, PMA at discharge, and duration of invasive mechanical ventilation were similar to 2 published cohorts of infants that specified routine blood gas sampling [22, 25].
Discussion
In this relatively large cohort of infants with established BPD who were cared for using a guidelines-driven approach that included eliminating routine blood gas measurements, we found that the majority of infants had no blood gases done after admission to the BPD NICU. Our data also suggest that the infants that had blood gases done may have had greater disease severity than did the infants who had no blood gases done after admission to the BPD NICU. It is interesting to note, that even in those sicker infants who had clinically indicated blood gas measurements the median number of blood gases done was only 4 during a relatively long length of stay. Our findings suggest that patients with established severe BPD can be managed without the use of routine blood gas measurements without increased adverse effects when compared to other cohorts. Moreover, the lack of routine blood gas measurements after admission to the BPD NICU in this cohort of infants with established BPD did not seem to impact liberation from respiratory support at least compared to other published cohorts of infants with established BPD. These findings support the notion that infants with established BPD can be effectively managed in the NICU after the diagnosis is made at 36 weeks PMA without routine use of blood gas measurements.
Blood gases are typically used to monitor the efficacy of ventilation in patients with BPD and to guide decisions regarding weaning or escalation of respiratory support. Recent clinical reviews by Abman et al. [16] and Gibbs et al. [26] suggest that routine physical examination, assessment of growth, and tolerance of developmental therapies may be effective in assessing adequacy of ventilation and need for changes in respiratory support in patients with established BPD. The bedside assessment of work of breathing and oxygen saturations provides important information regarding the pulmonary status of patients with established BPD [27]. In our unit, an infant with tachypnea, chest wall retractions, increased work of breathing, and agitation is considered under-supported and changes in respiratory support are made by our multidisciplinary BPD team. The effect of these changes can then be evaluated by assessing for improvements in the patient’s level of comfort, chest rise, FiO2, oxygen saturation, growth parameters, and tolerance of developmental therapies. Similarly, weaning of respiratory support can be guided by longitudinal assessments of FiO2, growth, and tolerance of developmental therapies. Routine nutrition labs are done in our unit on a weekly to monthly basis depending on patient’s nutritional status. The serum bicarbonate can be used as a surrogate to track changes in the pCO2, however we do not routinely rely on the serum bicarbonate when making changes to respiratory support. Our results also suggest that by eliminating routine blood gas sampling the multidisciplinary care team became comfortable with these non-invasive assessments, which resulted in 62% of our cohort never having a blood gas sampled after admission to the BPD NICU.
Interestingly, there were 18 patients who never had a blood gas after admission to the BPD NICU who underwent tracheostomy placement after admission. The decision to recommend a tracheostomy in an infant with severe BPD is complex and usually involves a continued need for high levels of respiratory support with marginal improvement over time or presence of airway abnormalities [28]. Recently Yallapragada et al. [29] surveyed 31 Children’s Hospitals and found that there are many qualitative indications that inform the decision to recommend a tracheostomy in patients with severe BPD. Interestingly, when asked for relative importance of indications the top 3 were: multiple extubation failures (90%), specific pCO2 values (86%), and PMA (82%) [29]. Our study suggests that pCO2 may not be a critical component of the decision to recommend tracheostomy, at least in this cohort of sBPD patients. Moreover, trending of FiO2 as well as serum bicarbonate values may provide useful longitudinal assessments of gas exchange in the chronic phase of sBPD.
To our knowledge, this is the first report of infants with established BPD who did not undergo routine blood gas sampling after the diagnosis of severe BPD is made at 36 weeks PMA. It has been reported that in one center all patients with established BPD had at least one blood gas done prior to discharge and that discharge from the NICU required a pCO2 < 60 mm Hg [21]. This practice was based on a study that found that the pre-NICU discharge pCO2 was associated with adverse post-discharge outcomes, including an increased risk of re-admission [30]. Interestingly, although some practices have been based on this notion, Dawson et al. did not observe that capillary pCO2 at 36 weeks PMA or discharge were associated with re-admission in the first year of life [21]. It is also important to remember that there are no widely accepted standards for optimal pCO2 levels in infants with BPD [31]. The optimal utility of routine blood gas determinations in established BPD requires further study.
Vinall et al. demonstrated that in a 50-member cohort of former very preterm infants a higher number of tissue-breaking procedures, including heel lances, were associated with lower fractional anisotropy on magnetic resonance imaging, a measure of white matter differentiation, and a lower IQ at a median follow up age of 7 years [32]. A secondary analysis of the Caffeine for Apnea of Prematurity trial data found that BPD was independently associated with increased odds of death or neurodevelopmental impairment at 5 years of age [9]. While the mechanisms underlying the association between BPD and neurodevelopmental impairment remain uncertain [12], there is a clear association between BPD and neurodevelopmental impairment. It is plausible that avoidance of unnecessary painful procedures, including blood gases, in patients with BPD may mitigate the risk and/or severity of neurodevelopmental impairment in early childhood, though additional prospective studies focused on long-term neurodevelopmental outcomes are needed to test this hypothesis.
Our study has important limitations. First, the retrospective, single center design of the study may potentially limit the generalizability of our findings. Second, the specific clinical circumstances surrounding blood gas sampling were not assessed. Thus, our conclusions are limited to routine blood gas sampling, and there are circumstances where clinically indicated blood gas sampling may provide important information to the clinician. Further studies are warranted to examine how to optimize the information obtained by blood gas analysis in concert with clinical assessments to develop interventions that improve outcomes in patients with established severe BPD. Lastly, our study did not examine neurodevelopmental outcomes and given the potential association between repeat blood gas sampling and NDI, future prospective studies are needed to focus on neurodevelopmental outcomes in early childhood in established severe BPD.
In conclusion, we found that patients with established severe BPD can be managed without routine blood gas analyses after 36 weeks PMA. Our results also suggest that the implementation of other measures of adequate respiratory support (FiO2, work of breathing, tolerance of therapies) in addition to the elimination of routine blood gas sampling after 36 weeks PMA may decrease overall utilization of blood gases in established severe BPD. Prospective studies are needed to determine the efficacy of alternative assessments of respiratory support across centers and BPD programs.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due patient privacy but are available from the corresponding author on reasonable request.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
Jensen EA, Edwards EM, Greenberg LT, Soll RF, Ehret DEY, Horbar JD. Severity of bronchopulmonary dysplasia among very preterm infants in the United States. Pediatrics. 2021;148:e2020030007.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171:e164396.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Jensen EA. Prevention of bronchopulmonary dysplasia: a summary of evidence-based strategies. Neoreviews. 2019;20:e189–e201.
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL. Bronchopulmonary dysplasia: NHLBI Workshop on the primary prevention of chronic lung diseases. Ann Am Thorac Soc. 2014;11:S146–153.
Bapat R, Nelin L, Shepherd E, Ryshen G, Elgin A, Bartman T. A multidisciplinary quality improvement effort to reduce bronchopulmonary dysplasia incidence. J Perinatol. 2020;40:681–7.
Schmidt B, Roberts RS, Davis PG, Doyle LW, Asztalos EV, Opie G, et al. Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. J Pediatr. 2015;167:982–6.
Bauer SE, Schneider L, Lynch SK, Malleske DT, Shepherd EG, Nelin LD. Factors associated with neurodevelopmental impairment in bronchopulmonary dysplasia. J Pediatr. 2020;218:22–27.
Trittmann JK, Nelin LD, Klebanoff MA. Bronchopulmonary dysplasia and neurodevelopmental outcome in extremely preterm neonates. Eur J Pediatr. 2013;172:1173–80.
Strunk T, Inder T, Wang X, Burgner D, Mallard C, Levy O. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infect Dis. 2014;14:751–62.
Mowitz ME, Ayyagari R, Gao W, Zhao J, Mangili A, Sarda SP. Health care burden of bronchopulmonary dysplasia among extremely preterm infants. Front Pediatr. 2019;7:510.
Johnston C, Barrington KJ, Taddio A, Carbajal R, Filion F. Pain in Canadian NICUs: have we improved over the past 12 years? Clin J Pain. 2011;27:225–32.
Ranger M, Grunau RE. Early repetitive pain in preterm infants in relation to the developing brain. Pain Manag. 2014;4:57–67.
Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuevas-Guaman M, Welty SE, et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2017;181:12–28. e11.
Shepherd EG, Knupp AM, Welty SE, Susey KM, Gardner WP, Gest AL. An interdisciplinary bronchopulmonary dysplasia program is associated with improved neurodevelopmental outcomes and fewer rehospitalizations. J Perinatol. 2012;32:33–38.
Logan JW, Lynch SK, Curtiss J, Shepherd EG. Clinical phenotypes and management concepts for severe, established bronchopulmonary dysplasia. Paediatr Respir Rev. 2019;31:58–63.
Courtney SE, Weber KR, Breakie LA, Malin SW, Bender CV, Guo SM, et al. Capillary blood gases in the neonate. A reassessment and review of the literature. Am J Dis Child. 1990;144:168–72.
King BC, Richardson T, Patel RM, Lee HC, Bamat NA, Patrick SW, et al. Cost of clinician-driven tests and treatments in very low birth weight and/or very preterm infants. J Perinatol. 2021;41:295–304.
Dawson SK, D’Andrea LA, Lau R, Lagatta JM. Using a home oxygen weaning protocol and pCO2 to evaluate outcomes for infants with bronchopulmonary dysplasia discharged on home oxygen. Pediatr Pulmonol. 2020;55:3293–303.
Shin SH, Shin JS, Kim EK, Kim HS. Capillary partial pressure of carbon dioxide for predicting rehospitalization in preterm infants under noninvasive respiratory support with severe bronchopulmonary dysplasia. Pediatr Pulmonol. 2021;56:3863–9.
Lagatta JM, Hysinger EB, Zaniletti I, Wymore EM, Vyas-Read S, Yallapragada S, et al. The impact of pulmonary hypertension in preterm infants with severe bronchopulmonary dysplasia through 1 year. J Pediatr. 2018;203:218–24.
Guaman MC, Pishevar N, Abman SH, Keszler M, Truog WE, Panitch H, et al. Invasive mechanical ventilation at 36 weeks post-menstrual age, adverse outcomes with a comparison of recent definitions of bronchopulmonary dysplasia. J Perinatol. 2021;41:1936–42.
Lagatta JM, Zhang L, Yan K, Dawson S, Msall ME, Ambalavanan N, et al. Prospective risk stratification identifies healthcare utilization associated with home oxygen therapy for infants with bronchopulmonary dysplasia. J Pediatr. 2022;251:105–12.
Gibbs K, Jensen EA, Alexiou S, Munson D, Zhang H. Ventilation strategies in severe bronchopulmonary dysplasia. Neoreviews. 2020;21:e226–e237.
Shepherd E, Nelin L Physical Examination. In: Goldsmith JP, Karotkin EH, Keszler M, Suresh GK, eds. Assisted ventilation of the neonate: an evidence-based approach to newborn respiratory care 7th edition. Philadelphia, PA: Elsevier; pp 70–75, 2022.
Mandy G, Malkar M, Welty SE, Brown R, Shepherd E, Gardner W, et al. Tracheostomy placement in infants with bronchopulmonary dysplasia: safety and outcomes. Pediatr Pulmonol. 2013;48:245–9.
Yallapragada S, Savani RC, Munoz-Blanco S, Lagatta JM, Truog WE, Porta NFM, et al. Qualitative indications for tracheostomy and chronic mechanical ventilation in patients with severe bronchopulmonary dysplasia. J Perinatol. 2021;41:2651–7.
Kovesi T, Abdurahman A, Blayney M. Elevated carbon dioxide tension is a predictor of subsequent adverse events in infants with bronchopulmonary dysplasia. Lung. 2006;184:7–13.
Wong SK, Chim M, Allen J, Butler A, Tyrrell J, Hurley T, et al. Carbon dioxide levels in neonates: what are safe parameters? Pediatr Res. 2022;91:1049–56.
Vinall J, Miller SP, Bjornson BH, Fitzpatrick KPV, Poskitt KJ, Brant R, et al. Invasive procedures in preterm children: brain and cognitive development at school age. Pediatrics. 2014;133:412–21.
Author information
Authors and Affiliations
Contributions
MJK, LCE, EGS, SEW, and LDN designed the study, collected, analyzed, interpreted the data, and drafted the manuscript. RJD, ANM, RB, and GE designed the study, interpreted the data, and critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kielt, M.J., Eldredge, L.C., Shepherd, E.G. et al. Managing established bronchopulmonary dysplasia without using routine blood gas measurements. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01955-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01955-x