Abstract
Study design
Secondary analysis of aggregated case series data.
Objectives
To examine the effects of a high-fat/high-carbohydrate meal on leukocyte populations in adults with a chronic SCI.
Setting
University-based laboratories in British Columbia, Canada.
Methods
Ten individuals (M = 9) with a traumatic SCI (>1-year post-injury; M = 15.5 years; n = 2 sensory complete, n = 7 motor complete) participated in this study. Participants arrived fasted (≥12 h) prior to both the control (quiet sitting, no food/drink) and experimental meal conditions (high-fat/high-carb meal: 880 kcal, 52 g fat, 73 g carbohydrates, 29 g protein). Blood samples were taken in the fasted state and at 120-min post-meal/baseline in both conditions. Immune cell counts were assessed using multi-color flow cytometry.
Results
A significant time × condition interaction effect was seen in CD3+, CD4+, and CD8+ T cells as well as CD56+ and CD3+/CD56+ natural killer (NK) cells (p < 0.05). CD14+/CD16+ monocytes and CD19+ B cells approached a significant time × condition interaction (p < 0.07). A main effect of time was observed in CD19+ B cells (p < 0.05). Cell counts for T-lymphocytes and NK cells followed the general trend of an increase in the control condition from baseline to 120-min with no change observed following the experimental meal condition.
Conclusions
Following the HFHC meal, immune cells did not show the same general increase observed following the control condition. Future research is needed to determine if there are any potential consequences of these immune cell responses in immunosuppressed populations and if other factors (e.g., diurnal variation) might influence immune cell response.
Similar content being viewed by others
Introduction
People with a spinal cord injury (SCI) are at an increased risk of infection and subsequent rehospitalization. Indeed, research suggests that 30% of individuals with an SCI will be re-hospitalized one or more times within 1-year post-injury [1], often due to urinary tract infections, respiratory complications, or pressure ulcers [2]. In Canada, it is estimated that the lifetime economic burden per individual with an SCI ranges from $1.5 million to $3.0 million for individuals with paraplegia and tetraplegia, respectively [3]. Thus, efforts to understand immune system function in persons with an SCI could have implications for both preventing infections and reducing the personal and economic burdens.
Evidence suggests that nervous system impairments in persons with an SCI can lead to the dysregulation of both the endocrine and immune system and subsequent chronic low-grade inflammation [4]. The disruption in nervous system activation that accompanies a lesion to the spinal cord is thought to disrupt the flow of signals from the sympathetic nervous system (SNS) to lymphoid organs, causing dysfunctional immune cell mobilization and responses. In addition, disrupted the flow of returning or afferent signals from the peripheral to the central nervous system (CNS) may reduce the activity of immunoregulatory CNS neurons [5]. This alteration in SNS signaling may negatively impact the immune system’s ability to respond to infection, leaving individuals immunocompromised [6]. In addition to the immunosuppressive consequences of an SCI, the electrical conductance malfunction explanation may also be responsible for neuroimmunological dysfunction and the upregulation of circulating inflammatory mediators [7]. Chronic upregulation of inflammation may further impact the production and mobilization of immune cells [5].
The link between diet, immune responses, and chronic inflammation in both clinical and sub-clinical populations is becoming more apparent. Notably, following consumption of foods high in dietary fats, (i.e., typical “Western” diets), elevated fat levels can be observed in the blood, a condition referred to as postprandial lipemia. Although the cause of acute postprandial lipemia-induced inflammation is somewhat contested, it may be the result of bacterial endotoxin or the release of a proinflammatory stimulant from the gut following the consumption of high-fat foods [8]. In a systematic review exploring the effects of a high-fat/high-calorie meal on post-prandial inflammation, pro-inflammatory markers were reliably elevated when assessed within leukocytes, however, inconsistent detection exists for the impact of a high-fat meal on plasma cytokines [8]. Similarly, high-fat diets may be related to increased inflammatory biomarkers (i.e., C-reactive protein (CRP), interleukin (IL)−6, and fibrinogen), while diets high in fruit/vegetable consumption were correlated with lower levels of these inflammatory biomarkers [9]. These data suggest that poor dietary habits may impact immune function and/or influence the development of chronic low-grade inflammation [8,9,10].
Among persons with an SCI, a 12-week anti-inflammatory diet intervention significantly reduced circulating pro-inflammatory cytokines [10]. To the best of our knowledge, no studies have evaluated how circulating immune cells acutely respond to a high-fat/high-calorie or pro-inflammatory meal in persons with an SCI. Understanding the acute immune response to a pro-inflammatory meal is critical, given that prolonged exposure to a stimulus known to exert negative inflammatory effects may have more significant consequences in a population that already faces inflammatory and immunological risk. The purpose of this study was to determine whether consuming a high-fat/high-carbohydrate (HFHC) processed meal can alter circulating immune cell numbers in individuals with an SCI. We hypothesized that congruent with a pro-inflammatory response, participants’ immune cell count would be elevated following a single HFHC meal when compared to baseline immune cell counts and to a control condition.
Methods
Participants
This study is a secondary analysis of case series data (NCT03955523) in which participants completed a single session of exercise, consumed an experimental meal, and rested quietly. The pilot study objectives were to (1) compare the extent to which various biometric and self-report measures were responsive to exercise and dietary manipulations in people with SCI, and (2) assess the feasibility of measuring all the outcomes during the same visit. The results informed the selection of outcome measures for a subsequent randomized controlled trial [11]. Afterward, we aggregated participant data to test hypotheses about the effects of the experimental manipulations on the pre-defined primary outcomes (e.g., measures of inflammation, immune cells, pain). This paper reports on the effects of dietary manipulation and control conditions on immune cell counts.
Ten participants (M = 15.5 years post-injury; 60% tetraplegia; 70% reported motor complete injuries and 20% reported sensory complete injuries) with a chronic, traumatic SCI (nine males, one female) volunteered for this study. We recruited both males and females but testing for potential sex differences was beyond the study’s scope. Demographic information is in Table 1.
Inclusion criteria: ≥1-year post-SCI with injury level at or below the third cervical vertebrae; experience chronic neuropathic pain; have an upper-arm vein that could accommodate three venepunctures per day; have no contraindications to maximal exercise based on the latest guidelines of the American College of Sports Medicine; be meeting the scientific SCI exercise guidelines for improving fitness (i.e., 20 min of moderate-to-vigorous intensity aerobic activity two times per week, and strength training two times per week, consisting of three sets of 8–10 repetitions for each major muscle group [12]). Exclusion criteria: clinically diagnosed metabolic disorder (e.g., diabetes, hypothyroidism); progressive disease (e.g., multiple sclerosis) or mental disorder (e.g., depression); are pregnant; or were unable to refrain from taking anti-inflammatory medication (e.g., ibuprofen, naproxen) for at least 24 h before each trial day.
Protocol overview
This study included three research visits and one familiarization visit. Each visit occurred on separate days, at the same time, with a minimum washout period of 1-week between visits. The familiarization visit consisted of participants learning details of the study, providing informed consent, and completing an aerobic fitness test. It was followed by an experimental meal day, a control day, and an exercise day, the order of which was determined by computer-generated simple randomization using “Calculator.net”. The exercise intervention data is not part of this study.
Experimental meal protocol
Prior to consumption of the HFHC meal, a baseline blood sample was drawn from an antecubital vein by a trained phlebotomist. The participant was then given 30 min to eat a standardized breakfast meal (i.e., McDonalds McWrap with an extra hash brown—880 kcal, 52 g fat; 53.7% total kcal, 72 g carbohydrate; 33% total kcal, 29 g protein; 13.3% total kcal; see Table 2). The experimental meal provided was designed based on the literature to induce a postprandial inflammatory response [8, 13] and to be representative of a fast food meal that might be consumed; however, the macronutrient distribution was slightly higher in fat than the self-report of overall dietary patterns of some individuals with SCI [14, 15]. Following consumption, participants sat quietly for 90-min before a second blood sample was taken (i.e., 2-h post-baseline). Studies have shown inflammatory markers are altered as early as 1–2 h post-prandially [8, 16].
Control protocol
The control protocol was identical to the experimental meal protocol, except the 30-min window for consuming the HFHC meal was substituted for 30-min of additional quiet sitting. This visit was to account for biological variability in measured outcomes due to the passage of time.
Blood analyses
All blood samples were collected in EDTA tubes and immediately transported to an adjacent laboratory for analyses. Immune cell counts were quantified using the 8-Color Immunophenotyping Kit (130-120-640, Miltenyi Biotec) on a MACSQuant Analyzer 10 Flow Cytometer (Miltenyi Biotec). Cell numbers per milliliter of blood and percentage of total leukocytes were recorded for monocytes, neutrophils, T cells, B cells, and natural killer (NK) cells.
Flow cytometry protocol
Preparation of 8 color phenotyping kit
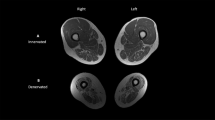
In total, 100 μl of whole blood kept at room temperature was transferred from the EDTA vacutainer to a 5 mL culture tube. In total, 10 μl of 8-color immunophenotyping cocktail (130-120-640, Miltenyi, CA, USA) and 10 μl of 7-AAD (130-111-568, Miltenyi, CA, USA) used as a viability marker were added directly to the sample. The stained sample was then gently vortexed for 3 s. Samples were covered with foil and placed on a rocker for 10 min. Following the first incubation, 2 mL of 1× red blood cell lysis solution (130-094-183, Miltenyi, CA, USA) was added. Samples were then gently vortexed for 3 s, covered with foil, and placed on the rocker for 15. Following the final incubation, samples were promptly analyzed on the flow cytometer (MacsQuant Analyzer, Miltenyi, CA, USA). Samples were analyzed using a variation of the express 8-color Panel, with instrument bank settings used to standardize laser and gain settings across the entire study. To obtain sufficient cell populations, 450 μl of prepared sample was processed at medium speed. The flow cytometer was calibrated according to the manufacturer’s instructions at the start of each day and the gating strategy was finalized using a Fluorescence Minus One control protocol to determine appropriate gating dimensions for measuring cell populations. The gating strategy layout can be observed in Fig. 1.
Flow cytometry gating strategy used to determine immune cell population and sub-(A) forward scatter (FSC) and side scatter (SSC) used to differentiate cells from debris. B Cells from gate A is separated into alive/dead populations. C Live cells are differentiated into the dump and non-dump cells, differentiating types of immune cells (i.e., monocytes, granulocytes, lymphocytes, debris). D Monocytes are differentiated from other cells based on the presence/absence of a cluster of differentiation (CD) 14/16 using Vioblue stain and SSC. E The three monocyte subgroups (classical, intermediate, nonclassical) are then isolated based on their degree of CD14/CD16 expression. F B cells are separated from non-B cells based on CD19+ PE- Vio770 stain. G From cells marked non-B cell in the previous gate, CD16+ neutrophils are isolated while remaining cells are moved to subsequent gate. H CD3+ T cells, NK cells, and NKT cell lymphocytes are differentiated. I From previously identified CD3+ T cells, CD4+ and CD8+ T cells can further be differentiated.
Statistical analysis
A linear mixed-effects model was used to assess the differences in leukocyte numbers within conditions over time using GraphPad Prism (v8.2.1). Condition, time, and their interactions were treated as repeated measures fixed factors and participants as a random factor. Prior to analyses, normality was assessed by visual inspection of Q-Q plots of the residuals, and variables that deviated substantially were natural log (Ln) transformed to meet assumptions. Statistical significance was set at p < 0.05. Significant interactions were followed up with pairwise comparisons between baseline and 120 min within condition using Sidak’s post-hoc test. Hedges’ g effect sizes were calculated and can be observed in Table 3 [17].
Cell responses in both conditions over time are reported with pairwise comparisons and effect sizes shown in Table 3. Results are presented below, organized according to cells that exhibited a significant condition × time interaction, a significant main effect of time, and no statistical significance.
Results
Cells that exhibited a difference between meal and control across time
A significant time × condition interaction effect was observed in CD3+ T cells (F(1,7) = 10.54 p = 0.014), CD4+ T cells (F(1,7) = 8.91 p = 0.02), CD8+ T cells (F(1,7) = 9.35 p = 0.018), as well as CD3+/CD56+ NK cells (F(1,7) = 7.128 p = 0.032) and CD56+ NK cells (F(1,7) = 5.957 p = 0.045). CD16+/CD14Dim monocytes (F(1,7) = 10.10, p = 0.056) and CD19+ B cells (F(1,7) = 10.10, p = 0.066) approached a significant interaction effect. The interaction effect reflected a general increase in cell counts in the control condition from baseline to 120-min but not in the meal condition. Post-hoc testing revealed significant increases from baseline to 120 min within the control condition for CD4+T cells (p = 0.022), CD16+ neutrophils (p = 0.001), CD19+B cells (p = 0.003), and CD56+ NK cells (p = 0.028). Post-hoc pairwise comparisons approached significance for increases from baseline to 120-min for CD8+T cells (p = 0.0504) and CD14++/CD16− monocytes (p = 0.085) in the control condition. No significant differences were found in pairwise comparisons in the meal condition for these cells. Table 3 presents leukocyte percent changes for the control and meal conditions. Figure 2 presents changes graphically.
Total cell count expressed in cells per milliliter of blood from baseline to 120-min post-baseline for (A) CD3+ T cells, (B) CD4+ T cells, (C) CD8+ T cells, (D) CD14++/CD16− monocytes, (E) CD14++/CD16+ monocytes, (F) CD14dim/CD16+ monocytes, (G) CD16+ neutrophils, (H) CD19+ B cells, (I) CD3+CD56+ NK-T cells, and (J) CD56+ NK cell. Empty circles and squares indicate the individual control and meal condition responses, respectively. Filled circles and squares indicate the control and meal condition averages, respectively. #Indicates a Significant Time × Condition Interaction Effect (p < 0.05). *Indicates a Significant main effect of Time (p < 0.05).
Cells where a main effect of time was detected
A main effect of time was observed for CD19+ B cells (F(1,9) = 6.42 p = 0.032). CD19+ B cell counts increased from baseline to 120-min.
Cells in which there was no interaction/condition effect
No significant time × condition interaction or main effect of time was observed in CD14+/CD16− monocytes, CD14+/CD16+ monocytes, or CD16+ neutrophils.
Discussion
The purpose of this study was to determine whether consuming an HFHC meal would alter circulating leukocyte numbers. Contrary to the hypothesis, most circulating immune cell counts increased from baseline to 120-min in the control condition, but not the experimental meal condition.
Cellular responses
Both T-lymphocytes and NK cells increased significantly following the control condition compared to relatively modest changes observed following the meal condition. Non-classical CD14dim/CD16+ monocytes tended to increase from baseline to 120-min in the control condition while trending toward a decrease following the meal condition. When activated, leukocytes can adhere to the vascular endothelium [18]. Lower circulating leukocyte concentrations in the meal condition versus the control condition at 120-min may therefore indicate activated immune cells that have evaded hematological detection [19]. Postprandial reductions in lymphocyte and monocyte counts may be due to the migration of cells into extravascular space following a meal-induced catecholamine release [19]. Increased postprandial leukocyte activation following exposure to an acute HFHC meal may be the result of endogenous bacterial endotoxin lipopolysaccharide, an inflammatory stimulus that is naturally present on gram-negative bacteria in the human gut and may cotransport with dietary fat [20].
In contrast, changes in classical (CD14++/CD16−) and intermediate (CD14++/CD16+) monocytes, along with neutrophils did not differ between the two conditions. These results partially align with evidence from the general population, whereby following an HFHC meal, postprandial activation of monocytes and neutrophils was significantly higher than in a control condition with no significant increases in lymphocyte counts [18]. Partial immune cell responses to an HFHC meal may be related to the activation of cell-specific cellular adhesion molecules (CAMs) which have been shown to increase following an acute HFHC meal [8] and result in the adhesion of cells to the vascular endothelium (i.e., reduced circulating concentrations). Whether SCI impacts the acute response of CAMs or other leukocyte adhesion processes following consumption of an HFHC meal will require further study.
Diurnal variation impacts circulating immune cell count
It is critical to observe diurnal variations in hematological outcomes, given that leukocyte concentrations significantly fluctuate throughout a 24-h cycle, whereby concentrations tend to increase throughout the day and peak close to midnight [21, 22]. In both conditions of the present study, participants arrived fasted for the baseline sample between 9:00 and 10:00 in the morning. Participants fasted for an additional 2-h within the control condition, whereby a general increase in circulating levels of lymphocytes such as CD3 + T cells (19%, g = 0.44), CD14+ monocytes (17%, g = 0.43), and CD16+ neutrophils (22%, g = 0.38) occurred. No differences were observed in the experimental meal condition.
Circadian rhythm modifications associated with an SCI may explain why participants did not display the anticipated increase in total leukocyte count from morning to noon. Interestingly, it has been shown that individuals with tetraplegia have blunted levels of the main circadian regulator melatonin [23]. Following an SCI, the mRNA expression of clock genes (i.e., period circadian regulator (PER)-1 and -2, and REV-ERBα) are disrupted. This may impact diurnal variations in immune cell counts given that PER-1 and -2 clock genes are strongly linked with the oscillations seen in leukocyte concentrations in able-bodied adults [24]. Therefore, it could be interpreted that the HFHC experimental meal provided in this study prevented a natural diurnal rise in leukocytes.
Potential implications for SCI-related immune dysfunction
Immunological dysfunction is a common secondary health complication among persons with an SCI and has been attributed in part to the loss of supraspinal nervous system control [4]. Reduced autonomic innervation plays a role in the commonly observed immune system deficiencies associated with an SCI, as lymphoid organs and the vast majority of lymphoid cells express adrenergic receptors which are stimulated by the autonomic nervous system [4]. Further, it has been demonstrated that both primary (e.g., bone marrow) and secondary (e.g., spleen) lymphoid organs receive autonomic innervation and contribute to the immune dysfunction observed following an SCI [4]. Although both innate and adaptive immune function is reduced following an SCI [25], injury level also plays an important role in the degree to which an SCI impacts immune function. For example, neutrophil phagocytic function is decreased in individuals with tetraplegia but not paraplegia with an injury below the level of T10 [6].
In addition, the phagocytic ability is significantly impaired, and NK cell cytotoxicity is reduced following an SCI, particularly for individuals with tetraplegia when compared to able-bodied controls and individuals with paraplegia who have sustained injuries below T10 [26]. NK cells are generally regarded as members of the innate immune system with some adaptive functionality that deals with both intra- and extra-cellular pathogens [26]. NK cells in particular have demonstrated an advanced cytotoxic ability that allows them to phagocytose a wide range of pathogens [27]. Reductions in lymphocyte numbers in the meal versus control condition in the current study, if corresponding with reduced function, could therefore impact the capacity of the adaptive immune response and remain an area ripe for study.
Limitations
Persons with an SCI are among the most physically inactive in society [28]. However, participants in this study were meeting the SCI exercise guidelines [12] which may limit generalizability to the SCI population. Further, it has been suggested that the prevalence of cardiometabolic disease (CMD) is between 31 and 72% in adults with SCI [29], which might limit the generalizability of our results as none of our participants reported having been diagnosed with a CMD. In addition, blood samples were collected at baseline and 120-min, which limits our ability to glean an understanding of the effects of an HFHC meal over a protracted period. It was not feasible to conduct tests of motor/sensory/autonomic completeness in our non-clinical research setting. Consequently, the generalizability of our results and the implications of injury completeness for their interpretation is unclear. Our sample included nine males and one female, which precluded any exploration of potential sex differences. Given the potential for sex differences in immune function [30], future research will be needed to determine if biological sex influences immune responses to dietary interventions in participants with SCI. Further, the experimental meal chosen for this study may not be typical of what is seen in some individuals with chronic SCI, indicating the need for research that explores the post-prandial responses to varying meal types in adults with chronic SCI.
Future directions
First, research should determine whether the differences in immune cell count following an HFHC meal, compared to control, are matched by changes in immune cell activation and/or function. Further, identifying whether consuming an HFHC fast food meal alters cells ability to respond to a challenge (e.g., pathogen) is critical in order to assess whether these variations in immune cell count have clinical relevance to immunity or risk of infection. Testing a wide range of experimental meals may provide valuable insight into the effects of varying food composition on immune cell numbers and functions among individuals with SCI. Finally, research should examine diurnal variations and 24-h leukocyte trends in individuals with SCI, as benchmarks for hematological variables are critically needed among this population.
Conclusions
In this study, we measured 11 immune cell phenotypes following an HFHC meal in participants with a chronic SCI. Results suggest that many cells responded differently between the control and meal conditions, with a general increase in total cell counts in the control condition, but not the meal condition. Whether these changes are due to a variance in the normal diurnal rhythm observed following an SCI or cell activation and remargination following the HFHC meal remains unclear. Regardless of the underlying mechanism(s), altered immune cell counts such as those observed following an HFHC meal may have important implications for overall immune function in people with an SCI.
References
National Spinal Cord Injury Statistical Center. J Spinal Cord Med. 2002:139–40.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–63. https://doi.org/10.1016/j.apmr.2004.03.016
Krueger H, Noonan VK, Trenaman LM, Joshi P, Rivers CS. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33:113–22.
Allison DJ, Ditor DS. Immune dysfunction and chronic inflammation following spinal cord injury. Spinal Cord. 2015;53:14–18. https://doi.org/10.1038/sc.2014.184
Cruse JM, Keith JC, Bryant ML, Lewis RE. Immune system-neuroendocrine dysregulation in spinal cord injury. Immunol Res. 1996;15:306–14.
Campagnolo DI, Bartlett JA, Keller SE. Influence of neurological level on immune function following spinal cord injury: a review. J Spinal Cord Med. 2000;23:121–8. https://doi.org/10.1080/10790268.2000.11753519
Moalem G, Tracey DJ. Immune and inflammatory mechanisms in neuropathic pain. Brain Res Rev. 2006;51:240–64. https://doi.org/10.1016/J.BRAINRESREV.2005.11.004
Herieka M, Erridge C. High-fat meal induced postprandial inflammation. Mol Nutr Food Res. 2014;58:136–46. https://doi.org/10.1002/mnfr.201300104
Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013;71:511–27. https://doi.org/10.1111/nure.12035
Allison DJ, Thomas A, Beaudry K, Ditor DS. Targeting inflammation as a treatment modality for neuropathic pain in spinal cord injury: a randomized clinical trial. J Neuroinflamm. 2016;13:152. https://doi.org/10.1186/s12974-016-0625-4
Martin Ginis KA, van der Scheer JW, Todd KR, Davis JC, Gaudet S, Hoekstra F, et al. A pragmatic randomized controlled trial testing the effects of the international scientific SCI exercise guidelines on SCI chronic pain: protocol for the EPIC-SCI trial. Spinal Cord. 2020;58:746–54. https://doi.org/10.1038/s41393-020-0478-7
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21. https://doi.org/10.1038/s41393-017-0017-3
Ghanim H, Abuaysheh S, Sia CL, Korzeniewski K, Chaudhuri A, Fernandez-Real JM, et al. Increase in plasma endotoxin concentrations and the expression of toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: implications for insulin resistance. Diabetes Care. 2009;32:2281–7. https://doi.org/10.2337/dc09-0979
Walters JL, Buchholz AC, Martin Ginis KA. Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord. 2009;47:318–22. https://doi.org/10.1038/sc.2008.134
Farkas GJ, Pitot MA, Berg AS, Gater DR. Nutritional status in chronic spinal cord injury: a systematic review and meta-analysis. Spinal Cord. 2019;57:3–17. https://doi.org/10.1038/s41393-018-0218-4
Fuller KNZ, Summers CM, Valentine RJ. Effect of a single bout of aerobic exercise on high-fat meal-induced inflammation. Metabolism. 2017;71:144–52. https://doi.org/10.1016/j.metabol.2017.03.001
Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4. https://doi.org/10.3389/fpsyg.2013.00863.
Oostrom AJHHMvan, Rabelink TJ, Verseyden C, Sijmonsma TP, Plokker HWM, De Jaegere PPTh, et al. Activation of leukocytes by postprandial lipemia in healthy volunteers. Atherosclerosis. 2004;177:175–82. https://doi.org/10.1016/j.atherosclerosis.2004.07.004
Hansen K, Sickelmann F, Pietrowsky R, Fehm HL, Born J. Systemic immune changes following meal intake in humans. Am J Physiol. 1997;273:R548–53. https://doi.org/10.1152/ajpregu.1997.273.2.R548
Erridge C, Attina T, Spickett CM, Webb DJ. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr. 2007;86:1286–92. https://doi.org/10.1093/ajcn/86.5.1286
Sennels HP, Jørgensen HL, Hansen A-LS, Goetze JP, Fahrenkrug J. Diurnal variation of hematology parameters in healthy young males: the Bispebjerg study of diurnal variations. Scand J Clin Lab Investig. 2011;71:532–41. https://doi.org/10.3109/00365513.2011.602422
Plumelle D, Lombard E, Nicolay A, Portugal H. Influence of diet and sample collection time on 77 laboratory tests on healthy adults. Clin Biochem. 2014;47:31–7. https://doi.org/10.1016/j.clinbiochem.2013.11.002
Fatima G, Sharma VP, Verma NS. Circadian variations in melatonin and cortisol in patients with cervical spinal cord injury. Spinal Cord. 2016;54:364–7. https://doi.org/10.1038/sc.2015.176
Kostovski E, Frigato E, Savikj M, Dahm AEA, Sandset PM, Mowinckel M-C, et al. Normalization of disrupted clock gene expression in males with tetraplegia: a crossover randomized placebo-controlled trial of melatonin supplementation. 2018. https://doi.org/10.1038/s41393-018-0176-x.
Cruse JM, Lewis RE, Dilioglou S, Roe DL, Wallace WF, Chen RS. Review of immune function, healing of pressure ulcers, and nutritional status in patients with spinal cord injury. J Spinal Cord Med. 2000;23:129–35. https://doi.org/10.1080/10790268.2000.11753520
Koszinowski UH, Reddehase MJ, Jonjic S. The role of CD4 and CD8 T cells in viral infections. Curr Opin Immunol. 1991;3:471–5. https://doi.org/10.1016/0952-7915(91)90005-L
Bancroft GJ. The role of natural killer cells in innate resistance to infection. Curr Opin Immunol. 1993;5:503–10. https://doi.org/10.1016/0952-7915(93)90030-V
Berg-Emons RJvanden, Bussmann JB, Stam HJ. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil. 2010;91:1856–61. https://doi.org/10.1016/j.apmr.2010.08.018
Nash MS, Groah SL, Gater DR, Dyson-Hudson TA, Lieberman JA, Myers J, et al. Identification and management of cardiometabolic risk after spinal cord injury: clinical practice guideline for health care providers. Top Spinal Cord Inj Rehabil. 2018;24:379–423. https://doi.org/10.1310/sci2404-379
Chan W-M, Mohammed Y, Lee I, Pearse DD. Effect of gender on recovery after spinal cord injury. Transl Stroke Res. 2013;4:447–61. https://doi.org/10.1007/s12975-012-0249-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dix, G.U., Jackson, G.S., Todd, K.R. et al. The effects of a high-fat/high-carbohydrate meal on leukocyte populations in adults with chronic spinal cord injury. Spinal Cord Ser Cases 7, 49 (2021). https://doi.org/10.1038/s41394-021-00412-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00412-7