Abstract
Some cytogenetic abnormalities (CAs) are associated with poorer prognosis in multiple myeloma (MM); proteasome inhibitors appear to benefit patients with high-risk CAs. We evaluated 2247 MM patients from the TOURMALINE-MM1/-MM2/-MM3/-MM4 trials to assess the PFS benefit of ixazomib plus lenalidomide-dexamethasone (Rd) vs placebo-Rd (TOURMALINE-MM1/-MM2) or ixazomib vs placebo (TOURMALINE-MM3/-MM4) in specific high-risk CAs. After a pooled median follow-up of 25.6 months, the hazard ratio (HR) for PFS with ixazomib- vs placebo-based therapy for high-risk patients was 0.74 (95% confidence interval [CI]: 0.59–0.93; median PFS [mPFS] 17.8 vs 13.2 months), and 0.70 (95% CI: 0.62–0.80; mPFS 26.3 vs 17.6 months) for complementary standard-risk patients. The HR for expanded high-risk patients was 0.75 (95% CI: 0.64–0.87; mPFS 18.1 vs 14.1 months), and 0.71 (95% CI: 0.59–0.85; mPFS 36.1 vs 21.4 months) for complementary standard-risk patients. The HR for PFS with ixazomib- vs placebo-based therapy was 0.68 in patients with t(4;14) (95% CI: 0.48–0.96; mPFS 22.4 vs 13.2 months), and 0.77 for patients with amp1q21 (95% CI: 0.63–0.93; mPFS 18.8 vs 14.5 months). A PFS benefit was demonstrated with ixazomib- vs placebo-based therapy regardless of cytogenetic status, with greatest benefit observed in patients with t(4;14) and amp1q21.
Similar content being viewed by others
Introduction
Therapeutic strategies for multiple myeloma (MM) have greatly advanced in the last two decades following the introduction of novel agents such as immunomodulatory imide drugs, anti-CD38 antibodies and proteasome inhibitors (PIs) [1,2,3]. PIs have become a cornerstone of MM therapy [4], and their use in a continuous fashion or to achieve higher cumulative doses leads to improved long-term outcomes compared with fixed-duration therapy [5,6,7]. However, despite these improvements, outcomes of patients with MM vary based on a number of prognostic factors, including cytogenetic risk [8]. Indeed, the survival of patients with certain cytogenetic abnormalities has generally remained poor compared with patients with standard-risk cytogenetic abnormalities [3, 9,10,11]. Cytogenetic abnormalities associated with poorer prognosis in MM include deletion of chromosome 17p [del(17p)], translocation between chromosomes 4 and 14 [t(4;14)], translocation between chromosomes 14 and 16 [t(14;16)], and amplification of 1q21 (amp1q21) [3], and, aside from amp1q21, are included in the 2016 International Myeloma Working Group (IMWG) definition of high-risk cytogenetics [12].
There is a general consensus among clinicians that treatment with PIs benefit patients carrying these cytogenetic abnormalities [12]. This has been demonstrated for the oral PI ixazomib- vs placebo-based therapy in a number of phase 3 studies [13,14,15,16,17]. In TOURMALINE-MM1, relapsed, refractory, or relapsed and refractory multiple myeloma (RRMM) patients with high-risk cytogenetic abnormalities treated with ixazomib plus lenalidomide-dexamethasone (IRd) had similar progression-free survival (PFS) to those with standard-risk cytogenetics vs patients who received placebo-Rd [13], suggesting that addition of ixazomib to Rd may have abrogated the increased risk conferred by cytogenetic abnormalities [13]. Additionally, patients with high-risk and expanded high-risk cytogenetics treated with IRd demonstrated a treatment benefit vs placebo-Rd (overall survival [OS] hazard ratio [HR] < 1) in the final OS analysis of TOURMALINE-MM1 [14]. Similarly, TOURMALINE-MM2 showed that patients with newly diagnosed multiple myeloma (NDMM) with expanded high-risk cytogenetics treated with IRd had improved PFS compared with placebo-Rd [15]. In the maintenance setting, patients with high-risk cytogenetics who received ixazomib maintenance following autologous stem cell transplant (ASCT) in TOURMALINE-MM3 had improved PFS vs placebo [16], and in TOURMALINE-MM4, transplant-ineligible patients with expanded high-risk cytogenetics who received ixazomib as post-induction maintenance demonstrated a PFS benefit vs placebo [17].
Although identification of certain cytogenetic abnormalities has guided stratification of high-risk patients and helped to characterize prognosis, not all patients with high-risk cytogenetic abnormalities exhibit the same response to therapy, and the efficacy of available treatment options varies according to the presence of particular cytogenetic abnormalities [12]. Accordingly, treatment decisions should be based on individual cytogenetic data [18]. At present, clinical trials assessing response to MM therapy according to specific cytogenetic abnormalities are limited [19], and the IMWG has stated that the analysis of cytogenetic subgroups in trials comparing different treatments is an important goal [12]. We therefore conducted this analysis of four TOURMALINE studies (TOURMALINE- MM1, -MM2, -MM3 and -MM4) [13, 15,16,17] to evaluate the association between PFS and individual cytogenetic risk and to assess whether certain patients benefit more with ixazomib-based therapy, thus contributing to the evolution of precision medicine within MM.
Methods
Patients and study designs
This pooled analysis included data from four randomized, placebo-controlled phase 3 trials and two treatment interventions. The full methods for these trials have been published previously [13, 15,16,17]. In TOURMALINE-MM1 (NCT01564537), -MM2 (NCT01850524), -MM3 (NCT02181413), and -MM4 (NCT02312258), respectively, adult patients were enrolled in 147, 157, 167, and 187 sites across 26, 8, 30, and 34 countries.
Patients with RRMM (N = 722) were enrolled into TOURMALINE-MM1, and eligible patients in TOURMALINE-MM2 (N = 705) had a confirmed diagnosis of symptomatic MM according to IMWG criteria and were eligible for treatment with Rd but ineligible for ASCT. The study designs of TOURMALINE-MM1 and -MM2 were similar; patients were randomized 1:1 to receive oral ixazomib 4 mg or matching placebo on days 1, 8 and 15 of 28-day cycles. In addition, all patients received oral lenalidomide 25 mg on days 1–21 (10 mg for patients with creatine clearance ≤60 or ≤50 mL/minute, depending on local prescribing information) and oral dexamethasone 40 mg on days 1, 8, 15 and 22 [13, 15].
In TOURMALINE-MM3 and -MM4, 656 and 706 patients, respectively, with a confirmed diagnosis of symptomatic MM according to IMWG criteria were enrolled. In TOURMALINE-MM3, eligible patients had achieved ≥partial response (PR) after undergoing standard induction therapy followed by high-dose melphalan conditioning and single ASCT within 12 months of diagnosis. Eligible patients in TOURMALINE-MM4 were transplant-ineligible or unwilling to receive ASCT and had achieved ≥PR after 6–12 months of standard induction therapy. The TOURMALINE-MM3 and -MM4 studies were similarly designed; patients were randomized 3:2 to receive maintenance therapy with single-agent oral ixazomib 3 mg or matching placebo on days 1, 8 and 15 of 28-day cycles [16, 17].
The primary endpoint for all four studies was PFS, defined as the time from the date of randomization to the date of first documentation of disease progression or death from any cause, as assessed by an independent review committee. A key prespecified secondary endpoint in all four studies was PFS in high-risk cytogenetic patient groups characterized by specific cytogenetic abnormalities [13, 15,16,17].
The trials were conducted in accordance with the International Conference on Harmonization Guidelines for Good Clinical Practice and appropriate regulatory requirements. Local ethics committees or institutional review boards approved the protocols. All patients provided written informed consent.
Pooled analysis patients
In this pooled analysis, evaluable patients were categorized into subgroups according to the presence of one or more cytogenetic abnormalities. Patients with del(17p) and/or t(4;14) and/or t(14;16) cytogenetic abnormalities were categorized as ‘high-risk’, and patients with ≥1 high-risk abnormality and/or amp1q21 were categorized as ‘expanded high-risk’. Complementary standard-risk cytogenetic subgroups were defined as the absence of these high-risk or expanded high-risk abnormalities in samples available for testing. If cytogenetic abnormalities were unknown, indeterminate, or missing, the patient was deemed as unclassifiable [13, 15,16,17].
Cytogenetic assessments
In TOURMALINE-MM1 and -MM2, cytogenetic abnormalities were assessed by a central laboratory at screening (within 8 weeks of randomization in TOURMALINE-MM2) using fluorescence in situ hybridization (FISH) in enriched CD138+ plasma cells from bone marrow aspirates. The presence of del(17p), t(4;14), and t(14;16) were defined based on cut-offs of 5%, 3%, and 3% positive cells, respectively, based on the false-positive rates (or technical cut-offs) of the FISH probes used. Cut-off values of 3% (TOURMALINE-MM1) and 20% (TOURMALINE-MM2) were used for amp1q21, and ≥3 copies were considered positive for 1q21 (TOURMALINE-MM1 and -MM2) [13,14,15].
In TOURMALINE-MM3 and -MM4, cytogenetic assessments were performed locally using FISH or conventional karyotyping with locally defined thresholds for positivity. Result reports were interpreted centrally by a board-certified hematopathologist. In selected regions where cytogenetic evaluation at the time of diagnosis was not routinely conducted, pre-screening cytogenetic evaluation was performed where possible [16, 17]. Cytogenetic characteristics were documented at the time of disease diagnosis and were not reassessed during the course of the study (TOURMALINE-MM3) [16].
Statistical analysis
Pooled data on progression events and deaths were used to generate Kaplan–Meier estimates for PFS for ixazomib- vs placebo-based therapy in the defined cytogenetic patient subgroups and for patients with ≥1 of the four individual cytogenetic abnormalities. Statistical comparisons of PFS in ixazomib- vs placebo-based therapy pooled treatment groups were based on unstratified HRs and descriptive log-rank p values [13, 15,16,17].
To control for potential confounding factors arising from differences between study designs and patient populations, a sensitivity analysis stratified by study was conducted by aggregating stratified HR from individual studies (weighted method to calculate overall HR). The pooled adjusted HR was derived from adjusting the determination of the overall HR applying the studies as covariate. The pooled weighted HR utilized the derived weights for each study, aggregated over the studies to obtain the pooled HR.
Results
Patients
Overall, 2247 patients in the pooled analysis population were evaluable for the presence or absence of del(17p), t(4;14), and t(14;16) cytogenetic abnormalities, of whom 497 (22%) were classified as high risk and 1750 (78%) were classified as standard risk (Table 1). Of these, 270 of 497 (54%) patients and 958 of 1750 (55%) patients received ixazomib-based therapy in the high-risk and complementary standard-risk subgroups, respectively (Table 1). Expanded high-risk cytogenetics (high-risk cytogenetic abnormalities and/or amp1q21) were evaluable in a total of 2098 patients (Table 1). Of these, 555 of 1143 (49%) patients receiving ixazomib-based therapy and 479 of 955 (50%) patients receiving placebo-based therapy had ≥1 high-risk cytogenetic abnormality and/or amp1q21, and were classified as expanded high risk (Table 1). Correspondingly, 588 (51%) and 476 (50%) of patients receiving ixazomib- and placebo-based therapy, respectively, were classified as standard risk (Table 1).
PFS analysis by cytogenetic risk subgroups
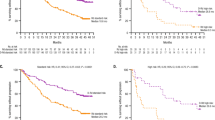
Median follow-up in the pooled analysis was 25.6 months (12.7, 54.6, 29.7, and 21.3 months, in TOURMALINE-MM1, TOURMALINE-MM2, TOURMALINE-MM3, and TOURMALINE-MM4, respectively). The HR for PFS with ixazomib- vs placebo-based therapy was 0.74 (95% confidence interval [CI]: 0.59–0.93; p = 0.0086) for patients in the high-risk subgroup, and the median PFS was 17.8 vs 13.2 months (Figs. 1 and 2A). For patients in the high-risk complementary standard-risk subgroup, the HR for PFS with ixazomib- vs placebo-based therapy was 0.70 (95% CI: 0.62–0.80; p = 0.0001; median PFS 26.3 vs 17.6 months) (Figs. 1 and 2B).
High-risk subgroup: presence of one or more of del(17p), t(4;14) or t(14;16) cytogenetic abnormalities; expanded high-risk subgroup: presence of any of the above and/or amp1q21; complementary standard-risk subgroups: patients without any of the specified cytogenetic abnormalities listed above for high-risk and expanded high-risk. *Data for t(14;16) are not shown due to small patient numbers. †Descriptive p values; analyses not powered for statistical testing. ‡1 patient was not included in the analysis due to inadequate sampling for cytogenetic assessment. CI confidence interval, HR hazard ratio, PFS progression-free survival.
The HR for PFS with ixazomib- vs placebo-based therapy in the expanded high-risk subgroup was 0.75 (95% CI: 0.64–0.87; p = 0.0002). The median PFS was 18.1 months for patients receiving ixazomib-based therapy compared with 14.1 months for patients receiving the placebo-based regimen (Figs. 1 and 3A). For patients in the expanded high-risk complementary standard-risk subgroup, the HR for PFS with ixazomib- vs placebo-based therapy was 0.71 (95% CI: 0.59–0.85; p = 0.0002; median PFS 36.1 vs 21.4 months) (Figs. 1 and 3B).
When cytogenetic risk status was compared in patients receiving ixazomib-based therapy, median PFS for patients in the high-risk subgroup was 17.8 months, vs 26.3 months in the standard-risk subgroup (complement of high-risk) (HR: 0.65; 95% CI: 0.54–0.78; Supplementary Fig. 1A). For patients in the expanded high-risk subgroup, median PFS was 18.1 months, vs 36.1 months in the standard-risk subgroup (complement of expanded high-risk) (HR: 0.54; 95% CI: 0.46–0.64; Supplementary Fig. 1B).
PFS analysis according to the presence of individual cytogenetic abnormalities
In patients with t(4;14), the HR for PFS with ixazomib- vs placebo-based therapy was 0.68 (95% CI: 0.48–0.96; p = 0.0268; median 22.4 vs 13.2 months) (Figs. 1 and 4A). For patients with amp1q21, the HR for PFS with ixazomib- vs placebo-based therapy was 0.77 (95% CI: 0.63–0.93; p = 0.0071; median 18.8 vs 14.5 months) (Figs. 1 and 4B). For patients with del(17p), the HR for PFS with ixazomib- vs placebo-based therapy was 0.80 (95% CI: 0.59–1.09; p = 0.1651; median 15.7 vs 13.2 months) (Figs. 1 and 4C). To assess the impact of del(17p) on outcomes independent of treatment, we analyzed PFS according to the presence of del(17p) vs standard-risk cytogenetics in patients who received placebo-based therapy (Supplementary Fig. 2). The HR for PFS for patients with del(17p) vs standard-risk cytogenetics was 0.69 (95% CI: 0.54–0.88; p = 0.0023; median 17.6 vs 13.2 months). For the analysis in patients with t(14;16) there were only 11 events in 16 patients receiving ixazomib-based therapy and 14 events in 23 patients receiving placebo-based therapy; the median PFS was 11.4 and 15.9 months, respectively (HR 1.21; 95% CI: 0.55–2.69; p = 0.634) (Supplementary Fig. 3).
Sensitivity analysis of PFS stratified by study
A sensitivity analysis of PFS was performed; the HRs with ixazomib- vs placebo-based therapy were 0.71 (95% CI: 0.57–0.89; p = 0.0033) for patients with high-risk cytogenetic abnormalities and 0.68 (95% CI: 0.59–0.77; p = 0.0001) for patients in the complementary standard-risk subgroups. Similarly, the HRs for PFS with ixazomib- vs placebo-based therapy were 0.70 (95% CI: 0.60–0.82; p = 0.0001) for patients in the expanded high-risk subgroup, and 0.67 (95% CI: 0.55–0.80; p = 0.0001) for patients in the respective standard-risk subgroup (Fig. 5). In patients with del(17p), t(4;14), and amp1q21, the HRs for PFS with ixazomib- vs placebo-based therapy were 0.75, 0.67, and 0.72 (Fig. 5).
Sensitivity analysis conducted by aggregating stratified HR from the individual studies (weighted method to calculate overall HR), to accommodate for potential confounding factors arising from the differing study designs. Patients who were alive or who had not progressed at the data cut-off were censored on the day of last contact. High-risk subgroup: presence of one or more of del(17p), t(4;14) or t(14;16) cytogenetic abnormalities; expanded high-risk subgroup: presence of any of the above and/or amp1q21; complementary standard-risk subgroups: patients without any of the specified cytogenetic abnormalities listed above for high-risk and expanded high-risk. *1 patient was not included in the analysis due to inadequate sampling for cytogenetic assessment. CI confidence interval, HR hazard ratio, PFS progression-free survival.
PFS analysis by combination (non-maintenance) vs single-agent (maintenance) therapy
Analyses of PFS to investigate whether ixazomib in combination with Rd (TOURMALINE-MM1 and TOURMALINE-MM2) improves outcomes for patients with high-risk cytogenetic abnormalities vs single-agent ixazomib (TOURMALINE-MM3 and TOURMALINE-MM4) are shown in Fig. 6.
In patients with high-risk cytogenetic abnormalities, the HR for PFS with ixazomib- vs placebo-based therapy in TOURMALINE-MM1 and TOURMALINE-MM2 (combination non-maintenance) was 0.64 (95% CI: 0.46–0.89; p = 0.007). In TOURMALINE-MM3 and TOURMALINE-MM4 (single-agent maintenance), the HR for PFS with ixazomib- vs placebo-based therapy was 0.83 (95% CI: 0.61–1.13; p = 0.2456) (Fig. 6A). The median PFS for patients receiving ixazomib as combination vs single-agent therapy was 21.4 vs 14.8 months. For patients receiving the placebo regimens, the median PFS was 12.9 vs 13.2 months for combination vs single-agent therapy (Fig. 6A).
For patients in the standard-risk subgroup, the HR for PFS with ixazomib- vs placebo-based in TOURMALINE-MM1 and TOURMALINE-MM2 (combination non-maintenance) was 0.74 (95% CI: 0.6–0.9; p = 0.0029); in TOURMALINE-MM3 and TOURMALINE-MM4 (single-agent maintenance) the HR for PFS with ixazomib- vs placebo-based therapy was 0.62 (95% CI: 0.52–0.74; p < 0.0001) (Fig. 6B). In the ixazomib treatment cohorts, the median PFS for patients was 35.3 vs 24.1 months for combination vs single-agent therapy, and for patients receiving the corresponding placebo regimen, median PFS was 19.4 vs 14.7 months, respectively (Fig. 6B).
Discussion
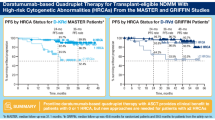
This pooled analysis of four TOURMALINE phase 3 studies demonstrated a PFS benefit with ixazomib- vs placebo-based therapy regardless of the presence of specific adverse cytogenetic abnormalities in patients with MM. Ixazomib-based therapy prolonged median PFS by 4.6 and 4.0 months compared with placebo-based therapy for patients with high-risk and expanded high-risk cytogenetic abnormalities, respectively. Furthermore, a similar magnitude of benefit was found for ixazomib- vs placebo-based therapy for patients with high-risk (HR 0.74) and expanded high-risk (HR 0.75) cytogenetic abnormalities compared to the respective complementary standard-risk subgroups (HRs 0.70 and 0.71). Importantly, in subgroup analyses of specific cytogenetic abnormalities, a greater PFS benefit with ixazomib- vs placebo-based therapy was demonstrated for patients carrying t(4;14) and amp1q21 cytogenetic abnormalities. Overall, ixazomib combined with Rd or as a single-agent maintenance therapy did not abrogate the negative impact of high-risk cytogenetic abnormalities, consistent with previously reported findings with ixazomib in non-transplant NDMM patients (TOURMALINE-MM2 [15]), the maintenance setting (TOURMALINE-MM3 [16] and TOURMALINE-MM4 [17]), and smaller real-world studies [20, 21]. Additionally, in a recent study in NDMM patients, no significant improvement of PFS or OS was demonstrated with IRd maintenance vs Rd in patients with standard- or high-risk cytogenetics [22].
However, in TOURMALINE-MM1, median PFS data suggested that ixazomib in combination with Rd may improve prognosis for RRMM patients with high-risk cytogenetics by lengthening PFS to that similar to patients with standard-risk cytogenetics [13, 23]. Furthermore, greater OS benefit was observed in patients with high-risk and expanded high-risk cytogenetics treated with ixazomib [14]. The pooled analysis presented here included two studies of single-agent ixazomib (TOURMALINE-MM3 and TOURMALINE-MM4) and two studies where patients received IRd (TOURMALINE-MM1 and TOURMALINE-MM2). Thus, the triple-drug regimen may have influenced the ability of ixazomib to abrogate the negative impact of high-risk cytogenetics in this specific treatment setting, as suggested by the IMWG [12], but not all patients were exposed to the triple-drug regimen in the TOURMALINE program. We therefore conducted an analysis to assess the impact of single-agent ixazomib vs combination therapy, in both the high-risk and complementary standard-risk cohorts. Our findings show that in patients with high-risk cytogenetics abnormalities, there was a PFS benefit with ixazomib vs placebo in combination with Rd (HR 0.64) and the HR was lower than with single-agent ixazomib vs placebo (HR 0.83). In contrast, in patients with standard-risk cytogenetic abnormalities, a PFS benefit was observed with both combination and single-agent ixazomib, but the HR for PFS with IRd vs placebo-Rd (HR 0.74) was higher than the HR for single-agent ixazomib vs placebo (HR 0.62). These results support the findings from TOURMALINE-MM1 that ixazomib in combination with Rd is efficacious in patients with high-risk cytogenetic abnormalities and may improve the prognosis of these patients [13, 23].
Further analyses in the high-risk and expanded high-risk subgroups, according to specific cytogenetic abnormalities, demonstrated a PFS benefit with ixazomib- vs placebo-based therapy in patients with t(4;14) (HR 0.68), amp1q21 (HR 0.77), and del(17p) (HR 0.80). Ixazomib- vs placebo-based therapy increased median PFS for patients with t(4;14) and amp1q21 by 9.2 and 4.3 months, respectively. Ixazomib-based therapy prolonged median PFS by 2.5 months for patients with del(17p). The greater magnitude of PFS benefit seen for patients carrying t(4;14) and amp1q21 suggests that improved outcomes in the expanded high-risk subgroups were primarily driven by PFS differences in patients with these more frequent cytogenetic abnormalities. The number of patients in the t(14;16) subgroup were small and conclusions based on the relative contribution of this cytogenetic abnormality on PFS cannot be drawn.
This analysis supports the hypothesis that PI-based therapy is clinically relevant in the management of patients with MM who have high-risk cytogenetic abnormalities [12], and broadens the range of populations and treatment settings over which this benefit may apply. Other PI agents, including carfilzomib and bortezomib, have previously indicated a benefit in patients with high-risk cytogenetic abnormalities [24, 25], although outcomes with carfilzomib-Rd were still poorer than for patients with standard-risk cytogenetics [24], and other studies of short-course bortezomib-based therapy have reported limited benefit [26, 27]. This suggests prolonged PI-based therapy is important in this treatment setting. In the context of long-term therapy, carfilzomib and bortezomib are parenterally administered PIs [28, 29] vs the oral administration of ixazomib [30, 31]. Oral administration conveniently allows for less frequent hospital or clinic visits during continuous/prolonged PI treatment. Additionally, carfilzomib is associated with cardiac and renal complications, while peripheral neuropathy is a treatment emergent adverse event of clinical importance with bortezomib [32, 33]. The safety profile of ixazomib is well established [13, 15,16,17], and ixazomib-based therapy is feasible in patients with high-risk cytogenetics based on tolerability data from previous studies [13,14,15,16,17, 23].
The limitations of this pooled analysis include differences in eligibility criteria, patient populations, and length of follow-up among the four studies, as well as higher patient numbers in the standard-risk vs high-risk subgroups. Additionally, the copy number for chromosome 1 abnormalities evaluated in this analysis was not specified. A recent publication focusing on the lack of uniformity of categorizing patients with additional copies of 1q as high-risk highlights the importance of copy number of 1q as a driver of poor outcomes in MM [34]. As such, further study that includes the patients’ copy number of 1q is needed in order to determine the impact of this abnormality on treatment outcomes. Furthermore, data on measurable residual disease (MRD) were not collected for all four studies, thus an analysis of the relationship between MRD and cytogenetics cannot be conducted; however, a recent publication by Paiva et al. evaluates the implications of MRD in the TOURMALINE-MM3 and TOURMALINE-MM4 study populations [35]. Another limitation is the use of inconsistent cut-off values for defining the presence of high-risk cytogenetic abnormalities across the four studies in this analysis, limiting cross-trial comparisons. At present, there is no standardized FISH-positivity cut-off value for defining the presence of del(17p) [12, 23]. It is currently unclear what minimum percentage of del(17p)-positive cells is associated with a poor prognosis, or whether this varies depending on treatment used and stage of disease [12]. Previous MM studies involving cytogenetic assessments have used a range of different cut-off values for FISH testing, with some publications suggesting that a cut-off of >55% positive cells del(17p) is required to be deemed high risk [24, 36,37,38,39]. In TOURMALINE-MM1 and TOURMALINE-MM2, a cut-off of 5% positive cells was used for del(17p), and in TOURMALINE-MM3 and TOURMALINE-MM4 thresholds for positivity were defined locally. Given the differences in assessing del(17p) between the studies and that in our analyses we did not stipulate a cut-off for del(17p) to be considered high-risk compared with previous publications, we analyzed PFS in patients who received placebo-based therapy according to whether they were del(17p) positive vs standard-risk cytogenetics. The findings from this analysis suggest that the population of patients defined as del(17p) positive were high-risk as they had significantly lower PFS compared to those assessed as standard-risk. However, these results are based on pooled data with different levels of del(17p) positive cells present within individual patients, and the impact of this variability on these outcomes is unknown. Nonetheless, despite these limitations and the more conservative approach taken towards defining del(17p) positive patients, there was an overall trend in favor of ixazomib- vs placebo-based therapy.
In conclusion, ixazomib- vs placebo-based therapy demonstrated a PFS benefit in patients with MM regardless of the presence of specific adverse cytogenetic abnormalities. Ixazomib- vs placebo-based therapy displayed a similar magnitude of PFS benefit in patients with high-risk and expanded high-risk cytogenetic abnormalities compared to the respective complementary standard-risk subgroups. Our results suggest that ixazomib- vs placebo-based therapy may provide a greater PFS benefit for patients carrying t(4;14) and amp1q21. Additionally, we demonstrate a PFS benefit for ixazomib in combination with Rd vs single-agent ixazomib in patients with high-risk MM. In line with previously reported findings, ixazomib combined with Rd or as single-agent maintenance therapy did not abrogate the negative impact of high-risk cytogenetic abnormalities. However, differences in eligibility criteria and patient populations across the four studies may have contributed to difficulties interpreting the data. Overall, the findings from this pooled analysis indicate that ixazomib-based therapy may be a viable treatment option for patients with MM who have high-risk and expanded high-risk cytogenetic abnormalities.
Data availability
The datasets, including the redacted study protocol, redacted statistical analysis plan, and individual participants’ data supporting the results reported in this article, will be made available within 3 months from initial request to researchers who provide a methodologically sound proposal. The data will be provided after its de-identification, in compliance with applicable privacy laws, data protection, and requirements for consent and anonymization.
References
Ito S. Proteasome inhibitors for the treatment of multiple myeloma. Cancers. 2020;12:1–19.
Du J, Zhuang J. Major advances in the treatment of multiple myeloma in American Society of Hematology annual meeting 2020. Chronic Dis Transl Med. 2021;7:220–6.
Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am J Hematol. 2020;95:548–67.
Kumar SK, Callander NS, Adekola K, Anderson L, Baljevic M, Campagnaro E, et al. Multiple Myeloma, Version 3.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:1685–717.
Jimenez-Zepeda VH, Duggan P, Neri P, Tay J, Bahlis NJ. Bortezomib-containing regimens (BCR) for the treatment of non-transplant eligible multiple myeloma. Ann Hematol. 2017;96:431–9.
Mateos MV, Richardson PG, Dimopoulos MA, Palumbo A, Anderson KC, Shi H, et al. Effect of cumulative bortezomib dose on survival in multiple myeloma patients receiving bortezomib-melphalan-prednisone in the phase III VISTA study. Am J Hematol. 2015;90:314–9.
Palumbo A, Gay F, Cavallo F, Di Raimondo F, Larocca A, Hardan I, et al. Continuous therapy versus fixed duration of therapy in patients with newly diagnosed multiple myeloma. J Clin Oncol. 2015;33:3459–66.
Wallington-Beddoe CT, Mynott RL. Prognostic and predictive biomarker developments in multiple myeloma. J Hematol Oncol. 2021;14:151.
Jurczyszyn A, Charliński G, Suska A, Vesole DH. The importance of cytogenetic and molecular aberrations in multiple myeloma. Acta Haematol Pol. 2021;52:361–70.
Goldschmidt H, Lokhorst HM, Mai EK, van der Holt B, Blau IW, Zweegman S, et al. Bortezomib before and after high-dose therapy in myeloma: long-term results from the phase III HOVON-65/GMMG-HD4 trial. Leukemia. 2018;32:383–90.
D’Agostino M, Ruggeri M, Aquino S, Giuliani N, Arigoni M, Gentile M, et al. Impact of gain and amplification of 1q in newly diagnosed multiple myeloma patients receiving carfilzomib-based treatment in the Forte Trial. Blood. 2020;136:38–40.
Sonneveld P, Avet-Loiseau H, Lonial S, Usmani S, Siegel D, Anderson KC, et al. Treatment of multiple myeloma with high-risk cytogenetics: a consensus of the International Myeloma Working Group. Blood. 2016;127:2955–62.
Moreau P, Masszi T, Grzasko N, Bahlis NJ, Hansson M, Pour L, et al. Oral ixazomib, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;374:1621–34.
Richardson PG, Kumar SK, Masszi T, Grzasko N, Bahlis NJ, Hansson M, et al. Final overall survival analysis of the TOURMALINE-MM1 phase III trial of ixazomib, lenalidomide, and dexamethasone in patients with relapsed or refractory multiple myeloma. J Clin Oncol. 2021;39:2430–42.
Facon T, Venner CP, Bahlis NJ, Offner F, White DJ, Karlin L, et al. Oral ixazomib, lenalidomide, and dexamethasone for transplant-ineligible patients with newly diagnosed multiple myeloma. Blood. 2021;137:3616–28.
Dimopoulos MA, Gay F, Schjesvold F, Beksac M, Hajek R, Weisel KC, et al. Oral ixazomib maintenance following autologous stem cell transplantation (TOURMALINE-MM3): a double-blind, randomised, placebo-controlled phase 3 trial. Lancet. 2019;393:253–64.
Dimopoulos MA, Spicka I, Quach H, Oriol A, Hajek R, Garg M, et al. Ixazomib as postinduction maintenance for patients with newly diagnosed multiple myeloma not undergoing autologous stem cell transplantation: the phase III TOURMALINE-MM4 trial. J Clin Oncol. 2020;38:4030–41.
Goldman-Mazur S, Vesole DH, Jurczyszyn A. Clinical implications of cytogenetic and molecular aberrations in multiple myeloma. Acta Haematol Pol. 2021;52:18–28.
Abdallah N, Rajkumar SV, Greipp P, Kapoor P, Gertz MA, Dispenzieri A, et al. Cytogenetic abnormalities in multiple myeloma: association with disease characteristics and treatment response. Blood Cancer J. 2020;10:82.
Li J, Bao L, Xia Z, Wang S, Zhou X, Ding K, et al. Ixazomib-based frontline therapy in patients with newly diagnosed multiple myeloma in real-life practice showed comparable efficacy and safety profile with those reported in clinical trial: a multi-center study. Ann Hematol. 2020;99:2589–98.
Cohen YC, Magen H, Lavi N, Gatt ME, Chubar E, Horowitz N, et al. Ixazomib-based regimens for relapsed/refractory multiple myeloma: are real-world data compatible with clinical trial outcomes? A multi-site Israeli registry study. Ann Hematol. 2020;99:1273–81.
Rosinol L, Oriol A, Ríos Tamayo R, Blanchard MJ, Jarque I, Bargay J, et al. Ixazomib plus lenalidomide/dexamethasone (IRd) versus lenalidomide/dexamethasone (Rd) maintenance after autologous stem cell transplant in patients with newly diagnosed multiple myeloma: results of the Spanish GEM2014MAIN trial. Blood 2021;138:466.
Avet-Loiseau H, Bahlis NJ, Chng WJ, Masszi T, Viterbo L, Pour L, et al. Ixazomib significantly prolongs progression-free survival in high-risk relapsed/refractory myeloma patients. Blood. 2017;130:2610–8.
Avet-Loiseau H, Fonseca R, Siegel D, Dimopoulos MA, Špička I, Masszi T, et al. Carfilzomib significantly improves the progression-free survival of high-risk patients in multiple myeloma. Blood. 2016;128:1174–80.
Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B, et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 2012;119:940–8.
Avet-Loiseau H, Leleu X, Roussel M, Moreau P, Guerin-Charbonnel C, Caillot D, et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol. 2010;28:4630–4.
Mateos MV, Oriol A, Martínez-López J, Gutiérrez N, Teruel AI, López de la Guía A, et al. Maintenance therapy with bortezomib plus thalidomide or bortezomib plus prednisone in elderly multiple myeloma patients included in the GEM2005MAS65 trial. Blood. 2012;120:2581–8.
Amgen. KYPROLIS® (carfilzomib): Highlights of Prescribing Information. 2021.
Takeda Pharmaceuticals. VELCADE® (bortezomib): Highlights of Prescribing Information. 2021.
Takeda Pharmaceutical. NINLARO® (ixazomib): Highlights of Prescribing Information. 2021.
Takeda UK. NINLARO: Summary of Product Characteristics (SmPC). 2021.
Dimopoulos MA, Roussou M, Gavriatopoulou M, Psimenou E, Ziogas D, Eleutherakis-Papaiakovou E, et al. Cardiac and renal complications of carfilzomib in patients with multiple myeloma. Blood Adv. 2017;1:449–54.
Richardson PG, Delforge M, Beksac M, Wen P, Jongen JL, Sezer O, et al. Management of treatment-emergent peripheral neuropathy in multiple myeloma. Leukemia. 2012;26:595–608.
Schmidt TM, Fonseca R, Usmani SZ. Chromosome 1q21 abnormalities in multiple myeloma. Blood Cancer J. 2021;11:83.
Paiva B, Manrique I, Dimopoulos MA, Gay F, Min C-K, Zweegman S, et al. MRD dynamics during maintenance for improved prognostication of 1280 myeloma patients in TOURMALINE-MM3 and -MM4 trials. Blood. 2022. https://doi.org/10.1182/blood.2022016782.
Corre J, Perrot A, Caillot D, Belhadj K, Hulin C, Leleu X, et al. del(17p) without TP53 mutation confers a poor prognosis in intensively treated newly diagnosed patients with multiple myeloma. Blood. 2021;137:1192–5.
Thakurta A, Ortiz M, Blecua P, Towfic F, Corre J, Serbina NV, et al. High subclonal fraction of 17p deletion is associated with poor prognosis in multiple myeloma. Blood. 2019;133:1217–21.
Chalopin T, Vallet N, Theisen O, Ochmann M, Tiab M, Godmer P, et al. No survival improvement in patients with high-risk multiple myeloma harbouring del(17p) and/or t(4;14) over the two past decades. Br J Haematol. 2021;194:635–8.
Zweegman S, van de Donk N. Deletion 17p: a matter of size and number? Blood. 2021;137:1135–6.
Acknowledgements
The authors would like to thank all patients and their families, as well as all investigators, for their valuable contributions to these studies. Victoria Enwemadu, PharmD, of Takeda Pharmaceuticals U.S.A., Inc., Lexington, MA provided editorial assistance. We would also like to acknowledge Cong Li, PhD, of Takeda Development Center Americas, Inc. (TDCA), Lexington, MA who facilitated the statistical analysis. Medical writing support for the development of this manuscript, under the direction of the authors, was provided by Beth Jamieson, BSc, and Philippa Lloyd, BSc, of Ashfield MedComms, an Inizio Company, funded by Takeda Pharmaceuticals U.S.A., Inc., Lexington, MA and complied with the Good Publication Practice (GPP) guidelines (DeTora LM, et al. Ann Intern Med 2022;175:1298–304).
Funding
These studies were funded by Millennium Pharmaceuticals, Inc., Cambridge, MA, USA, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Author information
Authors and Affiliations
Contributions
Conception and design: W-JC, SL, GJM, SKK, ABD, AV, RL, MAD, SVR. Collection and assembly of data: GJM, SI, PM, SKK, ABD, AV, KS, MAD, SVR. Data analysis and interpretation: W-JC, GJM, SI, PM, SKK, PT-A, MV, XZ, ABD, AV, KS, RL, MAD. Drafting/writing/revising the manuscript: all authors. Final approval of manuscript: all authors. Agree to be accountable for all aspects of work, which includes ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors.
Corresponding author
Ethics declarations
Competing interests
W-JC: Honoraria: Johnson and Johnson, BMS/Celgene, Amgen, Takeda, AbbVie, Sanofi, Pfizer; Research funding: Johnson and Johnson, BMS/Celgene, NMRC Singapore Translational Research (STaR) Investigator Award, National Research Foundation Singapore, Singapore Ministry of Education under the Research Centers of Excellence initiative. SL: Consultancy: Janssen, BMS, Celgene, Amgen, GSK, AbbVie, Takeda, Novartis, Genentech; Research support for trials: Janssen, BMS, Novartis; Member on board of directors and holder of stock: TG Therapeutics. GJM: Advisory council or committee: Celgene, BMS, Sanofi, Karyopharm, Janssen, GSK, Amgen, Oncopeptides, AbbVie. SI: Research funding: BMS, Ono, Takeda, Janssen, AbbVie, Chugai, Celgene, Sanofi, Pfizer, Daiichi Sankyo; Honoraria: Ono, Takeda, Janssen, BMS, Sanofi. PM: Honoraria: AbbVie, Amgen, Janssen, Sanofi, Celgene. SKK: Research funding: AbbVie, Takeda, Janssen, KITE, Merck, MedImmune/AstraZeneca, Novartis, Roche, Celgene, Adaptive, Sanofi; Advisory council or committee: KITE, Janssen, Takeda, MedImmune/AstraZeneca, AbbVie, Celgene, Adaptive. PT-A, MV, XZ: Employee: Takeda. ABD, AV, RL: Employee and holder of stock options: Takeda. KS: Employee, equity holder and divested equity in the past 24 months: Takeda. MAD: Honoraria: Amgen, BMS, Takeda, Beigene, Janssen. SVR: None.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chng, WJ., Lonial, S., Morgan, G.J. et al. A pooled analysis of outcomes according to cytogenetic abnormalities in patients receiving ixazomib- vs placebo-based therapy for multiple myeloma. Blood Cancer J. 13, 14 (2023). https://doi.org/10.1038/s41408-022-00768-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-022-00768-5