Abstract
Background
To identify modifiable antecedents during pre-pregnancy and pregnancy windows associated with a positive child health at 10 years of age.
Methods
Data on 889 children enrolled in the Extremely Low Gestational Age Newborn (ELGAN) study in 2002–2004 were analyzed for associations between potentially modifiable maternal antecedents during pre-pregnancy and pregnancy time windows and a previously described positive child health index (PCHI) score at 10 years of age. Stratification by race was also investigated for associations with investigated antecedents.
Results
Factors associated with higher PCHI (more positive health) included greater gestational age, birth weight, multiple gestation, and medical interventions, including assisted reproduction and cervical cerclage. Factors associated with lower PCHI included correlates of lower socioeconomic status, pre-pregnancy chronic medical disorders in the mother such as pre-pregnancy body mass index (BMI), and maternal asthma. When stratified by race, variation in significant results was observed.
Conclusions
Among children born extremely preterm, medical interventions and higher socioeconomic status were associated with improved PCHI, while chronic illness and high BMI in the mother is associated with lower PCHI at 10 years of age. Knowledge of such antecedent factors could inform efforts to develop interventions that promote positive child health outcomes in future pregnancies.
Similar content being viewed by others
Introduction
Positive child health reflects the reduced presence of aberrant conditions or disease, along with positive physical, cognition, and social–emotional well-being, and serves as a foundation for adult health and wellness. Whereas traditional analyses in children’s health studies generally have focused on risk for adverse outcomes, another approach is to increase understanding of what factors contribute to positive health. Preterm infants are at increased risk of a variety of adverse developmental and health outcomes.1,2 For example, at 10 years of age, in the Extremely Low Gestational Age Newborn (ELGAN) study cohort of children born at <28 weeks gestation in the United States, 25% had moderate-to-severe cognitive impairment,3 7.1% had autism spectrum disorder,4 7.6% had epilepsy,5 11.4% had cerebral palsy,6 and 4.9% had severe motor impairment.7 We recently described a positive child health index (PCHI) based on 11 adverse outcomes and found that within the ELGAN cohort, higher values on this index were associated with higher quality of life scores.8 Notably, 32% of the cohort had none of the 11 adverse outcomes (PCHI of 100%) at age 10 years.
Based on the premise that promoting antecedents of positive health outcomes will lead to improved long-term outcomes, the aim of this study was to identify early-life antecedents associated with positive child health outcomes at 10 years of age in the ELGAN cohort. Maternal antecedents were examined from the pre-pregnancy and pregnancy time intervals with a focus on potentially modifiable antecedents, such as maternal socioeconomic and health status. Knowledge of such antecedent factors could inform the development of educational practices and other interventions educational efforts and interventions that would increase the likelihood of positive child health outcomes in future pregnancies.
Methods
ELGAN study participants
STROBE cohort reporting guidelines were utilized for this study.9 From 2002 to 2004, women giving birth prior to 28 weeks gestation at one of 14 academic medical centers in five states in the United States were asked to enroll in the ELGAN study. Maternal consent was provided either upon hospital admission or prior to or shortly after delivery. The Institutional Review Board at each participating institution approved study procedures. Of the mothers approached, approximately 85% gave consent for participation in the original ELGAN study, resulting in a cohort of 1249 mothers and 1506 infants.
A trained research nurse interviewed mothers using a structured questionnaire shorty after time of delivery to obtain a variety of factors including sociodemographic information, such as maternal age, years of education, eligibility for public insurance, and mother’s pre-pregnancy weight and height. Information on pre-pregnancy and pregnancy maternal medications and health conditions was also collected at this time. Medical records were reviewed to collect medical information about the infant and mother. All antecedents investigated in this study were obtained from the maternal interview after birth and from maternal medical records. A total of 58 antecedents of interest were identified for this study, but 13 of the 58 were excluded from analyses due to a prevalence of 5% or lower in the population of participants resulting in a set of 45 for analysis. The complete set of 45 investigated antecedents and 13 excluded antecedents are listed in the Supplementary Information (Supplementary Table S4 and SI page 6, respectively).
Within a few days before or after delivery, mothers were interviewed and asked about pre-pregnancy weight and height, from which pre-pregnancy body mass index (BMI; weight/height2) was calculated. BMI was classified as underweight (≤18.4 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Gestational ages were estimated based on the dates of embryo retrieval, intrauterine insemination, or fetal ultrasound before the 14th week. An infant’s birth weight Z-score is defined as the number of standard deviations (SDs) above or below the median weight of infants of the same gestational age in referent samples not delivered for preeclampsia or fetal indications.10,11
ELGAN 10-year follow-up
In the original ELGAN cohort, 1198 children (80% of those enrolled) survived to age 10 years. A subset of 966 eligible children were selected for follow-up at 10 years of age because neonatal blood spots had been collected from these children, as the primary goal of the ELGAN study was to evaluate associations between neonatal systemic inflammation and cognitive outcome at 10 years of age. Of the 966 children recruited, a total of 889 (92%) participated in some or all of the 10-year evaluations (Supplementary Fig. S1), which were administered in one visit of 3 to 4 hours.
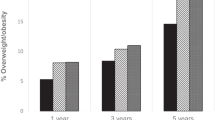
Eleven adverse outcomes were assessed at the 10-year follow-up: moderate/severe cognitive impairment,7 bilateral blindness,12 hearing impairment,12 gross motor function impairment,7 epilepsy,5 attention-deficit/hyperactivity disorder,13 autism,4 anxiety, depression, asthma, and obesity (i.e., BMI above the 95 percentile). Based on these 11 adverse outcomes, a PCHI was generated for each child.8 Supplementary Table S1 compares the maternal and newborn characteristics of the 889 children who were assessed and the 77 children who were not assessed from among the 966 children eligible for study participation. The rates of missing data among the 889 ELGAN who were assessed are provided in Supplementary Table S2. Although there were some missing data for individual disorders, children were assigned a PCHI that reflected their available data. Children with no reported disorders were assigned the highest PCHI of 100%. Any additional disorder reported for a child decreased the PCHI by a percentage based on the number of disorders investigated (9% drop for each additional disorder). In the binary model, children with no disorders (100% PCHI) were compared to children with any disorders (PCHI below 100%). In the categorical model, children with no disorders (100% PCHI) were compared to children with one disorder (PCHI 91%), two disorders (PCHI 82%), and three and above disorders (PCHI ≤73%). Further details of study methods can be found in Supplementary Information Methods (SI pages 3–6).
Statistical analysis
The associations between maternal demographics/modifiable antecedents and PCHI were analyzed using logistic regression for the dichotomous classification of disorders (0 vs. 1+) and ordinal logistic regression for the categorical classification of disorders (0 vs. 1 vs. 2 vs. 3+). Each of these regression models adjusted for the potential confounders of child’s sex, gestational age, and birth weight Z-score, public insurance, and maternal education, and a dichotomous classification of race (white vs. black/other). For the ordinal logistic regression models, the proportional odds assumption was verified to be tenable by inspecting plots of the empirical logits. To investigate whether the strength of associations between antecedents and PHCI varied by race, we performed formal tests of an interaction of antecedent and race. For cases where the interaction p value was or approached significance (p < 0.10), we conducted analyses stratified by race, presented in Tables 2 and 3. Since a large number of modifiable antecedents were considered, multiple testing was also addressed by performing Bonferroni adjustments to computed p values. Results that remained significant after additional Bonferroni adjustment are indicated with an asterisk in Tables 2 and 3.
Sensitivity analysis: mixed models
Generalized linear mixed models (GLMMs) were fit to account for possible dependence among children from a multiple birth. Estimates were made using Gaussian quadrature within PROC GLIMMIX with a random intercept associated with instances of a multiple birth. For each dichotomous coding of PCHI, the logistic regression model was compared with a logistic regression mixed model, and for each categorical coding of PCHI, the ordinal logistic model was compared with an ordinal logistic mixed model.
Results
Maternal demographics and PCHI
Maternal characteristics of the 889 ELGAN children that were assessed for PCHI at 10 years of age using the multi-categorical logistic model are presented in Table 1 (Supplementary Table S3). Lower PCHI scores (i.e., less positive health) were found among children born to mothers who identified as black/other race and were eligible for public health insurance (i.e., Medicaid). (Results for categorical analyses can be found in Supplementary Table S3.)
Newborn demographics and PCHI
Higher gestational ages and higher birth weights were associated with higher positive child health at 10 years of age (Table 1). (Supplementary Table S3 provides results for the adjusted categorical analyses).
Antecedents associated with higher PCHI (more positive child health)
Of the 45 modifiable antecedents investigated during the pre-pregnancy and pregnancy time intervals, six were associated with more positive child health, in at least one model; among study participants of all races: cervical cerclage, during pregnancy urine, bladder, or kidney infection, and multiple gestation (Tables 2 and 3, Supplementary Table S4–S7). Assisted reproduction and proteinuria during pregnancy were associated with more positive child health among non-white study participants, while receipt of antibiotics was associated with more positive child health among white participants.
Antecedents associated with lower PCHI (less positive child health)
Eight factors were associated with less positive health in at least one model; among study participants of all races: maternal overweight or obese pre-pregnancy, maternal asthma pre-pregnancy, maternal asthma during pregnancy, maternal treatment with asthma medication during pregnancy, maternal consumption of aspirin during pregnancy, and transition from private to public health insurance between the child’s visits at 2 years of age and 10 years of age (Tables 2 and 3, Supplementary Tables S4–S7). Public health insurance during pregnancy, proteinuria during pregnancy, and second-hand smoke exposure during pregnancy were associated with less positive child health among white study participants.
When conservative Bonferroni adjustments were made to account for multiple association analyses, the only antecedent with a statistically significant association with PCHI modeled as a binary outcome was maternal pre-pregnancy BMI (Table 2). In the multi-category ordinal logistic model, associations with PCHI were found for the antecedents maternal pre-pregnancy BMI, maternal use of asthma medicine during pregnancy, and multiple gestation (Table 3).
There was complete concordance among all maternal characteristics, newborn characteristics, and modifiable antecedents, with a statistically significant association with PCHI at the 0.05 level between the mixed models and the usual generalized linear models (Tables 1–3, Supplementary Tables S3–S7).
Discussion
The aim of this study was to identify early-life, potentially modifiable antecedents that are associated with positive child health at 10 years of age among children born extremely preterm (Table 4). We identified six antecedents associated with higher PCHI (more positive health); for three of these factors (cervical cerclage, multiple gestation, and maternal during pregnancy urine, bladder, or kidney infection), the association was found among study participants of all races. Among non-white study participants, assisted reproduction and proteinuria were associated with higher PCHI, and among white participants, receipt of antibiotics was associated with higher PCHI. We identified eight antecedents associated with lower PCHI (less positive health); six reflect maternal health: pre-pregnancy overweight/obese, pre-pregnancy and pregnancy asthma, treatment with asthma medication during pregnancy, maternal consumption of aspirin during pregnancy, and second-hand tobacco smoke. Among white study participants, mother’s exposure to tobacco smoke during pregnancy, proteinuria during pregnancy, and public insurance during pregnancy were associated with lower PCHI. Among study participants of all races, transition from private to public insurance between the child’s study visits at 2 and 10 years of age was associated with lower PCHI.
Increased PCHI
The finding that multiple gestation and cerclage are associated with higher PCHI could be attributable to residual confounding by socioeconomic status. The variables that we used to adjust for socioeconomic status, maternal education and insurance status, likely do not fully capture variation in socioeconomic status, which in the ELGAN study is associated with adverse neurodevelopmental outcomes,14,15 as well as asthma16 and obesity in the child.17 The more positive health of children born to mothers treated with interventions for threatened preterm delivery (cervical cerclage) might also reflect better access of such mothers and their children to health care.
Decreased PCHI
Lower positive child health was associated with chronic medical conditions in the mother, such as obesity, asthma, and diabetes. Maternal obesity is associated with neonatal inflammation18,19,20 and we have previously reported associations between neonatal inflammation and adverse neurodevelopmental outcomes in the ELGAN cohort.21,22 Asthma also has been linked to inflammatory pathways and altered placental signaling in fetal development,23 neonatal complications.24 Maternal diabetes prior to pregnancy is associated with macrosomia at birth and obesity in the offspring.25 One explanation for our finding of worse health among children born to mothers who became eligible for Medicaid between their child’s birth and when the child reached 10 years is that having a child increases the family’s medical expenses, thus increasing the likelihood that the family will qualify for public assistance. In addition, mothers with children with disabilities are often unable to continue to work outside of the home due to the demands of caring for a child with a disability.
Stratification by race
For many antecedents of PCHI identified in this study (maternal asthma, aspirin consumption during pregnancy, cerclage, and plurality), we detected no interaction between race and the antecedent. On the other hand, assisted reproduction was associated with higher PCHI only among non-whites. A plausible explanation for this interaction of race and assisted reproduction is that assisted reproduction might be a stronger marker of socioeconomic resources among non-whites than among whites. We observed that prenatal maternal antibiotic treatment was associated with higher PCHI only among whites. Previous studies have suggested the use of antibiotics may be influenced by social and lifestyle factors.26 We are unable to propose plausible explanations for the other interactions that we observed between race and antecedents of PCHI, such as the observation that protein in the urine was associated higher PCHI among non-white participants. Caution is appropriate when interpreting the results of stratified analyses because stratum-specific associations are based on relatively smaller sample sizes. We suggest future studies to validate and build upon results observed here. Future studies should further assess race and related socioeconomic factors in mediation analysis as potential modifiers of the effects observed in the current study.
Strengths and limitations
Strengths of this study include the large sample that was relatively diverse with respect to sociodemographic attributes. A possible limitation of this study is that the outcomes previously obtained for the PCHI were primarily neurodevelopmental outcomes, rather than a broader profile of disorders, such as cardiometabolic and respiratory illnesses. This potentially limits the generalizability of the findings to other conditions outside the neurodevelopmental outcomes at 10 years of age. Lastly, of the original 966, the 77 study participants lost to follow-up were more likely to have indicators of social disadvantage, such as eligibility for public assistance. The bias from lost-to-follow-up children would therefore be expected to result in an underestimation of adverse outcomes in the cohort. However, given the low frequency of lost-to-follow-up children (8%), the magnitude of this bias very likely was small (Supplementary Tables S1 and S2).
Implications
Several findings reported here could have implications for researchers interested in practice, policy, or programs that target improvement in child health outcomes among individuals born extremely preterm. Most notable is the finding that correlates of lower socioeconomic status (SES) early in life were associated with worse child health later in life. Irrespective of their family’s household income, individuals born extremely preterm are supported by expensive medical care during their initial hospitalization (in neonatal intensive care). In about one-third of the ELGAN cohort, the cost of neonatal intensive care, which has been estimated to be around $200,000 per surviving infant for those born at 24–27 weeks of gestation, was borne by public insurance.27 Given this large investment in survival of individuals born extremely preterm, and observed associations between indicators of low SES and worse outcomes among survivors, it is reasonable to ask whether the public should invest more in evidence-based programs.28 This may take the form of increasing publicly funded developmental surveillance and developmentally supportive therapies for survivors of extremely preterm birth. This would serve the goal of improving child health among those individuals born into lower social economic households, which have limited financial resources with which to pay for interventions to promote their child’s development. In addition, further research to identify biosocial correlates of socioeconomic disadvantage that explain its association with reduced PCHI could identify more specific targets for interventions.
In addition to programs to support families caring for an infant discharged from neonatal intensive care, positive child health among individuals born extremely preterm might be promoted by prenatal programs to improve maternal health prior to conception and during pregnancy.29,30,31 Here we report that chronic maternal illnesses, such as pre-pregnancy obesity, asthma, and tobacco smoke exposure during pregnancy were associated with reduced PCHI at 10 years of age, suggesting that interventions to improve the health of mothers, including smoking cessation and weight reduction prior to pregnancy, might benefit not only the mother but also the later life health of her offspring.
Conclusions
Among infants born extremely preterm, pre-pregnancy and perinatal factors are associated with variation in the offspring’s overall health and development as much as 10 years later. Socioeconomic factors intertwined with race may also play an integral role in the associations between PCHI and antecedents, and needs to be investigated in future research. Interventions that target these early-life factors could have long-term benefits for individuals born extremely preterm.
References
Anderson, P. J. Neuropsychological outcomes of children born very preterm. Semin. Fetal Neonatal Med. 19, 90–96 (2014).
Linsell, L., Malouf, R., Morris, J., Kurinczuk, J. J. & Marlow, N. Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight: a systematic review. JAMA Pediatr. 169, 1162–1172 (2015).
Heeren, T. et al. Cognitive functioning at the age of 10 years among children born extremely preterm: a latent profile approach. Pediatr. Res. 82, 614–619 (2017).
Joseph, R. M. et al. Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res. 10, 224–232 (2017).
Douglass, L. M. et al. Cumulative incidence of seizures and epilepsy in ten-year-old children born before 28 weeks’ gestation. Pediatr. Neurol. 73, 13–19 (2017).
Kuban, K. C. et al. Cranial ultrasound lesions in the NICU predict cerebral palsy at age 2 years in children born at extremely low gestational age. J. Child Neurol. 24, 63–72 (2009).
Kuban, K. C. et al. Girls and boys born before 28 weeks gestation: Risks of cognitive, behavioral, and neurologic outcomes at age 10 years. J. Pediatr. 173, 69–75. e61 (2016).
Bangma, J. T. et al. Assessing positive child health among individuals born extremely preterm. J. Pediatr. 202, 44–49.e4 (2018).
Von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 4, e296 (2007).
Yudkin, P. L., Aboualfa, M., Eyre, J. A., Redman, C. W. & Wilkinson, A. R. New birthweight and head circumference centiles for gestational ages 24 to 42 weeks. Early Hum. Dev. 15, 45–52 (1987).
Leviton, A. et al. Maternal infection, fetal inflammatory response, and brain damage in very low birth weight infants. Pediatr. Res. 46, 566–566 (1999).
Bright, H. R. et al. Neurocognitive outcomes at 10 years of age in extremely preterm newborns with late-onset bacteremia. J. Pediatr. 187, 43–49 (2017).
Scott, M. N. et al. Neurocognitive correlates of attention-deficit hyperactivity disorder symptoms in children born at extremely low gestational age. J. Dev. Behav. Pediatr. 38, 249–259 (2017).
Joseph, R. M., O’Shea, T. M., Allred, E. N., Heeren, T. & Kuban, K. K. Maternal educational status at birth, maternal educational advancement, and neurocognitive outcomes at age 10 years among children born extremely preterm. Pediatr. Res. 83, 767 (2018).
Logan, J. W. et al. Neurocognitive function of 10 year-old multiples born extremely preterm. J. Perinatol. 39, 237–247 (2019).
Jackson, W. M. et al. Risk factors for chronic lung disease and asthma differ among children born extremely preterm. Pediatr. Pulmonol. 53, 1533–1540 (2018).
Wood, C. T. et al. Antecedents of obesity among children born extremely preterm. Pediatrics 142, e20180519 (2018).
van der Burg, J. W. et al. The role of systemic inflammation linking maternal BMI to neurodevelopment in children. Pediatr. Res. 79, 3 (2015).
van der Burg, J. W. et al. Are extremely low gestational age newborns born to obese women at increased risk of cerebral palsy at 2 years? J. child Neurol. 33, 216–224 (2018).
van der Burg, J. W. et al. Maternal obesity and attention-related symptoms in the preterm offspring. Early Hum. Dev. 115, 9–15 (2017).
Kuban, K. C. et al. Systemic inflammation and cerebral palsy risk in extremely preterm infants. J. Child Neurol. 29, 1692–1698 (2014).
Allred, E. N. et al. Systemic inflammation during the first postnatal month and the risk of attention deficit hyperactivity disorder characteristics among 10 year-old children born extremely preterm. J. Neuroimmune Pharmacol. 12, 531–543 (2017).
Meakin, A. S. et al. Review: placental adaptations to the presence of maternal asthma during pregnancy. Placenta 54, 17–23 (2017).
Murphy, V. et al. The risk of congenital malformations, perinatal mortality and neonatal hospitalisation among pregnant women with asthma: a systematic review and meta-analysis. BJOG Int. J. Obstet. Gynaecol. 120, 812–822 (2013).
Yessoufou, A. & Moutairou, K. Maternal diabetes in pregnancy: early and long-term outcomes on the offspring and the concept of “metabolic memory”. Exp. Diabetes Res. 2011, 218598 (2011).
Stokholm, J. et al. Prevalence and predictors of antibiotic administration during pregnancy and birth. PLoS ONE 8, e82932 (2013).
Phibbs, C. S. & Schmitt, S. K. Estimates of the cost and length of stay changes that can be attributed to one-week increases in gestational age for premature infants. Early Hum. Dev. 82, 85–95 (2006).
Spittle, A., Orton, J., Anderson, P. J., Boyd, R. & Doyle, L. W. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 11, 3–4 (2015).
Byerley, B. M. & Haas, D. M. A systematic overview of the literature regarding group prenatal care for high-risk pregnant women. BMC Pregnancy Childbirth 17, 329 (2017).
Williamson, G. R., O’Connor, A. & Kayleigh, E. J. Women’s experiences of personalised support for asthma care during pregnancy: A systematic review of the literature. BMC Pregnancy Childbirth 17, 69 (2017).
Yeo, S., Walker, J. S., Caughey, M. C., Ferraro, A. M. & Asafu-Adjei, J. K. What characteristics of nutrition and physical activity interventions are key to effectively reducing weight gain in obese or overweight pregnant women? A systematic review and meta-analysis. Obes. Rev. 18, 385–399 (2017).
Acknowledgments
We gratefully acknowledge the contributions of the ELGAN subjects the ELGAN subjects’ families, as well as the colleagues listed below. This study was supported by grants from the National Institute of Neurological Disorders and Stroke (5U01NS040069-05; 2R01NS040069-06A2), the National Institute of Child Health and Human Development (5R01HD092374-02 and 5P30HD018655-34), the Office of the NIH Director (1UG3OD023348-01), NIH training grant (T32-ES007018), and National Institute of Nursing Research (1K23NR017898-01).
ELGAN-2 Members
Project Lead for ELGAN-2: Julie V. Rollins, MA.
Site Principal Investigators
Baystate Medical Center, Springfield, MA: Bhahvesh Shah, MD; Rachana Singh, MD, MS. Boston Children’s Hospital, Boston, MA: Linda Van Marter, MD, MPH and Camilla Martin, MD, MPH; Janice Ware, Ph.D. Tufts Medical Center, Boston, MA: Cynthia Cole, MD; Ellen Perrin, MD. University of Massachusetts Medical School, Worcester, MA: Frank Bednarek, MD; Jean Frazier, MD. Yale University School of Medicine, New Haven, CT: Richard Ehrenkranz, MD; Jennifer Benjamin, MD. Wake Forest University, Winston-Salem, NC: T. Michael O’Shea, MD, MPH. Wake Forest University, Winston-Salem, NC: T. Michael O’Shea, MD, MPH. University of North Carolina, Chapel Hill, NC: Carl Bose, MD; Diane Warner, MD, MPH. East Carolina University, Greenville, NC: Steve Engelke, MD. Helen DeVos Children’s Hospital, Grand Rapids, MI: Mariel Poortenga, MD; Steve Pastyrnak, Ph.D. Sparrow Hospital, East Lansing, MI: Padu Karna, MD; Nigel Paneth, MD, MPH; Madeleine Lenski, MPH. University of Chicago Medical Center, Chicago, IL: Michael Schreiber, MD; Scott Hunter, Ph.D; Michael Msall, MC. William Beaumont Hospital, Royal Oak, MI: Danny Batton, MD; Judith Klarr, MD.
Site Study Coordinators
Baystate Medical Center, Springfield, MA: Karen Christianson, RN; Deborah Klein, BSM, RN. Boston Children’s Hospital, Boston MA: Maureen Pimental, BA; Collen Hallisey, BA; Taryn Coster, BA. Tufts Medical Center, Boston, MA: Ellen Nylen, RN; Emily Neger, MA; Kathryn Mattern, BA. University of Massachusetts Medical School, Worcester, MA: Lauren Venuti, BA; Beth Powers, RN; Ann Foley, EdM. Yale University School of Medicine, New Haven, CT: Joanne Williams, RN; Elaine Romano, APRN. Wake Forest University, Winston-Salem, NC: Debbie Hiatt, BSN (deceased); Nancy Peters, RN; Patricia Brown, RN; Emily Ansusinha, BA. University of North Carolina, Chapel Hill, NC: Gennie Bose, RN; Janice Wereszczak, MSN; Janice Bernhardt, MS, RN. East Carolina University, Greenville, NC: Joan Adams (deceased); Donna Wilson, BA, BSW. Nancy Darden-Saad, BS, RN. Helen DeVos Children’s Hospital, Grand Rapids, MI: Dinah Sutton, RN; Julie Rathbun, BSW, BSN. Sparrow Hospital, East Lansing, MI: Karen Miras, RN, BSN; Deborah Weiland, MSN. University of Chicago Medical Center, Chicago, IL: Grace Yoon, RN; Rugile Ramoskaite, BA; Suzanne Wiggins, MA; Krissy Washington, MA; Ryan Martin, MA; Barbara Prendergast, BSN, RN. William Beaumont Hospital, Royal Oak, MI: Beth Kring, RN.
Psychologists
Baystate Medical Center, Springfield, MA: Anne Smith, Ph.D.; Susan McQuiston, Ph.D. Boston Children’s Hospital: Samantha Butler, Ph.D.; Rachel Wilson, Ph.D.; Kirsten McGhee, Ph.D.; Patricia Lee, Ph.D.; Aimee Asgarian, Ph.D.; Anjali Sadhwani, Ph.D.; Brandi Henson, PsyD. Tufts Medical Center, Boston MA: Cecelia Keller, PT, MHA; Jenifer Walkowiak, Ph.D.; Susan Barron, Ph.D. University of Massachusetts Medical School, Worcester MA: Alice Miller, PT, MS; Brian Dessureau, Ph.D.; Molly Wood, Ph.D.; Jill Damon-Minow, Ph.D. Yale University School of Medicine, New Haven, CT: Elaine Romano, MSN; Linda Mayes, Ph.D.; Kathy Tsatsanis, Ph.D.; Katarzyna Chawarska, Ph.D.; Sophy Kim, Ph.D.; Susan Dieterich, Ph.D.; Karen Bearrs, Ph.D. Wake Forest University Baptist Medical Center, Winston-Salem NC: Ellen Waldrep, MA; Jackie Friedman, Ph.D.; Gail Hounshell, Ph.D.; Debbie Allred, Ph.D. University Health Systems of Eastern Carolina, Greenville, NC: Rebecca Helms, Ph.D.; Lynn Whitley, Ph.D. Gary Stainback, Ph.D. University of North Carolina at Chapel Hill, NC: Lisa Bostic, OTR/L; Amanda Jacobson, PT; Joni McKeeman, Ph.D.; Echo Meyer, Ph.D. Helen DeVos Children’s Hospital, Grand Rapids, MI: Steve Pastyrnak, Ph.D. Sparrow Hospital, Lansing, MI: Joan Price, EdS; Megan Lloyd, MA, EdS. University of Chicago Medical Center, Chicago, IL: Susan Plesha-Troyke, OT; Megan Scott, Ph.D. William Beaumont Hospital, Royal Oak, MI: Katherine M. Solomon, Ph.D.; Kara Brooklier, Ph.D.; Kelly Vogt, Ph.D.
Author information
Authors and Affiliations
Consortia
Contributions
All authors listed on this manuscript contributed to all three types of substantial contributions listed in Pediatric Research instructions to authors. Bi-weekly conference calls were held throughout the processes of brainstorming, method development, writing, and reviewing of this manuscript in which all authors participated.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the ELGAN study are given below the Acknowledgments.
Supplementary information
Rights and permissions
About this article
Cite this article
Bangma, J.T., Kwiatkowski, E., Psioda, M. et al. Early life antecedents of positive child health among 10-year-old children born extremely preterm. Pediatr Res 86, 758–765 (2019). https://doi.org/10.1038/s41390-019-0404-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0404-x
This article is cited by
-
Child and family factors associated with positive outcomes among youth born extremely preterm
Pediatric Research (2023)
-
Environmental influences on child health outcomes: cohorts of individuals born very preterm
Pediatric Research (2023)
-
Placental programming, perinatal inflammation, and neurodevelopment impairment among those born extremely preterm
Pediatric Research (2021)
-
Families’ perspectives on monitoring infants’ health and development after discharge from NICUs
Pediatric Research (2021)
-
Psychosocial and medical adversity associated with neonatal neurobehavior in infants born before 30 weeks gestation
Pediatric Research (2020)