Abstract
Bardet–Biedl syndrome (BBS) is a rare autosomal recessive disorder of the cilia, often resulting in a phenotype of obesity, rod-cone dystrophy, a variable degree of intellectual disability, polydactyly, renal problems, and/or hypogonadism in males or genital abnormalities in females. We here report the case of an 11-year-old girl who presented with postaxial polydactyly, retinal dystrophy, and childhood obesity, suggesting Bardet–Biedl syndrome. She had no renal problems, developmental delay, or intellectual disability. Genetic testing revealed compound heterozygous variants in the IFT74 gene (c.371_372del p.Gln124Argfs*9 and c.16850–1G>T p.?). We here report the second patient with Bardet–Biedl syndrome due to biallelic IFT74 variants. Both patients have obesity, polydactyly, retinal dystrophy, and no renal abnormalities. The present case however, has normal intellect, whereas the other patient has intellectual disability. We hereby confirm IFT74 as a BBS gene and encourage diagnostic genetic testing laboratories to add IFT74 to their BBS gene panels.
Similar content being viewed by others
Introduction
Bardet–Biedl syndrome (BBS) is a rare autosomal recessive ciliopathy characterized by polydactyly, rod-cone dystrophy, renal abnormalities, obesity, and intellectual disability [1]. Currently, over 20 genes are associated with BBS [2]. BBS is most often caused by germline variants affecting function in BBS1 and BBS10 [1]. Some recently discovered BBS genes are members of the intraflagellar transport machinery (IFT). IFT is a bidirectional mechanism involved in the protein motility within the cilia and is important for both ciliogenesis and maintenance of the cilia [3]. There are three IFT genes associated with BBS: IFT27, IFT74, and IFT172 [2, 4]. All three genes encode for parts of the IFT-B complex which is needed in the anterograde transport of ciliary proteins, whereas the protein complex IFT-A is required for the retrograde transport [3]. Most biallelic pathogenic variants in IFT genes are associated with skeletal ciliopathies such as short-rib thoracic dysplasia (OMIM # 617102, # 611263, # 617866) and cranioectodermal dysplasia (OMIM # 218330). Two of the BBS-associated IFT genes, IFT74 and IFT172, are currently called “BBS20” in literature [4,5,6], which leads to confusion regarding which gene is in fact the BBS20-gene. We would suggest using IFT74 and IFT172 only and discard BBS20 for the sake of clarity. Biallelic pathogenic IFT74 variants are associated with BBS20 in OMIM (OMIM # 617119) and have thus far only been reported in a single case [5]. We here report the second patient, confirming IFT74 as one of the genes causing BBS when disrupted.
Subjects and methods
Case report
The proband is the second child of nonconsanguineous Dutch parents. She was born after an uncomplicated pregnancy of 41 weeks by cesarean section. Prenatal ultrasounds showed no anomalies. Birth weight was 4710 g (>2 SD for gestational age). Immediately after birth, postaxial polydactyly of the feet was noticed. There was a hemangioma at the left side of the jaw and earlobe, which later completely involuted. There were no craniofacial dysmorphisms. She had a large occipitofrontal circumference (OFC) of 40.8 cm at age one month (+3.3 SD). The additional toes were removed at age 11 months. She attained age appropriate milestones in all developmental sectors except for speech, speaking only five words at the age of 2 years but developing normal speech later in childhood. Because of her learning skills, she could skip a class in elementary school and will follow the highest level of secondary education in The Netherlands which grants access to university. Suboptimal vision was first noticed at the age of 5 years and ophthalmological examination showed macular hypopigmentation and a granular appearance. Currently, there is reduced central vision. Peripheral vision is intact. Ultrasound examination of the kidneys at age 1 year and age 8 years revealed no abnormalities of the kidneys. Age at menarche was 10 years and 11 months. No signs of genital abnormalities were noticed during physical examination and on ultrasound examination.
The proband presented at Obesity Center CGG in Rotterdam, The Netherlands at age 8 years and 10 months. She was referred for in-depth analysis of her obesity and to find a possible cause for her phenotype. Weight gain and hyperphagia started at the age of 4 years. Her eating pattern was normal and she had low-normal amounts of physical activity. At that time, height was 145.5 cm (+1.5 SD for age and sex); weight 52 kg; BMI 24.6 kg/m2 (+3 SD). She still had macrocephaly with an OFC of 58.4 cm (+3.8 SD). Indirect calorimetry revealed a 14% lower resting energy expenditure than predicted. Laboratory measurements regarding comorbidities of obesity, including standard oral glucose tolerance test, showed no signs of hepatic steatosis, and no dyslipidemia or impaired glucose tolerance. At her most recent visit at age 11 years and 2 months, her height was 162.7 cm (+1.8 SD), BMI was 26.8 kg/m2 (+2.9 SD), and OFC of 58.2 cm (+2.9 SD). Her urine albumin/creatinine ratio was normal.
Family history
There are no other family members with polydactyly or retinodystrophy, nor are there family members with other signs of BBS that are not present in the proband. The OFC of the father was +2 SD above average for age and sex, the OFC of the mother was at 0 SD.
Genetic analysis
Prior to referral to our outpatient clinic, gene panel analysis for eye diseases and ciliopathies performed in 2014 could not identify a cause of the patient’s phenotype. We performed whole-exome sequencing (WES). WES libraries were prepared using SeqCap EZ MedExome (Roche Sequencing, Pleasanton, CA) and sequenced on a HiSeq2500 platform. Using literature research, a selection of BBS and obesity associated genes was generated (Supplementary data). Variants found by WES were screened against the list of selected genes to detect known and novel causes of genetic causes of obesity and/or BBS. Variant classification was performed according to the recommendations of the American College of Medical Genetics and Genomics [7]. The identified variants were submitted to the Leiden Open Variation Database (LOVD). Sequential segregation analysis of detected variants in the patient’s parent was performed using Sanger sequencing.
Results
Two heterozygous variants in IFT74 (NC_000009.12, NM_025103.3): c.[371_372del];[1685–1G>T] p.[(Gln124Argfs*9)]; [p.?] were identified. The first variant is a novel deletion of two nucleotides causing a frameshift and premature stop, which would likely lead to nonsense-mediated decay. The second variant is an intronic variant in the splice consensus sequence, which has already been described in the other IFT74 patient (ClinVar RCV000240867.2) [5]. Splice prediction software predicts a complete loss of this splice donor site. Both variants were classified as probably pathogenic. Sanger sequencing showed that the variants were inherited from the parents, confirming that the variants are indeed biallelic. Both the variants and the phenotype are submitted to LOVD (https://databases.lovd.nl/shared/genes/IFT74). The variant IDs are #0000604191 and #0000604192, respectively. The individual ID is #00269286 and the phenotype ID is #0000210664.
Discussion
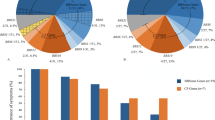
This is the second report of IFT74 variants causing a BBS, validating IFT74 as a BBS gene. So far only one previous case of BBS caused by biallelic IFT74 variants has been published by Lindstrand et al. in 2016 [5]. This patient was a 36-year-old male with retinitis pigmentosa, microcephaly, obesity, polydactyly, hypogonadism, and no renal abnormalities. Lindstrand et al. report that their patient had intellectual disability but without developmental delay (sic). This phenotype differs from the phenotype in our patient (Table 1). Interestingly, our patient had macrocephaly, whereas the previously reported patient had microcephaly. Macrocephaly is more frequently observed in BBS cases than microcephaly [8]. The macrocephaly could also be familial in our case, since the father has an OFC of +2SD. Moreover, the phenotype difference between the two patients is especially important regarding the normal intelligence in our patient and intellectual disability in the Lindstrand patient. We want to emphasize this difference because of its importance for prenatal diagnostics and genetic counseling. Around 60% of BBS patients have learning difficulties, which are usually mild to moderate [9]. The intellectual phenotype of IFT74-associated BBS now ranges from intellectual disability to normal intellectual capacity. Both cases did not have renal anomalies. Since renal problems are observed in 53–82% of BBS cases [1], more cases need to be described to find out if absence of renal problems in our cases are coincidental or if the renal phenotype is less severe in IFT74-associated BBS cases. Future studies and reports of BBS patients with IFT74 variants are needed to gain insight in the complete clinical spectrum and the causes of the phenotype differences. The previously reported case had the same splice variant as our patient (c.168501G>T), but the second variant was different. There was a deletion of ∼20 kb encompassing exons 14–19 of the long transcript of IFT74. The deletion does not impair the function of the short isoform. The splice variant that occurs in both patients also affects the long isoform. Lindstrand et al. hypothesize that their proband is hypomorphic for IFT74 function. The second variant found in our patient (c.371_372del p.(Gln124Argfs*9)) causes a premature stop which would affect both isoforms. With only two known patients, it is difficult to predict whether there could indeed be a genotype–phenotype correlation.
With regards to phenotype differences, it remains to be investigated whether IFT74 variants are involved in the oligogenic inheritance of BBS, in which variants at different BBS loci could modify the severity of the phenotype [10]. Currently, only ten tests available in the Genetic Testing Registry offer IFT74 sequencing [11]. Of all 373 BBS-related gene panels (including retinitis pigmentosa panels, obesity panels, and kidney panels) there are only nine panels in the registry that include IFT74 [12]. Therefore, we recommend IFT74 sequencing in unsolved cases with the clinical diagnosis of BBS and add this gene to BBS gene panels. This case report also serves as an example of how an exome based approach for diagnostics might be advantageous over a targeted based approach. In this case exome sequencing was performed, but data were analyzed using a virtual gene panel. Using this approach the analysis started with a set of known genes associated with the phenotype of interest and was extended with the analysis of additional genes. In cases where the parents are sequenced as well, the entire exome can be “opened up” to search for novel candidate genes. A virtual gene panel provides a mechanism to include and rapidly add genes of interest and to exclude the analysis of certain genes to minimize the risk of incidental findings [13].
In conclusion, this is the second patient with BBS due to biallelic IFT74 variants, confirming its status as a BBS gene.
References
Forsythe E, Beales PL. Bardet–Biedl syndrome. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, editors. Seattle, WA: GeneReviews((R)); 1993.
Forsythe E, Kenny J, Bacchelli C, Beales PL. Managing Bardet–Biedl syndrome-now and in the future. Front Pediatr. 2018;6:23.
Taschner M, Lorentzen E. The intraflagellar transport machinery. Cold Spring Harb Perspect Biol. 2016;8:a028092.
Schaefer E, Stoetzel C, Scheidecker S, Geoffroy V, Prasad MK, Redin C, et al. Identification of a novel mutation confirms the implication of IFT172 (BBS20) in Bardet–Biedl syndrome. J Hum Genet. 2016;61:447–50.
Lindstrand A, Frangakis S, Carvalho CM, Richardson EB, McFadden KA, Willer JR, et al. Copy-number variation contributes to the mutational load of Bardet–Biedl syndrome. Am J Hum Genet. 2016;99:318–36.
Bujakowska KM, Zhang Q, Siemiatkowska AM, Liu Q, Place E, Falk MJ, et al. Mutations in IFT172 cause isolated retinal degeneration and Bardet-Biedl syndrome. Hum Mol Genet. 2015;24:230–42.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Moore SJ, Green JS, Fan Y, Bhogal AK, Dicks E, Fernandez BA, et al. Clinical and genetic epidemiology of Bardet-Biedl syndrome in Newfoundland: a 22-year prospective, population-based, cohort study. Am J Med Genet A. 2005;132A:352–60.
Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet–Biedl syndrome: results of a population survey. J Med Genet. 1999;36:437–46.
Beales PL, Badano JL, Ross AJ, Ansley SJ, Hoskins BE, Kirsten B, et al. Genetic interaction of BBS1 mutations with alleles at other BBS loci can result in non-Mendelian Bardet–Biedl syndrome. Am J Hum Genet. 2003;72:1187–99.
Genetic Testing Registry: IFT74. 2019. https://www.ncbi.nlm.nih.gov/gtr/all/tests/?term=80173[geneid].
Genetic Testing Registry: Bardet–Biedl. 2019. https://www.ncbi.nlm.nih.gov/gtr/all/tests/?term=bardet-biedl+.
Lohmann K, Klein C. Next generation sequencing and the future of genetic diagnosis. Neurotherapeutics. 2014;11:699–707.
Acknowledgements
We are very grateful to the proband and her parents for their cooperation and permission regarding this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee of the Erasmus Medical Center and was conducted in accordance with the Helsinki Declaration.
Informed consent
Written informed consent was obtained from the parents of the proband for publication of the medical data and photographs.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kleinendorst, L., Alsters, S.I.M., Abawi, O. et al. Second case of Bardet–Biedl syndrome caused by biallelic variants in IFT74. Eur J Hum Genet 28, 943–946 (2020). https://doi.org/10.1038/s41431-020-0594-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-020-0594-z
This article is cited by
-
High diagnostic yield in skeletal ciliopathies using massively parallel genome sequencing, structural variant screening and RNA analyses
Journal of Human Genetics (2021)
-
A missense mutation in IFT74, encoding for an essential component for intraflagellar transport of Tubulin, causes asthenozoospermia and male infertility without clinical signs of Bardet–Biedl syndrome
Human Genetics (2021)