Abstract
Objectives
To investigate the incidence of seizures and short-term mortality associated with seizures in children undergoing extracorporeal membrane oxygenation (ECMO).
Methods
PubMed, Embase, and Web of Science were searched from inception to September 2021. Study quality was assessed using the Newcastle-Ottawa Scale. Random effects meta-analysis was conducted.
Results
Fourteen studies met the inclusion criteria for quantitative meta-analysis. The cumulative estimate of seizure incidence was 15% (95% CI: 12–17%). Studies using electroencephalography reported a higher incidence of seizures compared with those using electro-clinical criteria (19% vs. 9%, P = 0.034). Furthermore, 75% of seizures were subclinical. Children receiving extracorporeal cardiopulmonary resuscitation (ECPR) exhibited a higher incidence of seizures compared to children with respiratory and cardiac indications. Seizure incidence was higher in patients undergoing venoarterial (VA) ECMO compared with venovenous (VV) ECMO. The pooled odds ratio of mortality was 2.58 (95% CI: 2.25–2.95) in those developed seizures.
Conclusion
The incidence of seizures in children requiring ECMO was 15% and majority of seizures were subclinical. The incidence of seizures was higher in patients receiving ECPR than in those with respiratory and cardiac indications. Seizures were more frequent in patients undergoing VA ECMO than VV ECMO. Seizures were associated with increased short-term mortality.
Impact
-
The incidence of seizures in children undergoing extracorporeal membrane oxygenation (ECMO) was ~15% and majority of the seizures were subclinical.
-
Seizures were associated with increased short-term mortality.
-
Risk factors for seizures were extracorporeal cardiopulmonary resuscitation and venoarterial ECMO.
-
Electroencephalography (EEG) monitoring is recommended in children undergoing ECMO and further studies on the optimal protocol for EEG monitoring are necessary.
Similar content being viewed by others
Introduction
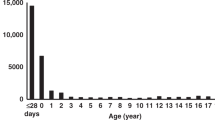
Extracorporeal membrane oxygenation (ECMO) was first successfully applied in 1971 for the rescue of neonates and in 1972 for the support of adult patients with reversible respiratory failure1,2. Since then, it has been increasingly applied as a life support technique for both children and adult patients with severe but potentially reversible cardiopulmonary diseases3,4. Despite the benefit of decreasing mortality, ECMO is associated with an increased burden of neurological complications. Children receiving ECMO represent a unique patient population, which is vulnerable to both focal and diffuse neurological impairment5. In children, the ECMO-related neurological injury, including seizures, hypoxic-ischemic brain injury, ischemic stroke, intracerebral hemorrhage and brain death, has been reported to be up to 20%6. In comparison, the incidence of neurological complications in general pediatric intensive care unit was estimated to be 13%7.
The reported incidence of seizures varied substantially in children receiving ECMO, ranging between 6 and 23%8,9,10. However, most of these previous studies were single center studies with heterogenous patient populations and indications for ECMO use, which lowered the general applicability of the results. In addition, children receiving ECMO who developed seizures have been reported to exhibit poor prognosis and high short-term mortality9,11. However, some studies have revealed that the presence of seizures did not increase mortality in pediatric patients10,12,13. In the present study, we performed a systematic review and meta-analysis to determine the incidence of seizures in children receiving ECMO and to investigate whether the presence of seizures is associated with increased short-term mortality.
Materials and methods
Search strategy
PubMed, Embase and Web of Science were searched to identify studies reporting the prevalence of seizures in children receiving ECMO and the association of seizures with the short-term mortality of children. The search focused on the following key words: “extracorporeal membrane oxygenation”, “extracorporeal cardiopulmonary resuscitation”, “extracorporeal life support”, “seizures”, “status epilepticus”, “epileptic state”, “neurologic outcome”, “neurologic prognosis”, “neurological complication” and “neurological injury”. The search process terminated in September 2021. The detailed search strategy was provided in the Supplementary Materials.
Study selection and data extraction
The search results were independently reviewed by 2 authors (G. L. and Y. L.) for eligibility with any disagreement resolved by consensus. Studies fulfilling the following criteria were included: (1) Clinical trials, cohort studies, case control studies or case reports/series reporting the incidence of seizures and/or the association of seizures with patient mortality; (2) patient population was children (age ≤ 18), or the data of the children population was available; (3) case number was more than 5. References of the included studies were screened for eligibility. The study period and institution for patient recruitment were carefully compared for exclusion of studies with patient population overlap. Studies from a single center that participated in the Extracorporeal Life Support Organization (ELSO) with an overlapping study period with the ELSO report were excluded if the ELSO report was included.
Information was extracted from the eligible studies by 2 authors (G. L. and Y. L.) independently, and this included number of patients, number of patients with seizures, patient types (neonatal or pediatric), study period, patient number, indication for ECMO, cannulation methods (venoarterial [VA] or venovenous [VV]), ECMO support days, seizure detection methods, proportion of subclinical nonconvulsive seizures, survival rate for patients with seizures and survival rate for patients without seizures. The outcomes of interest were (1) Incidence of seizures; (2) odds ratio of mortality for patients with seizures compared to patients without seizures.
Quality assessment
Two authors (Y. Z. and Q. F.) independently evaluated the risk of bias of the included studies using the Newcastle-Ottawa Scale (NOS) for assessment of the quality of nonrandomized studies in meta-analysis. The NOS contained 3 domains, which were patient selection, comparability, and assessment of outcome or exposure. The quality of studies was considered high with low risk of bias when the NOS score was 6 points or more.
Statistical analyses
The present systematic review and meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) principles. The incidence of seizures was calculated with Freeman-Tukey double arcsine transformation14. The heterogeneity was assessed using the I2. I2 ≥ 50% indicates a high degree of heterogeneity and I2 < 50% indicates low degree of heterogeneity. A random-effect model was used to estimate the pooled incidence of seizures and the pooled odd ratio of mortality. For the incidence of seizures, subgroup analysis was performed for seizure diagnosis criteria, proportion of subclinical nonconvulsive seizures, indications of ECMO, ECMO cannulation methods and patient types. Publication bias was assessed using the Egger regression test. P < 0.05 was considered to indicate a statistically significant difference. The analysis was performed using STATA version 14.0 (StataCorp LP, College Station, TX).
Results
Study selection and quality assessment
Figure 1 shows the selection process following the PRISMA principle. A total of 778 articles were identified, of which 648 articles remained after duplication removal. Based on our criteria, 566 articles were excluded, leaving 82 articles eligible for full-text screening. A total of 14 articles remained for quantitative meta-analysis6,9,10,11,12,13,15,16,17,18,19,20,21,22. All 14 studies were retrospective cohort studies. Majority of the studies were single center studies (10/14, 71%). Three studies analyzed solely neonatal patients and the remaining 11 studies analyzed neonatal and pediatric patients. Table 1 summarizes the basic characteristics of the included studies.
Table 2 presents the results of quality assessment for all studies using NOS. All studies were judged to be of high quality and low risk of bias with a median NOS score of 6.
Incidence of seizures in children undergoing ECMO and subgroup analysis
Twelve studies6,9,10,11,13,15,16,17,18,20,21,22 with a total of 21,930 patients were included for estimation of the incidence of seizures among children undergoing ECMO. In meta-analysis, the pooled incidence of seizures was 15% (95% confidence interval [CI]: 12–17%, I2 = 95.9%, P < 0.001; Fig. 2).
In all 12 studies, we compared seizure incidences between studies that applied electroencephalography (EEG) for the diagnosis of seizures and those using electro-clinical criteria. The pooled incidence of seizures for studies using EEG was 19% (95 CI: 14–24%; Fig. 3A), which was significantly higher (P = 0.034) than that of studies using electro-clinical criteria with 9% (95 CI: 5–13%; Fig. 3A).
A Forest plot of the incidence of seizures in studies that applied EEG for seizure diagnosis versus studies using electro-clinical criteria. B Forest plot of the proportion of subclinical non-convulsive seizure. C Forest plot of the incidence of seizures in patients with cardiac, respiratory, and ECPR indications, respectively. D Forest plot of the incidence of seizures in patients with venoarterial ECMO versus patients with venovenous ECMO. The incidence of seizures and proportion of subclinical seizures were calculated using a random-effects model. CI confidence interval, ECPR extracorporeal cardiopulmonary resuscitation, ECMO extracorporeal membrane oxygenation, EEG electroencephalography, ES estimate.
In 6 studies9,10,11,12,17,21 with a total of 440 patients, the proportion of subclinical nonconvulsive seizures was reported. In meta-analysis, the pooled proportion of subclinical seizures was 75% (95%: 63–76%; Fig. 3B).
In 9 studies9,10,11,12,13,15,16,17,21 with a total of 8268 patients, the incidence of seizures was reported for cardiac, respiratory, and extracorporeal cardiopulmonary resuscitation (ECPR) indications. The pooled incidence of seizures for children receiving ECMO with cardiac, respiratory, and ECPR indications was 15% (95% CI: 11–20%; Fig. 3C), 12% (95% CI: 7–17%; Fig. 3C), and 30% (95% CI: 22–39%; Fig. 3C), respectively. Children with ECPR indication had a higher incidence of seizures compared with children with respiratory indication (30% vs. 12%, P = 0.002) and children with cardiac indication (30% vs. 15%, P = 0.008). There was no significant difference of seizure incidence between children with cardiac and respiratory indications (15% vs. 12%, P = 0.33).
In 7 studies9,10,12,13,16,17,21 with a total of 4145 patients, the incidence of seizures was reported for VA ECMO and VV ECMO. The pooled incidence of seizures for VA ECMO was 22% (95% CI: 15–29%, Fig. 3D), which was more frequent (P = 0.03) than that of VV ECMO with 4% (95% CI: 0–15%, Fig. 3D).
In 7 studies6,10,15,16,17,20,22 with a total of 21,475 patients, the incidence of seizures was available for neonatal and pediatric populations. The pooled incidence of seizures was 11% (95% CI: 6–16%; Supplementary materials, Fig S1) and 8% (95% CI: 4–13%; Supplementary materials, Fig. S1) for neonatal and pediatric populations, respectively. There was no statistical difference between neonatal and pediatric populations in terms of the incidence of seizures (P = 0.14).
In summary, the pooled incidence of seizures in children undergoing ECMO was 15% (Fig. 2). Studies using EEG reported a higher incidence of seizures compared with studies using electro-clinical criteria (19% vs. 9%, P = 0.034; Fig. 3A). The pooled proportion of subclinical seizures was 75% (Fig. 3B). Children with ECPR indications had a higher incidence of seizures compared to those with cardiac (30% vs. 15%, P = 0.008; Fig. 3C) and respiratory (30% vs. 12%, P = 0.002; Fig. 3C) indications. Children receiving VA ECMO had a higher incidence of seizures compared to those receiving VV ECMO (22% vs. 4%, P = 0.03; Fig. 3D). There was no significant difference regarding the incidence of seizures between neonatal and pediatric patients (11% vs. 8%, P = 0.14; Fig S1).
Odds ratio of mortality for children who develop seizures during ECMO
In 9 studies9,10,11,13,15,16,17,19,21 with a total of 8918 patients, mortality was reported separately for children with seizures and without seizures. In meta-analysis, the pooled odds ratio of mortality for children who developed seizures during ECMO was 2.58 (95% CI: 2.25–2.95, I2 = 0, P = 0.55; Fig. 4).
Publication bias
The Egger regression test revealed no publication bias for both overall seizure incidences (P = 0.10) and odds ratio of mortality (P = 0.76).
Discussion
The use of ECMO has increased over the last decade3, and this has also been recommend for pediatric COVID-19 patients with acute respiratory distress syndrome and/or cardiac failure23. Seizure is one of the common neurological complications in children receiving ECMO24. The present meta-analysis revealed that seizures occurred in 15% of children receiving ECMO. A recent systematic review estimated the incidence of seizures to be ~20% based on several single studies24. Reported seizure incidences among children receiving ECMO vary substantially in literature, ranging between 7 and 40%. The wide range of seizures incidence may be due to the use of different criteria for seizure detection and the emphasis of different ECMO indications. Studies using EEG monitoring reported a higher incidence of seizures than those using electro-clinical criteria. Majority (75%) of the seizures were nonconvulsive. Therefore, studies may underestimate the incidence of seizures if continuous EEG is not applied17,24. Children requiring ECPR had the highest incidence of seizures, which was markedly higher than that of patients with respiratory and cardiac indications. In a previous ELSO report, neonatal patients with ECPR indication had a higher chance of developing neurological injury (39%) compared with those with respiratory (22%) and cardiac (28%) indications6. Cardiac arrest is a known risk factor for hypoxic ischemic injury related to seizures5. It may explain the high incidence of seizures in this type of patients.
Seizures were more frequent in patients receiving VA ECMO than in patients receiving VV ECMO. A recent meta-analysis of the adult population reported that patients receiving VA ECMO had higher rates of acute brain injury than patients receiving VV ECMO25. However, no meta-analysis has looked specifically at children. The reasons for the high incidence of seizures in children with VA ECMO are complex. Disruption of cerebral autoregulation has been demonstrated in animal models due to alteration of cerebral perfusion and microcirculatory impairment caused by loss of pulsatile blood flow in VA ECMO26,27. Decreased regional cerebral oxygen saturation in patients with VA ECMO is related to secondary neurologic injury28. Furthermore, VA ECMO is associated with Harlequin syndrome, a rare condition causing by the antegrade deoxygenated blood from the left ventricle29. It can result in hypoxia of the upper body and brain, which increases the risk of seizures.
In meta-analysis, seizures were associated with higher short-term mortality. Seizures have been demonstrated to increase both cerebral metabolism and intracranial pressure30, which may potentially increase morbidity and mortality in patients with a hypo-perfused brain. Additionally, a previous study also reported that children requiring ECMO who developed seizures had an increased risk of long-term cognitive impairment and cerebral palsy31. Therefore, it is important for prompt recognition of seizures to identify children who are at risk of brain injury and worse clinical outcomes. The American Clinical Neurophysiology Society Consensus Statement recommends the use of continuous EEG in critically ill children receiving ECMO for at least 24 hours32. Moreover, even when seizures are absent, the detection of EEG background abnormalities, such as asymmetry and state change, is associated with neuroimaging abnormalities11,33,34 (e.g., brain edema, intracranial hemorrhage and cerebral ischemia) and unfavorable neurological outcomes35,36. However, practical guidelines for neurocritical care of ECMO patients are still lacking9,37. The present meta-analysis could provide evidence to strengthen the recommendation of EEG application in children undergoing ECMO.
The strength of this systematic review and meta-analysis was the inclusion of a large number of cohorts. We included all studies without population overlap reporting seizure incidences regardless of criteria for seizure diagnosis, indication for ECMO and cannulation methods of ECMO, which helped us to identify risk factors for seizure development in this patient population. However, there were several limitations. First, a number of the included studies did not perform continuous EEG for all the consecutive patients, which might under-represent the prevalence of seizures in children receiving ECMO. Therefore, the pooled estimate of seizure incidence of our study may under-estimate the real incidence of seizure in this population. Future prospective studies with continuous EEG to monitor seizure occurrence are required. Second, since information regarding the timing of seizure occurrence was limited, it was infeasible to comment for the best timing to start EEG monitoring. The optimal timing for EEG in children undergoing ECMO remains a field to be explored. Third, analysis of the association between burden of seizures and short-term mortality was not available due to the limited information. Finally, the studies included in this meta-analysis spanned from 1973 to 2010, where ECMO technology and ECMO practice have undergone substantial changes. This may be a cause of heterogeneity. Given the high heterogeneity, all estimates were generated using a random-effect model.
Conclusion
The incidence of seizures in children receiving ECMO was ~15%, and seizures were commonly subclinical. Seizures were more frequent in patients receiving ECMO for ECPR indications than in patients receiving ECMO for respiratory and cardiac indications. Seizures were more frequent in patients receiving VA ECMO than in patients receiving VV ECMO. The presence of seizures was associated with increased short-term mortality. Further studies to explore the optimal protocol for EEG monitoring are required.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
White, J. J., Andrews, H. G., Risemberg, H., Mazur, D. & Haller, J. A. Jr. Prolonged respiratory support in newborn infants with a membrane oxygenator. Surgery 70, 288–296 (1971).
Hill, J. D. et al. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). use of the bramson membrane lung. N. Engl. J. Med. 286, 629–634 (1972).
Thiagarajan, R. R. et al. Extracorporeal life support organization registry international report 2016. ASAIO J. 63, 60–67 (2017).
Barbaro, R. P. et al. Extracorporeal membrane oxygenation for Covid-19: evolving outcomes from the international extracorporeal life support organization registry. Lancet 398, 1230–1238 (2021).
Abend, N. S., Dlugos, D. J. & Clancy, R. R. A review of long-term eeg monitoring in critically ill children with hypoxic-ischemic encephalopathy, congenital heart disease, ecmo, and stroke. J. Clin. Neurophysiol. 30, 134–142 (2013).
Polito, A. et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. an analysis of elso registry data. Intensive Care Med. 39, 1594–1601 (2013).
Raghu, V. K. et al. Neurological complications acquired during pediatric critical illness: exploratory “mixed graphical modeling” analysis using serum biomarker levels. Pediatr. Crit. Care Med. 22, 906–914 (2021).
Mehta, A. & Ibsen, L. M. Neurologic complications and neurodevelopmental outcome with extracorporeal life support. World J. Crit. Care Med. 2, 40–47 (2013).
Okochi, S. et al. Prevalence of seizures in pediatric extracorporeal membrane oxygenation patients as measured by continuous electroencephalography. Pediatr. Crit. Care Med. 19, 1162–1167 (2018).
Cook, R. J. et al. Electrographic seizures and brain injury in children requiring extracorporeal membrane oxygenation. Pediatr. Neurol. 108, 77–85 (2020).
Yuliati, A. et al. Prevalence of seizures and risk factors for mortality in a continuous cohort of pediatric extracorporeal membrane oxygenation patients. Pediatr. Crit. Care Med. 21, 949–958 (2020).
Piantino, J. A. et al. Nonconvulsive seizures are common in children treated with extracorporeal cardiac life support. Pediatr. Crit. Care Med. 14, 601–609 (2013).
Bauer Huang, S. L. et al. Seizures are associated with brain injury in infants undergoing extracorporeal membrane oxygenation. J. Child Neurol. 36, 230–236 (2021).
Miller, J. J. The Inverse of the Freeman – Tukey Double Arcsine Transformation. Am. Stat. 32, 138–138 (1978).
Streletz, L. J. et al. Utility of serial eegs in neonates during extracorporeal membrane oxygenation. Pediatr. Neurol. 8, 190–196 (1992).
Zwischenberger, J. B. et al. Complications of neonatal extracorporeal membrane oxygenation. collective experience from the extracorporeal life support organization. J. Thorac. Cardiovasc Surg. 107, 838–848 (1994).
Lin, J. J. et al. Electrographic seizures in children and neonates undergoing extracorporeal membrane oxygenation. Pediatr. Crit. Care Med. 18, 249–257 (2017).
LaRovere, K. L. et al. Patterns of head computed tomography abnormalities during pediatric extracorporeal membrane oxygenation and association with outcomes. Pediatr. Neurol. 73, 64–70 (2017).
Morell, E. et al. Extracorporeal membrane oxygenation in pediatric pulmonary hypertension. Pediatr. Crit. Care Med. 21, 256–266 (2020).
Trivedi, P. et al. Clinical outcomes of neonatal and pediatric extracorporeal life support: a seventeen-year, single institution experience. Artif. Organs 43, 1085–1091 (2019).
Hassumani, D. O., Shan, M., Mastropietro, C. W., Wing, S. E. & Friedman, M. L. Seizures in children with cardiac disease on extracorporeal membrane oxygenation. Neurocrit Care 36, 157–163 (2021).
Hervey-Jumper, S. L. et al. Neurological complications of extracorporeal membrane oxygenation in children. J. Neurosurg. Pediatr. 7, 338–344 (2011).
Kache, S. et al. Covid-19 Picu guidelines: for high- and limited-resource settings. Pediatr. Res. 88, 705–716 (2020).
Said, A. S., Guilliams, K. P. & Bembea, M. M. Neurological monitoring and complications of pediatric extracorporeal membrane oxygenation support. Pediatr. Neurol. 108, 31–39 (2020).
Shoskes, A. et al. Brain injury is more common in venoarterial extracorporeal membrane oxygenation than venovenous extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit. Care Med. 48, 1799–1808 (2020).
Ingyinn, M., Lee, J., Short, B. L. & Viswanathan, M. Venoarterial extracorporeal membrane oxygenation impairs basal nitric oxide production in cerebral arteries of newborn lambs. Pediatr. Crit. Care Med. 1, 161–165 (2000).
Short, B. L., Walker, L. K., Bender, K. S. & Traystman, R. J. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr. Res. 33, 289–294 (1993).
Khan, I. et al. Regional cerebral oximetry as an indicator of acute brain injury in adults undergoing veno-arterial extracorporeal membrane oxygenation-a prospective pilot study. Front Neurol. 9, 993 (2018).
Tsangaris, A. et al. Overview of veno-arterial extracorporeal membrane oxygenation (Va-Ecmo) support for the management of cardiogenic shock. Front Cardiovasc Med. 8, 686558 (2021).
Vespa, P. M. et al. Increased incidence and impact of nonconvulsive and convulsive seizures after traumatic brain injury as detected by continuous electroencephalographic monitoring. J. Neurosurg. 91, 750–760 (1999).
Parish, A. P., Bunyapen, C., Cohen, M. J., Garrison, T. & Bhatia, J. Seizures as a predictor of long-term neurodevelopmental outcome in survivors of neonatal extracorporeal membrane oxygenation (Ecmo). J. Child Neurol. 19, 930–934 (2004).
Herman, S. T. et al. Consensus statement on continuous eeg in critically ill adults and children, part i: indications. J. Clin. Neurophysiol. 32, 87–95 (2015).
Amigoni, A. et al. Neurologic outcome in children after extracorporeal membrane oxygenation: prognostic value of diagnostic tests. Pediatr. Neurol. 32, 173–179 (2005).
Ostendorf, A. P., Hartman, M. E. & Friess, S. H. Early electroencephalographic findings correlate with neurologic outcome in children following cardiac arrest. Pediatr. Crit. Care Med. 17, 667–676 (2016).
Hahn, J. S., Vaucher, Y., Bejar, R. & Coen, R. W. Electroencephalographic and neuroimaging findings in neonates undergoing extracorporeal membrane oxygenation. Neuropediatrics 24, 19–24 (1993).
Fox, J. et al. Eeg is a predictor of neuroimaging abnormalities in pediatric extracorporeal membrane oxygenation. J. Clin. Med. 9, 2512 (2020).
Cho, S. M., Farrokh, S., Whitman, G., Bleck, T. P. & Geocadin, R. G. Neurocritical care for extracorporeal membrane oxygenation patients. Crit. Care Med. 47, 1773–1781 (2019).
Funding
This work was supported by Sanming Project of Medicine in Shenzhen (No. SZSM202011005).
Author information
Authors and Affiliations
Contributions
G.L., Y.L. and H.Z. designed the study. G.L., Y.L., Y.Z. and Q.F. acquired the data. YL. and G.L. performed statistical analysis. G.L. and YL. drafted the manuscript. H.Z. revised the manuscript critically. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lin, G., Li, Y., Zhuang, Y. et al. Seizures in children undergoing extracorporeal membrane oxygenation: a systematic review and meta-analysis. Pediatr Res 93, 755–762 (2023). https://doi.org/10.1038/s41390-022-02187-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02187-5
This article is cited by
-
Seizures in children undergoing extracorporeal membrane oxygenation
Pediatric Research (2024)
-
Reply to: Seizures in children undergoing extracorporeal membrane oxygenation
Pediatric Research (2024)
-
Neonatal seizures during extra corporeal membrane oxygenation support
European Journal of Pediatrics (2024)