Abstract
Background
The beneficial effects of folate have been observed under different conditions, but the available evidence on inflammation and reduction of cardiovascular disease (CVD) in type 2 diabetes mellitus (T2DM) is limited. The study aimed to explore the effects of folate on inflammation and homocysteine amongst individuals with T2DM.
Methods
PubMed, Scopus, and Cochrane Library were used to search for evidence. A random-effect model meta-analysis through Review Manager (version 5.4) and metaHun was performed. Results were reported as standardized mean differences (SMD) and 95% confidence intervals graphically using forest and funnel plots.
Results
Data from 9 trials with 426 patients living with T2DM were analyzed. Folic acid supplementation significantly revealed a large effect size on homocysteine levels compared to placebo, SMD = −1.53, 95%CI (−2.14,−0.93), p < 0.05. Additionally, we observed a medium marginal effect size on C-reactive protein (SMD = −0.68, 95%CI (−1.34, −0.01), p = 0.05). However, no significant effect on tumor necrosis factor-α (SMD = −0.86, 95%CI (−2.65, 0.93), p = 0.34), and interleukin-6 (SMD = −0.04, 95%CI (−1.08, 1.01), p = 0.95) was observed.
Conclusion
Evidence analyzed in this study suggests that folic acid supplementation in T2DM reduces homocysteine and may mitigate CVDs. However, its effect on inflammation is inconclusive.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a condition that elevates blood glucose, also known as hyperglycemia [1]. Patients living with T2DM are at higher risk of developing cardiovascular diseases (CVD) than healthy individuals [2]. The prevalence of diabetes worldwide in 2021 was estimated to be 10.3% and this is continually rising with estimated projections of around 12.2% in 2045 [3]. The main factors that exacerbate the development of CVD in T2DM include but are not limited to hyperinsulinemia, obesity, hypertension, hypertriglyceridemia, hypercholesterolemia, and homocysteinemia [4]. Inflammation is a central feature in T2DM, contributing to CVD among patients with T2DM. For instance, an increased circulating plasma C-reactive protein (CRP) [5, 6] is noted in patients with T2DM, which may further increase the risk of CVD. Moreover, T2DM are more likely to develop hyperhomocysteinemia primarily due to folate and vitamin B12 deficiency [7, 8]. It is noteworthy to indicate that patients with T2DM who rely on metformin to control hyperglycemia often develop hyperhomocysteinemia, which further makes them susceptible to CVDs [9].
Previous studies have reported a link between homocysteine and inflammation [10,11,12]. For instance, evidence from preclinical and clinical studies demonstrated an association between homocysteine and proinflammatory responses [10, 13]. Homocysteine is an amino acid associated with the risk of CVD if its level is elevated in the body [14]. Although homocysteine and inflammation markers are frequently detected at the same time, they are not correlated as they have revealed an inverse relationship in previous scientific evidence [8, 15]. We anticipate that measuring them simultaneously will improve the overall interpretation and understanding of their correlation in T2DM. Due to their contribution to the development of CVDs in T2DM, an approach that can reduce the circulating levels of inflammatory markers and homocysteine in T2DM can be important to ameliorate inflammation, halt cardiovascular-related complications amongst T2DM and further reduce morbidity and mortality. It is important to note that T2DM medications widely used to control hyperglycemia in T2DM are available; however, their long-term may result in vitamin B12 and folate deficiency [16, 17]. Recent evidence has shown that folate deficiency is associated with an increased level of homocysteine, increasing the risk of CVD in T2DM [18, 19]. The above shortfalls for drugs and related side effects have prompted an exploration of dietary supplements and macronutrients in alleviating cardiovascular-related complications in T2DM. Other examples include vitamin D [20], and folate, a natural form of vitamin B9 due to its pleiotropic effects in diabetes and fewer side effects than other expensive and toxic therapies [21]. Folate is primarily found in green leafy vegetables and plays a role in cell division and synthesis of nucleic acids [22].
Folate has been explored by previous studies on inflammation, focusing on CRP levels in patients with T2DM. However, the findings reported by various studies are contradictory [23, 24]. While Fatahi et al. [25] through meta-analysis, demonstrated a positive effect of folate on inflammation, the results must be treated with caution as only CRP as a marker of inflammation was assessed, and this might introduce bias, as it is difficult to conclude on the severity of inflammation based on one biomarker. Sato has reported no effect of 20 mg of folic acid on CRP and IL-6 as markers of inflammation in T2DM [15]. Additionally, the findings by Kaye et al., [26] suggest that folic acid may reduce the homocysteine levels in T2DM. However, completely different results were reported in a randomized, placebo-controlled, cross-over trial where there was no significant difference between folic acid and placebo groups on homocysteine [27]. Thus, the current study aims to systematically review and meta-analyze data from RCT to evaluate the effect of folic acid/folate on the level of homocysteine and inflammation in T2DM adult patients to rule out any inconsistencies observed in previous evidence. Furthermore, this review and meta-analysis also indicate the effective doses of folic acid/folate therapy that can alleviate inflammation among patients living with T2DM.
Methodology
This systematic review and meta-analysis are prepared and reported using an updated Preferred Reporting Items for Systematic Review and Meta-Analysis guideline [28] and checklist (Appendix 1). The protocol for this study has been registered with PROSPERO (the International Prospective Register of Systematic Reviews), CRD2023476986, for transparency.
Aim of the study
To evaluate if folic acid supplementation can ameliorate inflammation. In addition, we sought to determine the overall effect of folic acid on homocysteine in T2DM.
Information source and search strategy
A comprehensive literature search was conducted using online databases, including PubMed, Scopus, and Cochrane Library. The following medical subject headings (MeSH) and keywords were used: “Folate” OR “folic acid” OR “Folacin” OR “Vitamin B9” AND “type 2 diabetes mellitus” OR “type 2 diabetes” OR “hyperglycemia.” These search terms were adjusted to suit each database used. The search was restricted to randomized controlled trials published from inception until 15 October 2023. The search was also restricted to RCT published in English. Furthermore, the reference lists of retrieved studies were also screened for additional relevant studies. Two researchers (KM and GRM) independently screened titles and abstracts of all retrieved studies, and discrepancies were resolved through discussion and re-evaluation of the study.
Eligibility criteria
Inclusion criteria
All trials that satisfied our PICOS criteria were included (Table 1); for instance, all participants were adult patients living with T2DM, folic acid or folate treatment as an intervention, placebo as a control group, and inflammation and homocysteine levels as the outcomes of interest. Therefore, all randomized controlled trials that evaluated the effect of folic acid on concentrations of homocysteine, CRP, IL-6, and TNF-α were included.
Exclusion criteria
In case of any unavailable full-text article, we contacted the corresponding author, and if there was no response, the paper was excluded. Clinical trials using other interventions were excluded: no information about inflammation, no control groups, pregnant women, animal models of T2DM, gray literature, or other supplements were excluded.
Data items and extraction
The main researcher (KM) designed an Excel extraction sheet, and this was shared with the secondary researcher GRM prior to extraction. This Excel sheet included data items such as leading author surname, year of publication, study location, study design, population, gender distribution, mean age, mean body mass index, glycated hemoglobin, method of determining homocysteine, study duration, dosage of folic acid supplements, as the means ± standard deviation (SD) of the outcome measures in the folate/folic acid and placebo groups at baseline and post-intervention (change in values) for inflammatory markers (CRP, IL-6, and TNF-α) and homocysteine levels. The data were extracted independently by KM and GRM to minimize the risk of bias and extraction errors. Any disagreement was resolved by a third independent researcher WNP, who re-evaluated the study or data items in question.
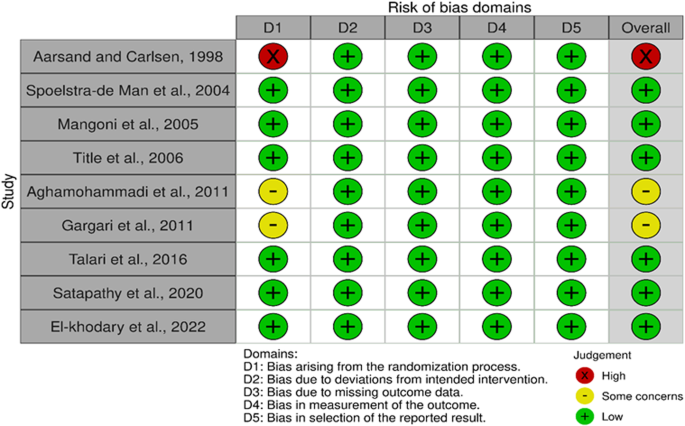
Risk of bias in individual studies
The risk of bias (ROB) across all eligible studies was assessed following the Cochrane risk of bias tool [29]. Each included trial was evaluated based on five domains: bias arising from the randomization process, bias due to deviation from intended intervention, bias due to missing outcome data, bias due to missing outcome data, bias in the measurement of the outcome, bias in the selection of the reported results. A study was judged as low risk if all domains were at low risk of bias and judged as some concern if one domain was judged as some concern. Two independent researchers (KM and GRM) made the overall judgment. In the event of disagreement, a third researcher (WNP) made a judgment of the domain in question.
Data synthesis and statistical analysis
The meta-analysis was carried out using Review Manager (RevMan Version 5.4) and Meta-Hun http://softmed.hacettepe.edu.tr/metaHUN/ (accessed on 28/10/23). Means and SD of the outcome measures (CRP, IL-6, TNF-α, and homocysteine) reported for the folate and placebo groups were used to obtain the overall estimates. Where the SD of the mean difference was not reported in the studies, we estimated it using the following formula: change in SD = √[(SD pre-treatment)2 + (SD post-treatment)2 – (2 R × SD pre-treatment × SD post-treatment)]. The correlation coefficient (R) of 0.8 was considered based on previous reports [30]. Additionally, the mean was estimated using formulae \({\rm{X}}{\rm{\bar{} }}=\frac{{\rm{a}}+2{\rm{m}}+{\rm{b}}}{4}\), and SD was estimated using \({\rm{SD}}=\frac{{\rm{range}}}{4}\) when the sample size is smaller than 70 if the trial reported median and interquartile range (IQR) [31]. In contrast, SD was estimated using the standard error of the mean (SEM) \(={\rm{SD}}\div\surd {\rm{n}}\) when the trial reported a standard error of the mean. The overall effect sizes for all effect measures were reported as standardized mean differences (SMD) and 95% confidence intervals (CI). SMD was preferred due to variables being reported in different units of measure. Random-effect model was used due to moderate heterogeneity, respectively. We further assessed heterogeneity between studies through the I2 statics test (I2 > 50%), considered as moderate heterogeneity [32, 33]. A p-value of < 0.05 was considered statistically significant, and the Cohens d was used to interpret the magnitude of the effect size. A Cohens d of 0.1, 05, and 0.8 was classified as a small, medium, and large effect, respectively. Publication bias was evaluated graphically through funnel plot inspection and statistically using Egger’s regression test. A sensitivity analysis was conducted using a leave-one-out analysis to determine each study’s effect on the overall effect size [34, 35]. The overall certainty of evidence across the studies was evaluated in accordance with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guideline [36]. The quality of evidence was classified into four categories based on the corresponding evaluation criteria: high, moderate, low, and very low.
Results
Characteristics of included studies
Nine trials [23, 24, 27, 37,38,39,40,41,42] with 426 T2DM on folate/folic acid compared to placebo were included. The intervention group had 226 patients in the T2DM compared to 201 in the placebo group. These trials were conducted in Australia [40], Canada [27], India [38], Iran [24, 38, 39, 41], Egypt [37], Norway [42] and the Netherlands [23] between 1998 and 2022. All included trials were randomized controlled trials, with one open-labeled [38], one double-blinded cross-over [27], and the rest were double-blinded trials. The sample size varied from smallest (26) to largest (100). The treatment was administered as either folate/folic acid in all trials between doses of 0.25 mg to 10 mg for a period ranging from 2 weeks to 28 weeks. At least seven trials [23, 24, 37,38,39,40,41] used folate at 5 mg for 4–26 weeks. The mean age of participants in the folate group was 59.57 ± 4.68 years, with a body mass index of 27.39 ± 3.05 kg/m2. The baseline glycated hemoglobin in the folate group was 7.67 ± 0.40%. The gender distribution across all trials was 134 males in folate and 130 in the placebo group, respectively. Different techniques were used to measure homocysteine in these trials, with the common one being an Enzyme immunoassay by homocysteine kit followed by an enzyme-linked immunosorbent assay (ELISA) kit. A detailed overview of the included trials is presented in Table 2.
Literature search
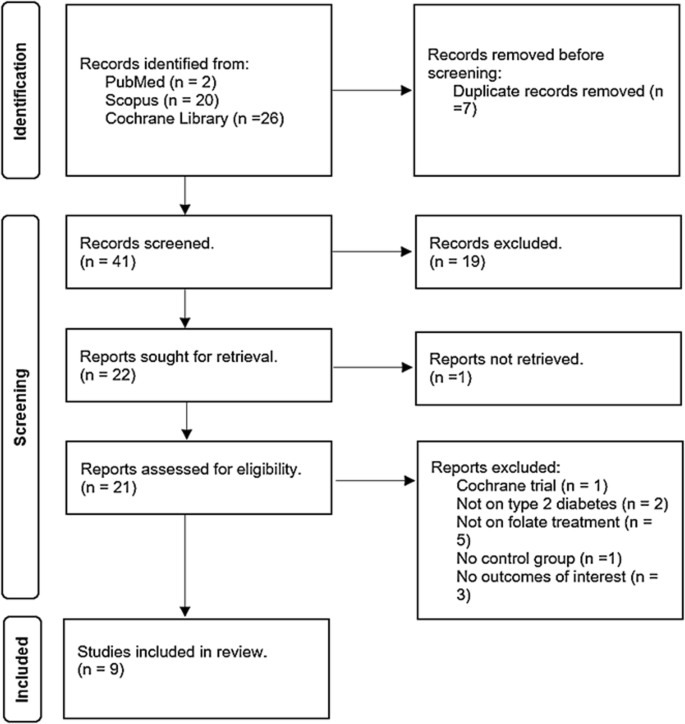
A comprehensive overview of the study selection process is presented in the PRISMA flow diagram in Fig. 1. The electronic search across three main databases, namely PubMed, Scopus, and the Cochrane Library, identified forty-eight records. PubMed contributed two records, Scopus contributed twenty, and the Cochrane Library contributed twenty-six (Table 1S). All forty-eight records were stored in the Mendeley Reference Manager (version 2.104.0). Duplicate identification revealed seven records replicated in the databases and were excluded. Consequently, forty-one unique records underwent screening by independent researchers (KM and GRM). During the initial screening based on eligibility criteria, nineteen records were deemed irrelevant due to unrelated titles, abstracts, keywords, and focus.
Among the remaining twenty-two records subjected to full screening, one was published in Chinese and was excluded to prevent potential misinterpretation upon translation to English. Of the remaining twenty-one records, five employed interventions other than folate; three did not address our specified outcomes of interest, two involved irrelevant populations as they were not T2DM, one did not have a control group, and one represented a registration for an ongoing Cochrane trial. Consequently, only nine trials met the eligibility criteria for relevance to our study.
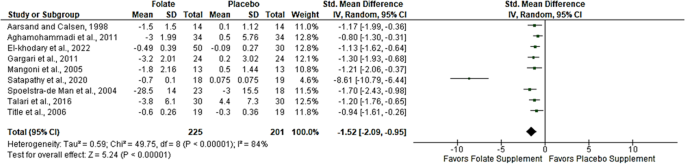
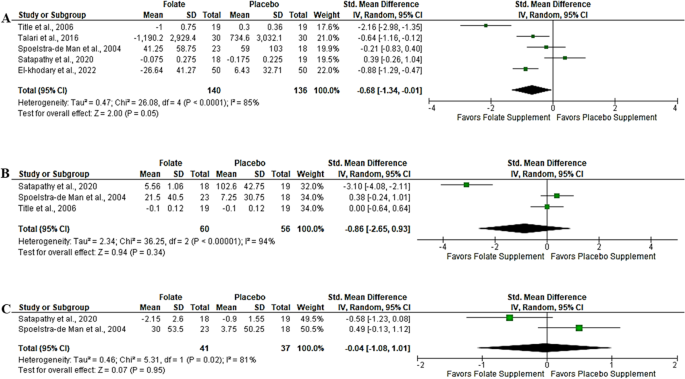
Effect of folic acid supplementation on homocysteine
The effect of folic acid supplementation on homocysteine was analyzed from nine trials [23, 24, 27, 37,38,39,40,41,42] with a sample size of 426 T2DM on folic acid versus placebo. The overall effect from the random effect model showed a large effect size demonstrated by a significant reduction in the level of homocysteine in T2DM on folic acid compared to placebo, SMD = −1.53, 95%CI (−2.14,−0.93), p < 0.05 (Fig. 2). Of concern was an observed level of heterogeneity (I2 = 86%) across the included studies.
Effect of folic acid supplementation on inflammation
Three markers of inflammation were evaluated: CRP, TNF-α, and IL-6; however, only five trials [21, 25, 35,36,37] evaluated CRP in T2DM following folic acid supplementation compared to placebo. The results from the random-effect meta-analysis revealed a medium effect size demonstrated by a marginal reduction in CRP; SMD = −0.68, 95%CI (−1.34, −0.01), p = 0.05 (Fig. 3A). This was accompanied by a high level of heterogeneity (I2 = 85%). Likewise, the results from 3 trials [23, 27, 38] that evaluated TNF-α showed a large effect size; however, this was statistically not significant, SMD = −0.86, 95%CI (−2.65, 0.93), p = 0.34 (Fig. 3B). These trials revealed moderate evidence of heterogeneity (I2 = 94%). Only two trials [23, 38] assessed the effect of folate on IL-6; the evidence from the random-effect meta-analysis showed a small effect size, and this also not significant, SMD = −0.04, 95%CI (−1.08, 1.01), p = 0.95 (Fig. 3C). Similarly, there was moderate evidence of heterogeneity across these trials (I2 = 81%).
Heterogeneity and subgroup analysis
Due to observed heterogeneity in homocysteine results, we performed subgroup analyses based on both sample size (< or > 50 T2DM patients) and folate dosage (0.25, 5, or 10 mg). The subgroup analysis of the sample size revealed evidence of heterogeneity (I2 = 70.5%) (Fig. 1SA). Notably, studies with a sample size below 50 exhibited high heterogeneity (I2 = 89%), contrasting with those above 50, which displayed no heterogeneity (I2 = 0%) (Fig. 1SA).
Additionally, the subgroup analysis on the dosage of folic acid supplementation showed a decrease in heterogeneity (I2 = 20.1%); however, a 5 mg administration led to a 2% decrease in heterogeneity (I2 = 86%) (Fig. 1SB). Subgroup analysis on duration of intervention revealed reduced heterogeneity (I2 = 35.8%). Interestingly, medium duration demonstrated no evidence of heterogeneity (I2 = 0%) (Fig. 2SA). Finally, a subgroup analysis based on gender distribution for homocysteine revealed an overall test difference indicating heterogeneity (I2 = 95.7%). However, studies conducted in males showed no heterogeneity(I2 = 0%), whereas those involving both genders resulted in high heterogeneity (I2 = 89%) (Fig. 2SB). The results of a meta-analysis on CRP revealed a moderate heterogeneity(I2 = 73%). This warranted subgroup to find the source of this variation; firstly, we subgrouped studies according to sample size and dosage of folic acid supplementation. We found that the evidence from trials with a sample size below 50 slightly changed heterogeneity (I2 = 50%), while more than 50 had I2 = 0% (Fig. 3SA). Interestingly, the overall test for subgroup differences also revealed no heterogeneity (I2 = 0). On the other hand, subgroups according to dosage showed that trials that used 5 mg of folate/folic acid had I2 = 74%, while those that used 10 mg had I2 = 85%. Moreover, the test for subgroup difference showed I2 = 92.3% (Fig. 3SB).
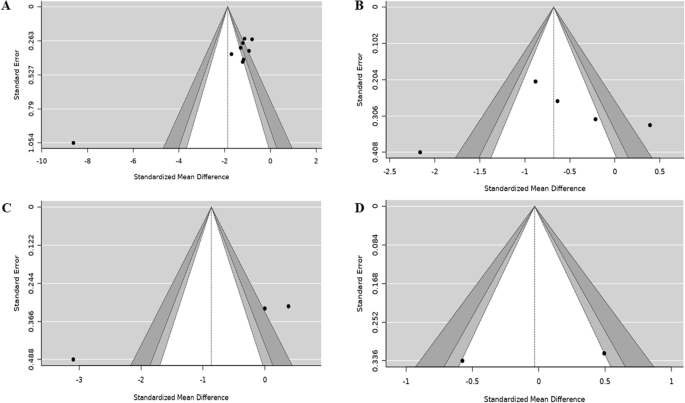
Publication bias (Funnel plots and Egger’s regression test)
Publication bias was assessed by visualization of the funnel plot, and we noted evidence of bias on homocysteine (Fig. 4A), and this was consistent with the findings of the Eggers regression test (Z score = −6.06, p < 0.05). This suggests that trials with positive significant results were more likely to be published than negative trials. On the contrary, the funnel plot revealed no evidence of bias on hs-CRP- (Fig. 4B), which was supported by the Eggers regression test (Z score = −0.75, p = 0.46). For TNF-α, Eggers regression showed some potential level of bias (Z score = −6.15, p < 0.05); this was supported by a funnel plot (Fig. 4C). Additionally, IL-6 revealed no bias graphically (Fig. 4D); however, due to few trials, no regression was assessed.
Sensitivity analysis across the trials
Sensitivity results for homocysteine showed that the exclusion of the study by Satapathy et al. [38], due to small weight, resulted in the change in overall effect size, SMD = −1.14, 95%CI (−1.36, −0.92), p = 0.0000 (Table 2S). The exclusion of El-khodary et al. [37] in CRP results changed the overall effect size to SMD = −0.63, 95%CI (−1.56, 0.30), p = 0.16 (Table 3S). When Satapathy et al., [38] was excluded from TNF-α analysis, the effect size changed to SMD = 0.20, 95%CI (−0.27, 0.66), p = 0.0000 (Table 4S). For IL-6, exclusion of [38] led to SMD = 0.49, 95%CI (−0.13, 1.12), p = 0.0000 (Table 5S).
Assessment of risk of bias across and certainty of evidence across the included trials
Among nine trials, two trials [39, 41] were judged as having some concerns of bias as the process of randomization was not clear in their methodology. Only one trial was judged as high risk [42], due to lack of information about the randomization method used. Interestingly, 67% of trials [23, 24, 27, 37, 38, 40] were judged as low risk of bias as they scored low risk across all domains (Fig. 5). GRADING of trials revealed moderate certainty of evidence on homocysteine, CRP, and TNF-α, while IL-6 evidence was found to be of low certainty (Table 6S). The downgrade was due to heterogeneity, risk of bias, or imprecision due to the small sample size (<400).
Discussion
To the best of our knowledge, this is the first comprehensive meta-analysis of RCT to evaluate the effect of folic acid supplementation on homocysteine and inflammation in adult patients with T2DM. We found that folic acid supplementation was associated with a reduction in homocysteine levels. The observed SMD (1.52) was large effect, suggesting anti-homocysteine properties. Additionally, there was a marginal effect of folic acid on CRP without a significant effect on TNF-α and IL-6 in patients with T2DM. Subgroup analysis showed that the folate effect on homocysteine was more pronounced at a higher dose (10 mg) than 5 mg supplementation. However, it is important to note that only one trial used 10 mg compared to 5 mg that used 5 mg of folic acid. It was evident that studies with a sufficient sample size (50 and above patients) had a more pronounced effect than those with a smaller sample size. Although folic acid supplementation at both short and medium periods reduced homocysteine, the reduction was more pronounced at short periods (0–4 weeks) compared to medium periods (8–12 weeks). Our research reveals lower homocysteine levels in individuals living with T2DM receiving folate supplements, indicating a potential decrease in the risk of CVD. We are confident with the evidence synthesized in this study as the evidence showed moderate certainty in homocysteine. In T2DM, insulin resistance and associated impaired kidney function results in an elevated homocysteine level [43,44,45,46,47]. This elevation promotes the development of CVD complications associated with T2DM.
Interestingly, the evidence from this study shows that folic acid supplementation can reduce homocysteine by converting it into methionine, lowering the risk of cardiovascular complications in T2DM patients [26]. Notably, previous evidence has shown that folic acid supplementation can reduce homocysteine levels in patients living with T2DM by increasing the 5-methyltetrahydrofolate intracellular pool [37]. This effect is crucial as an elevated level of homocysteine can damage blood vessels and contribute to the development of CVD [45]. Therefore, any strategies therapeutically that reduce homocysteine may assist in alleviating CVD among T2DM. In obese children, similar trends have been observed when administering a minimum of 1 g of folic acid, leading to a substantial reduction in homocysteine levels [48]. Similar findings are observed in gestational diabetes, as 1 mg and 5 mg of folic acid supplementation significantly reduced homocysteine levels [49]. Although the pathological and physiological mechanisms of these conditions differ, these findings demonstrate the efficacy of folate supplementation across diverse conditions and age groups. A non-randomized trial in menopausal T2DM women also showed that 800 µg of folate significantly reduced homocysteine levels. However, this study revealed an inverse correlation between folic acid and homocysteine (r = −0.4876, p-value = 0.0134) [50]. Although the mechanism by which folate reduces homocysteine in T2DM is poorly documented, it is assumed that this is associated with the role of folate in one-carbon metabolism. Folic acid supplementation increases the availability of one-carbon units, which then promotes the remethylation of homocysteine to methionine [51]. This subsequently results in a decrease in homocysteine levels in the body. While such benefits are acknowledged, contrasting findings from other studies suggest a possible risk of CVD in T2DM, even with folic acid supplementation [52]. These findings suggest a limitation in the beneficial effect of folate, especially in T2DM. It is assumed that folate deficiency impairs the conversion of homocysteine to methionine, resulting in homocysteine accumulation in the blood [53]. High homocysteine levels are associated with an increased risk of CVDs and other health problems.
Although there was a marginal effect on hs-CRP (p = 0.05), no significant effect of folic acid supplementation on other markers of inflammation was observed. This was shown by no significant effect on TNF-α and IL-6 following supplementation with folic acid compared to placebo. A reduction in hs-CRP following folic acid supplementation reveals, to some extent, the beneficial effect of folic acid as an anti-inflammatory agent. However, as not all inflammatory markers were reduced, the findings are thus inconclusive. Among some factors contributing to the challenge in elucidating conflicting findings regarding the impact of folic acid on inflammation is the limited number of trials conducted. The inability of folic acid to improve some markers of inflammation indicates that it does not exhibit anti-inflammatory properties. For instance, Spoelstra-de Man et al., [23] reported no effect of folic acid on hs-CRP, IL-6, and TNF-α. The same findings were observed by Title et al. [27], however, only TNF-α and hs-CRP were investigated, and no effect was observed. Despite these null findings, another trial observed a significant effect of folic acid on hs-CRP in T2DM, as demonstrated by a significant decrease in hs-CRP within the folic acid group before and after folic acid supplementation. This same trend was also observed when folic acid supplementation was compared to placebo [24]. The latter supports our findings as we observed a reduction in hs-CRP with a medium to large effect size (Cohen d = 0.68). Other researchers reported a significant decrease in IL-6 and TNF-α following folic acid supplementation compared to placebo, suggesting the anti-inflammatory effects of folic acid in T2DM [38]. These findings differ from our overall findings in this study as we reported no significant effect of folic acid on TNF-α and IL-6. Another study showed a significant change between baseline and post-treatment on hs-CRP, however, there were no significant changes between the folic acid and placebo groups [38]. In obese children, 1 mg of folic acid has proven to offer an anti-inflammatory effect, as demonstrated by a significant decrease in IL-6, TNF-α, and IL-8 [48].
Similarly, El-khodary et al. [37] also showed a significant decrease in hs-CRP between baseline and post-treatment (p = 0.008). The same trial reported a significant decrease in hs-CRP following three months of folic acid supplementation compared to placebo (p = 0.005). This study also showed a positive correlation between homocysteine and hs-CRP (r = 0.308, p = 0.002). Due to these contradicting results on inflammation, the effect of folic acid on inflammation is not clear, other researchers have suggested that folic acid may be involved in the reduction of hs-CRP by reducing homocysteine and oxidative stress. For instance, Talari et al., [24] reported an increased adjusted glutathione (GSH) following folic acid supplementation in T2DM compared to placebo.
Additionally, folic acid exhibits anti-insulinemic activities [54, 55] may further alleviate inflammation by suppressing the synthesis of inflammatory cytokines. It is important to note that while the benefits were not observed in this study, this might be attributable to the number of trials analyzed primarily because observational differences were noted. Previous evidence suggests that homocysteine promotes the expression of inflammatory markers by increasing the activation of nuclear factor kappa β (NF-kβ) and poly-adenosine diphosphate (ADP) ribose polymerase. Therefore, we speculate that folic acid anti-homocysteine properties may alleviate inflammation by inhibiting the activation of NF-κβ and ADP and thus suppressing the expression of inflammatory markers [56, 57]. Evidence from in vitro studies has also shown that folic acid may reduce inflammation by inhibiting the phosphoinositide 3-kinases (PI3K)/hypoxia-inducible factor 1-alpha (HIF-1α) pathway [58]. Even though the reduction in homocysteine following folate supplementation is normally accompanied by a reduction in CRP and subsequent deactivation of NF-κβ and low IL-6 and TNF-α, the contradictory findings observed in our study may be due to few trials and sample size across the trials analyzed in this study.
Strength and limitation
The present analyses exclusively examined evidence from randomized trials, considered to provide high clinical evidence. Notably, there was a low risk of bias observed across various domains in the risk of bias assessment, indicating that the quality of the studies was satisfactory. The GRADE tool was also employed to evaluate the overall quality of the analyzed evidence, and it was categorized as either moderate or very low in one outcome due to the small sample size.
Furthermore, a comprehensive subgroup analysis was performed, considering various confounding factors. The I2 statistics revealed moderate heterogeneity. For transparency, the study was registered with PROSPERO, and the experienced researchers adhered to PRISMA guidelines, boosting confidence in the reliability of the current findings. However, it is crucial to acknowledge certain limitations in our study, such as few relevant trials, indicating a minimal sample size of only 426 patients living with T2DM. Moreover, existing trials have employed varying quantitative methodologies, introducing potential differences in sensitivity and specificity, especially with the use of ELIZA AND HPLC for the determination of homocysteine.
Conclusion and future recommendations
The findings from nine trials involving a sample of 426 participants in this study indicate that folic acid supplementation in T2DM may reduce homocysteine levels, a potential biomarker for CVDs. However, due to the limited number of trials analyzed, null effects were observed concerning some of the inflammatory markers. It is crucial to interpret the conclusions of our study with caution, emphasizing the need for further trials with adequate sample sizes.
Considering the limitations acknowledged in this study, we propose recommendations for future investigations into folic acid in T2DM, particularly focusing on inflammation. We suggest that forthcoming RCTs use sufficient sample sizes and adhere to the reporting guidelines outlined in the consolidated standards of reporting trials (CONSORT). Additionally, these trials should adhere to standardized methodologies, implementing an accurate randomization process, blinding of personnel and participants. Furthermore, we emphasize the necessity for high-quality meta-analyses to comprehensively elucidate the benefits of folic acid supplementation in managing T2DM.
Data availability
The data used in this review are available from the corresponding author upon reasonable request.
References
American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care. 2022;45:S17–S38.
Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26:25–32.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pr. 2022;183:109119.
Giorgino F, Leonardini A, Laviola L. Cardiovascular disease and glycemic control in type 2 diabetes: Now that the dust is settling from large clinical trials. Ann N. Y Acad Sci. 2013;1281:36–50.
Hayfron-Benjamin CF, Maitland-Van Der Zee AH, van den Born BJ, Amoah AGB, Meeks KAC, Klipstein-Grobusch K, et al. Association between C reactive protein and microvascular and macrovascular dysfunction in sub-Saharan Africans with and without diabetes: The RODAM study. BMJ Open Diabetes Res Care 2020;8. https://doi.org/10.1136/bmjdrc-2020-001235.
Pfützner A, Schöndorf T, Hanefeld M, Forst T. High-sensitivity C-reactive protein predicts cardiovascular risk in diabetic and nondiabetic patients: effects of insulin-sensitizing treatment with pioglitazon. J Diabetes Sci Technol. 2010;4:706–16.
Abdulhameed LQ, Sultan AA, AL-Mahdawi ZMM. Homocysteine: A recent potential risk factor for type 2 diabetes mellitus patients in Diyala Province. AIP Conf Proc. 2023;2593:050004.
Wu JT. Circulating homocysteine is an inflammation marker and a risk factor of life-threatening inflammatory diseases. J Biomed Lab Sci. 2007;19:107–12.
Lala K, Lala D, Duggad S. Serum vitamin B12 and homocysteine levels in type 2 diabetes patients on metformin. Int J Adv Med. 2020;7:1376.
Durga J, Van Tits LJH, Schouten EG, Kok FJ, Verhoef P. Effect of lowering of homocysteine levels on inflammatory markers a randomized controlled trial. Arch Intern Med. 2005;165:1388–94.
Li T, Chen Y, Li J, Yang X, Zhang H, Qin X, et al. Serum homocysteine concentration is significantly associated with inflammatory/immune factors. PLoS One. 2015;10:e0138099.
El Oudi M, Aouni Z, Mazigh C, Khochkar Phd R, Gazoueni Phd E, Haouela H, et al. Homocysteine and markers of inflammation in acute coronary syndrome. Exp Clin Cardiol. 2010;15:e25–e28.
Elsherbiny NM, Sharma I, Kira D, Alhusban S, Samra YA, Jadeja R, et al. Homocysteine induces inflammation in retina and brain. Biomolecules. 2020;10:393.
Zhang Z, Gu X, Fang X, Tang Z, Guan S, Liu H, et al. Homocysteine and the risk of cardiovascular events and all-cause death in elderly population: a community-based prospective cohort study. Ther Clin Risk Manag. 2020;16:471–81.
Sato S, Tajiri Y, Nakayama H, Yamada K. Folic acid supplementation of aspirin therapy further improves vascular endothelial function among patients with type 2 diabetes: a short-term crossover study. Diabetol Int. 2015;6:284–9.
Miyan Z, Waris N. Association of vitamin B 12 deficiency in people with type 2 diabetes on metformin and without metformin: a multicenter study, Karachi, Pakistan. BMJ Open Diabetes Res Care. 2020;8:e001151.
Awad NA, Alsaady ZA, Albayati MAM, Mutlak SS. Correlation study of metformin drug with vit.B12 and folic acid in women suffer of type 2 diabetic disease. J Pharm Negat Results. 2022;13:308–12.
Song S, Song BM, Park HY. Associations of serum folate and homocysteine concentrations with all-cause, cardiovascular disease, and cancer mortality in men and women in Korea: the Cardiovascular Disease Association Study. J Nutr. 2023;153:760–70.
Ebesunun MO, Obajobi EO. Elevated plasma homocysteine in type 2 diabetes mellitus: a risk factor for cardiovascular diseases. JAMA Netw Open. 2022;5:e2146124.
MacGirlley R, Phoswa WN, Mokgalaboni K. Modulatory Properties of Vitamin D in Type 2 Diabetic Patients: A Focus on Inflammation and Dyslipidemia. Nutrients 2023;15. https://doi.org/10.3390/nu15214575.
Qudsia F, Matti HA, Riaz S. Pleiotropic effect of folate-cobalamin combinational therapy on diabetes mellitus. Ann Nutritional Disord Ther. 2020;7:1–8.
Fact Sheet for Health Professionals. Folate - Health Professional Fact Sheet https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/ (accessed 28 Oct 2023).
Spoelstra-de MA, Brouwer CB, Terheggen F, Bollen JM, Stehouwer CD, Smulders YM. No effect of folic acid on markers of endothelial dysfunction or inflammation in patientswith type 2diabetes mellitus and mild hyperhomocysteinaemia. J Med. 2004;62:246–53.
Talari HR, Rafiee M, Farrokhian A, Raygan F, Bahmani F, Darooghegi Mofrad M, et al. The effects of folate supplementation on carotid intima-media thickness and metabolic status in patients with metabolic syndrome. Ann Nutr Metab. 2016;69:41–50.
Fatahi S, Pezeshki M, Mousavi SM, Teymouri A, Rahmani J, Kord Varkaneh H, et al. Effects of folic acid supplementation on C-reactive protein: A systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovascular Dis. 2019;29:432–9.
Kaye AD, Jeha GM, Pham AD, Fuller MC, Lerner ZI, Sibley GT, et al. Folic Acid Supplementation in Patients with Elevated Homocysteine Levels. Adv Ther. 2020;37:4149–64.
Title LM, Ur E, Giddens K, McQueen MJ, Nassar BA. Folic acid improves endothelial dysfunction in type 2 diabetes - An effect independent of homocysteine-lowering. Vasc Med. 2006;11:101–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:1–9.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61.
Giuliano C, Karahalios A, Neil C, Allen J, Levinger I. The effects of resistance training on muscle strength, quality of life and aerobic capacity in patients with chronic heart failure — A meta-analysis. Int J Cardiol. 2017;227:413–23.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:1–10.
Bowden J, Tierney JF, Copas AJ, Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med. Res. Methodol. 2011;11. https://doi.org/10.1186/1471-2288-11-41.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I 2 Index? Psychol Methods. 2006;11:193–206.
Moreno SG, Sutton AJ, Ades A, Stanley TD, Abrams KR, Peters JL, et al. Assessment of regression-based methods to adjust for publication bias through a comprehensive simulation study. BMC Med. Res. Methodol. 2009;9. https://doi.org/10.1186/1471-2288-9-2.
Doleman B, Freeman SC, Lund JN, Williams JP, Sutton AJ. Funnel plots may show asymmetry in the absence of publication bias with continuous outcomes dependent on baseline risk: presentation of a new publication bias test. Res Synth Methods. 2020;11:522–34.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction - GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
El-khodary NM, Dabees H, Werida RH. Folic acid effect on homocysteine, sortilin levels and glycemic control in type 2 diabetes mellitus patients. Nutr Diabetes. 2022;12:1–8.
Satapathy S, Bandyopadhyay D, Patro BK, Khan S, Naik S. Folic acid and vitamin B12 supplementation in subjects with type 2 diabetes mellitus: A multi-arm randomized controlled clinical trial. Complement Ther Med. 2020;53:102526.
Gargari BP, Aghamohammadi V, Aliasgharzadeh A. Effect of folic acid supplementation on biochemical indices in overweight and obese men with type 2 diabetes. Diabetes Res Clin Pr. 2011;94:33–38.
Mangoni AA, Sherwood RA, Asonganyi B, Swift CG, Thomas S, Jackson SHD. Short-term oral folic acid supplementation enhances endothelial function in patients with type 2 diabetes. Am J Hypertens. 2005;18:220–6.
Aghamohammadi V, Gargari P, Aliasgharzadeh A. Effect of folic acid supplementation on homocysteine, serum total antioxidant capacity, and malondialdehyde in patients with type 2 diabetes mellitus. J Am Coll Nutr. 2011;30:210–5.
Aarsand AK, Carlsen SM. Folate administration reduces circulating homocysteine levels in NIDDM patients on long-term metformin treatment. J Intern Med. 1998;244:169–74.
Zhang X, Qu YY, Liu L, Qiao YN, Geng HR, Lin Y, et al. Homocysteine inhibits pro-insulin receptor cleavage and causes insulin resistance via protein cysteine-homocysteinylation. Cell Rep. 2021;37. https://doi.org/10.1016/j.celrep.2021.109821.
Shen Z, Zhang Z, Zhao W Relationship between plasma homocysteine and chronic kidney disease in US patients with type 2 diabetes mellitus: a cross-sectional study. BMC Nephrol. 2022;23. https://doi.org/10.1186/s12882-022-03045-6.
Lei X, Zeng G, Zhang Y, Li Q, Zhang J, Bai Z, et al. Association between homocysteine level and the risk of diabetic retinopathy: a systematic review and meta-analysis. Diabetol. Metab. Syndr. 2018;10. https://doi.org/10.1186/s13098-018-0362-1.
Zhao W, Chen L, Lin Y, He H, Ma H, Hu Q, et al. Association of homocysteine and insulin resistance with increased risk of mortality in a nondiabetic population: third national health and nutrition examination survey. Metab Syndr Relat Disord. 2022;20:255–63.
Meigs JB, Jacques PF, Selhub J, Singer DE, Nathan DM, Rifai N, et al. Fasting plasma homocysteine levels in the insulin resistance syndrome the Framingham Offspring Study. Diabetes Care. 2001;24:1403–10.
Dehkordi E, Sedehi M, Shahraki Z, Najafi R. Effect of folic acid on homocysteine and insulin resistance of overweight and obese children and adolescents. Adv Biomed Res. 2016;5:88.
Davari Tanha F, Kaveh M, Shariat M. Homocysteine in gestational diabetes and normal pregnancy plus effects of folic acid. Iran J Public Health. 2008;37:118–26.
Vijayakumar A, Kim EK, Kim H, Choi YJ, Huh KB, Chang N. Effects of folic acid supplementation on serum homocysteine levels, lipid profiles, and vascular parameters in post-menopausal Korean women with type 2 diabetes mellitus. Nutr Res Pr. 2017;11:327–33.
Williamson JM, Arthurs AL, Smith MD, Roberts CT, Jankovic-Karasoulos T. High folate, perturbed one-carbon metabolism and gestational diabetes mellitus. Nutrients 2022;14. https://doi.org/10.3390/nu14193930.
Song Y, Cook NR, Albert CM, Van Denburgh M, Manson JAE. Effect of homocysteine-lowering treatment with folic acid and B vitamins on risk of type 2 diabetes in women: A randomized, controlled trial. Diabetes. 2009;58:1921–8.
Varela-Moreiras A, Martínez-Vega G, Partearroyo R, Pajares T, Varela-Nieto MA. Folic acid deficiency impairs homocysteine metabolism in the inner ear inducing premature hearing loss in C57BL/6J mice. 2013. http://hdl.handle.net/10261/125351.
Lind MV, Lauritzen L, Kristensen M, Ross AB, Eriksen JN. Effect of folate supplementation on insulin sensitivity and type 2 diabetes: A meta-analysis of randomized controlled trials. Am J Clin Nutr. 2019;109:29–42.
Asbaghi O, Ashtary-Larky D, Bagheri R, Moosavian SP, Olyaei HP, Nazarian B et al. Folic acid supplementation improves glycemic control for diabetes prevention and management: A systematic review and dose-response meta-analysis of randomized controlled trials. Nutrients 2021;13. https://doi.org/10.3390/nu13072355.
Zhang X, Chen S, Li L, Wang Q, Le W. Folic acid protects motor neurons against the increased homocysteine, inflammation and apoptosis in SOD1G93A transgenic mice. Neuropharmacology. 2008;54:1112–9.
Zhang L, Li Z, Xing C, Gao N, Xu R. Folate Reverses NF-κB p65/Rela/IL-6 level induced by hyperhomocysteinemia in spontaneously hypertensive rats. Front Pharmacol. 2021;12. https://doi.org/10.3389/fphar.2021.651582.
Huang X, He Z, Jiang X, Hou M, Tang Z, Zhen X et al. Folic acid represses hypoxia-induced inflammation in THP-1 cells through inhibition of the PI3K/Akt/HIF-1α pathway. PLoS ONE 2016;11. https://doi.org/10.1371/journal.pone.0151553.
Acknowledgements
We acknowledge University of South Africa research office for payment of article processing charges.
Funding
This study is partially funded by the South African Research Excellence Award for Next Generation Researchers (NONF230515106418), Research Development Grants for nGAP Scholars (NGAP23022780506) and South African National Research Foundation Special Transformative Awards (NSTA231114163486). Funders have no role in the conceptualization, preparation, data analysis, and conclusion reached in this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization, KM.; methodology, KM, GRM, and WNP.; software, KM.; validation, KM, WNP, and SLL.; formal analysis, K.M.; investigation, K.M.; resources, KM.; data curation, KM and WNP; funding, KM; writing—original draft preparation, KM; writing—review and editing, KM, GRM, WNP and SLL; supervision, WNP and SLL. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mokgalaboni, K., Mashaba, G.R., Phoswa, W.N. et al. Folic acid supplementation on inflammation and homocysteine in type 2 diabetes mellitus: systematic review and meta-analysis of randomized controlled trials. Nutr. Diabetes 14, 22 (2024). https://doi.org/10.1038/s41387-024-00282-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41387-024-00282-6