Abstract
Purpose
To evaluate Microperimetry (MP) and multifocal electroretinogram (mfERG) as whole-macula functional markers of treatment response in naive diabetic macular oedema (DMO) patients undergoing ranibizumab treatment.
Methods
An exploratory sub-analysis of a prospective study (NCT01947881-CHARTRES). Patients received three monthly ranibizumab injections (loading dose) followed by pro re nata (PRN) regimen during 1 year. At baseline, during and after treatment (Months 0, 3, 6 and 12), subjects were tested using BCVA, OCT, MP and mfERG. MP was performed in the central 12°, and retinal sensitivity was measured overall (mean sensitivity (MS)), and in three concentric rings (R1–R3). mfERG P1 amplitude and implicit time were measured over six concentric rings (R1–R6).
Results
Thirty-two eyes were included. MP mean and rings sensitivity were significantly lower in DMO (p < 0.001). After loading dose, a significant improvement in retina sensitivity was observed, particularly in good BCVA responders (MS = +2.28 dB; R1 = +2.33 dB, R2 = +2.20 dB, R3 = +2.25 dB; p = 0.049). Overall retinal sensitivity was significantly correlated with BCVA improvement (r = 0.54; p = 0.026) and inversely correlated with OCT central subfield thickness improvement (r = −0.39; p = 0.026). mfERG amplitude and implicit time were also lower in DMO (p < 0.011). An improvement of mfERG P1 amplitude and implicit time in R1 was noted in good responders after ranibizumab loading dose (+16.49 nV/deg2; p = 0.013 and −0.005 ms; p = 0.048, respectively). When changing to PRN treatment regimen, BCVA was maintained during the 12 months of follow-up but worsening of the visual function was detected by MP and mfERG.
Conclusions
Microperimetry and mfERG were able to demonstrate DMO functional improvement after treatment loading dose, as well as early visual changes when treatment regimen was switched to PRN.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR), namely diabetic macular oedema (DMO), is a major cause of vision loss in working-age people, with significant personal, social and economic impact [1].
Anti-vascular endothelial growth factor (anti-VEGF) agents, such as bevacizumab, ranibizumab and aflibercept, have revolutionized treatment in DMO [2,3,4]. However, in order to evaluate treatment response, most randomized clinical trials still use best-corrected visual acuity (BCVA) as a primary endpoint, and central retinal thickness (CRT) reduction as a secondary endpoint. BCVA, a test that identifies the number of letters read on a distant vision chart, may not reflect the daily visual problems patients face, which can lead to a significant impact in their quality of life. Besides that, cut-off values of BCVA improvement frequently considered clinically significant in the course of a therapy, have been widely discussed by Food and Drugs Administration [5, 6] and investigators [7, 8] due to several limitations, including subjectivity of the method. This leads to the need of validating other functional evaluations as methods for assessing diseases progression or treatment efficacy.
While DR is mainly considered a microvascular disease [9], there is an increased recognition that neural changes occur in diabetes [10,11,12]. Psychophysiological and electrophysiological measurements of retinal function might address this issue, evaluating the neural component of DR in a larger retinal area, avoiding the subjectivity of BCVA. Microperimetry (MP) in DR and DMO, has proven to be an effective functional method in the examination of retina sensitivity changes [13,14,15]. By presenting multiple luminous stimuli of different intensities in several locations of the central retina, it objectively measures the achromatic luminance threshold in foveal and parafoveal regions. By a built-in eye tracking system and simultaneous imaging of the posterior pole, it allows a direct and precise association between retinal function and localized structural alterations. Multifocal electroretinography (mfERG) [16], can also concurrently extract retinal responses generated at multiple retinal locations, enabling topographic mapping of retinal function in the central 40–50° of the retina and improving the functional evaluation of retinal diseases. Studies have shown that mfERG can show neuroretina changes in diabetic patients without retinopathy [17], with retinopathy [12, 18] and with DMO [19,20,21]. In DMO, the most consistent changes seem to be amplitude decrease and implicit time increase of P1 (the positive peak that follows a focal flash) [21].
To the best of our knowledge, no previous studies have quantitatively evaluated improvement or lack of improvement after anti-VEGF treatment with both MP and mfERG, nor have they related these changes to improvements in BCVA or CRT. Therefore, this study aims to evaluate functional vision changes, determined by MP and mfERG, in eyes with DMO at baseline and after ranibizumab loading dose, as well as, after 6 and 12 months of follow-up. In addition, we also investigated if these methods correlate with visual acuity (VA) or optical coherence tomography (OCT).
Materials and methods
Study design and participants
An exploratory sub-analysis of an observational, longitudinal and prospective study (ClinicalTrials.gov identifier NCT01947881-CHARTRES) [22] was performed at the Association for Innovation and Biomedical Research on Light and Image in collaboration with the Ophthalmology Department, Centro Hospitalar e Universitário de Coimbra. Research and data collection were approved by the local ethics committee and adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients before being included in this sub-analysis and after an explanation of the nature of participation.
Adult patients with type 2 diabetes and treatment-naïve centre-involving DMO were enroled, defined by central subfield thickness ≥300 µm in the study eye, evaluated by spectral-domain OCT (Spectralis OCT, Heidelberg Engineering GmbH, Heidelberg, Germany), and with a BCVA below 79 ETDRS letters. The study recruitment occurred between January 2014 and January 2015. Exclusion criteria were previous anti-VEGF or macular laser treatment (in both eyes), other causes of macular oedema (in the study eye), cataract precluding fundus observation, proliferative DR, either active or treated in the previous 3 months, aphakia, uncontrolled glaucoma, arteriothrombotic event in the previous 6 months, pregnancy and breastfeeding and glycated haemoglobin higher than 11.0%.
Simultaneously, age-matched healthy subjects without DM or any other diagnosed vitreoretinal disease were included during the recruitment of the study, as a control group for MP and mfERG results. The same exclusion criteria were applied, and these subjects underwent a unique visit with a full ophthalmic examination and the above mentioned functional tests.
Study protocol
Study patients were submitted to a baseline full ophthalmic evaluation, including BCVA, dilated fundus examination, colour fundus photography and spectral-domain OCT (Spectralis OCT, Heidelberg Engineering GmbH, Heidelberg, Germany). BCVA was measured and recorded as letters read at 4 m on ETDRS charts. If less than 20 letters were read at 4 m, BCVA was evaluated at 1 m. Final BCVA letter score was calculated by adding the number of letters read at 4 m plus 30 (or the number of letters read at 1 m). Patients received a course of monthly intravitreal injections of ranibizumab (Lucentis, 0.5 mg in 0.05 mL; Novartis Europharm Limited, Camberley, UK) for 3 months, followed by a period of 12 months of pro re nata (PRN), according to the standard practice for DMO treatment and the Summary of Product Characteristics, and underwent mfERG and MP before the first injection (M0). One month after the third injection (M3), BCVA measurements, OCT, mfERG and MP were repeated, as well as at months 6 and 12 (M6 and M12).
Microperimetry
MP was performed using MP1 Microperimeter (Nidek, Gamagori, Japan) in all patients and control subjects. A customized radial grid of 45 stimuli in the central 12° was used with stimuli size Goldman III and 200 ms of projection time. The fixation target was a 1° red cross and stimulation was performed in a white, monochromatic background at 4 asb. The starting stimulus light attenuation was set at 10 dB and a 4–2 double staircase strategy was used with an built-in automatic eye tracker that compensates for eye movements. All subjects (patients and controls) underwent MP with dilated pupils. A 5-min mesopic visual adaptation and a pre-test training were performed in all subjects before starting the test. Overall mean sensitivity (MS) of the entire 12° area was analysed as well as the MS of three concentric rings in the same area: (R1-2°; R2-4°; R3-6°), covering ~1, 3 and 6 mm, respectively, of the central retina area.
Multifocal ERG
mfERG was recorded monocularly using a CRT monitor (Retiscan; Roland Consult, Wiesbaden, Germany), according to International Society for Clinical Electrophysiology of Vision guidelines [23] in all patients and controls. The projected stimulus consisted of 103 scaled hexagons. The recordings were performed under room light conditions and before CFP or OCT to avoid retinal cells saturation. Study eye pupil was fully dilated and fellow eye was occluded by a pad. Summed responses from six concentric ring/annuli defined as R1 <3°, R2 3–7.8°, R3 7.8–15°, R4 15–24°, R5 24–31° and R6 31–42°, were used for analysis. These were described as P1 amplitude density (nV/deg2) and implicit time (ms). The P1 amplitude was measured from N1 through to P1 peak, whereas the P1 implicit time was the time from the onset of the light stimulus to the P1 peak.
Statistical analysis
Baseline (M0) MP MS and baseline (M0) mfERG P1 amplitude and implicit time were compared between the enroled DMO patients and a sample of 62 age-matched control subjects. Repeated-measures ANOVA was performed to analyse changes at four timepoints (M0, M3, M6 and M12) of MP MS and mfERG P1 amplitude and implicit time in all DMO patients, and subdivided by BCVA response to anti-VEGF treatment categories: poor responders (decrease/increase < 5 letters), responders (increase ≥ 5 and <10 letters) and good responders (increase ≥ 10 letters). BCVA response groups were based on the type of response to ranibizumab treatment reported by previous studies [3, 24, 25]. OCT CRT at M0, M3, M6 and M12 was also used for correlation analysis between retinal structure and functional MP and mfERG parameters. Continuous variables were described by mean and standard deviation. Categorical values were described by absolute frequencies and percentages. Two-independent samples t-test and paired samples t-test were used, after checking for normality with Shapiro–Wilk test. Spearman correlation analysis was performed. A receiver operating characteristic (ROC) analysis was performed to identify the best predictors (MP MS and mfERG P1 amplitude and implicit time) for a BCVA improvement >10 ETDRS letters. All analyses were performed using STATA®, version 13.1 (StataCorp, College Station, EUA). A p value < 0.05 was considered statistically significant and all tests were two-sided.
Results
Study sample characterization
We included 32 eyes of 32 subjects with treatment-naïve centre-involving DMO that underwent a course of monthly intravitreal injections of ranibizumab for 3 months and were followed for a total of 12 months in a PRN regimen. Subjects had a mean age of 65.76 ± 5.47 years and 62.5% (n = 20) were male. At baseline (M0), mean BCVA was 62.58 ± 9.50 letters (minimum 38, maximum 75 letters), and mean central subfield thickness was 406.35 ± 122.61 µm (minimum 245 µm, maximum 708 µm).
Sixty-two age-matched control subjects were included in the control group for MP and mfERG results (mean age 64.31 ± 7.26 years; age was not significantly different between control and DMO subjects, p = 0.330).
DMO vs controls—baseline (M0) evaluation by microperimetry and mfERG
MP overall MS and rings sensitivity was significantly lower in DMO patients compared to controls (Table 1; mean difference DMO − controls, MS: −9.76 dB; R1: −11.29 dB; R2: −10.09; R3: −9.44 dB; p < 0.001). Retinal sensitivity was gradually increased from central ring (R1-radii 2°) to peripheral rings (R2-radii 4°, R3-radii 6°).
mfERG P1 amplitude was significantly lower in DMO subjects in all studied rings (Table 1; mean difference DMO − controls, R1: −69.78 nV/deg2; R2: −32.43 nV/deg2; R3: −19.98 nV/deg2; R4: −13.22 nV/deg2; R5: −9.34 nV/deg2 and R6: −7.34 nV/deg2; all p < 0.001). P1 implicit time was only significantly different between groups from R4 to R6, though only a small difference was observed (R4: +0.97 ms, p = 0.023; R5: +1.07 ms, p = 0.011 and R6: +1.40 ms, p = 0.001).
DMO—3 months evaluation (M3), immediately after the loading dose (monthly intravitreal RBZ)
After three monthly ranibizumab injections, both BCVA (mean intra-subject improvement, 7.27 ± 9.99 letters, p < 0.001, paired samples t-test) and OCT CRT improved significantly (mean intra-subject improvement, −120.28 ± 130.80 µm, p < 0.001, paired samples t-test). BCVA change was further categorized by range of change in poor responders (decrease/increase < 5 letters), responders (increase ≥ 5 and <10 letters) and good responders (increase ≥ 10 letters). In our sample, 25.0% eyes (n = 8) were classified as poor responders, 31.2% eyes (n = 10) as responders and 43.8% eyes (n = 14) as good responders.
MP overall sensitivity (MS) and rings sensitivity significantly improved after M3 treatment, in good responders only (Table 2; mean intra-subject improvement: MS = +2.28 dB; p = 0.049; rings sensitivity = R1 +2.33 dB, R2 +2.20 dB and R3 +2.25 DB; p = 0.049)
In the same way, mfERG P1 amplitude in R1 was significantly increased after M3 treatment in good responders only (Table 2; mean intra-subject improvement: +16.49 nV/deg2; p = 0.049). A small but significant change was also seen in P1 implicit time, again in good responders (mean intra-subject improvement: −1.12 ms; p = 0.048). No changes in P1 amplitude or implicit time were seen in R2, R3, R4, R5 and R6, regardless of clinical response category (all p > 0.05).
BCVA improvement was moderately and significantly correlated with mfERG P1 amplitude and implicit time improvement in R1 (correlation coefficient, r = 0.36; p = 0.041; r = 0.45; p = 0.009, respectively) but especially with overall retinal sensitivity (correlation coefficient, r = 0.54; p = 0.026). No correlations were found between BCVA and mfERG or MP for peripheral rings.
Conversely and as expected, a moderate inverse correlation between CRT change and overall retinal sensitivity and mfERG P1 amplitude improvements were found (r = −0.39, p = 0.026 and r = −0.38 p = 0.074, respectively).
DMO—6 months and 1-year functional changes under PRN regimen
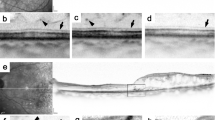
After the loading dose (M3) patients received intravitreal injections under a PRN regimen and were followed at months 6 and 12 (mean n° of injections during 12 months of PRN, 1.78 ± 1.53 IVT). Although BCVA remained unaltered during the follow-up period, when the treatment regimen was changed to PRN, a gradual worsening of visual function was detected by MP and mfERG (Fig. 1).
Microperimetry and mfERG as predictors of functional response to anti-VEGF treatment
Response to treatment was defined as the improvement in number of letters after 3 monthly injections of ranibizumab. Nevertheless, analysing graphs on Fig. 1, we can observe that even before treatment, patients with higher MP sensitivity and mfERG implicit time were the ones that had better BCVA outcomes after therapy. To explore the value of MP and mfERG as baseline discriminators of a good visual response to anti-VEGF therapy, an ROC analysis was performed revealing that both MP sensitivity and mfERG implicit time at R1 were good baseline discriminators of BCVA response, despite not reaching statistical significance (Table 3). mfERG amplitude did not show any discriminative power.
Discussion
In the first step of our analysis we compared our DMO patient’s cohort with an age-matched control cohort regarding MP and mfERG findings. We found that in all studied areas, retina sensitivity, evaluated by MP, was significantly lower in DMO subjects, in comparison to the controls. As expected, the central ring was the most affected, with a progressive increase of sensitivity to the peripheric rings, which is probably related with the increased fluid accumulation in the foveal area. These results are in agreement to previous works showing that increased CRT severely impairs luminous sensitivity [26, 27] and validates MP as a method to demonstrate functional inner retinal impairment in DMO. We also found that mfERG P1 amplitude was likewise significantly and markedly lower in DMO subjects in all studied rings, with an increase of the implicit time, showing functional outer retina impairment [28]. These results confirm the published literature that showed that P1 amplitudes were significantly decreased in DMO patients [19]. Weiner et al., using focal ERG in DMO, also reported decreased amplitudes and longer implicit times [29].
In the second part of our analysis we prospectively evaluated changes in MP and mfERG produced by RBZ loading dose on DMO patients. We evaluated these changes in three clinical (BCVA) response categories: poor responders, responders and good responders. We have shown that after RBZ treatment, MP MS and sensitivity in R1—fovea, R2—parafoveal area, and R3—perifoveal area, as well as mfERG P1 amplitude in R1 were significantly and clearly increased in good responders. These results seem to suggest that DMO functional recovery occurs at the foveal level, as measured by BCVA, but also extends to the entire macular area, as shown by improvements in both MP and mfERG. In the daily practice and in several clinical trials for evaluation of safety and effectiveness of medical products, BCVA is the only used indicator of functional recovery [30]. In fact, it is frequently discussed if BCVA improvements of one or two or even fiveletters, with its individual variability, is significant enough to consider the efficacy of a therapy in improving visual function [6, 7] as it does not always reflect patient’s visual experience [8]. BCVA, as a high contrast test that evaluates the recognition of single black letters in a white chart, reveals to be insufficient in the evaluation of important aspects of visual function as like retina sensitivity in different light conditions. This raises the necessity to validate objective and reliable methods to better characterize and measure the degree of functional vision in each patient. In our study, when correlating BCVA with MP and mfERG before and after treatment, BCVA improvement was moderately and significantly associated with these two functional parameters, reinforcing their potential usefulness as functional biomarkers with clinical utility. Moreover, even before treatment, when no BCVA significant differences exist between patients (as shown in Fig. 1), MP and mfERG values appear to have a good discriminative power to separate patients that will be good or poor responders, after treatment (ROC AUC = 0.65 and 0.68, respectively, Table 3). These results may indicate that different levels of visual dysfunction could occur in parallel with, or even before, BCVA impairment [31], and are worthwhile to be evaluated for a better characterization of DMO patients.
Interestingly, a significant and negative correlation between CRT in OCT and both MP sensitivity and mfERG P1 amplitude was found in our results, confirming the value of OCT as surrogate for visual response in DMO [32]. Therefore, a combined evaluation of functional and structural examinations in DMO would appear to be appropriate for treatment assessments.
Our study also confirmed that better visual function improvement occurs when patients receive monthly injections, and that these improvements decrease when treatment regimen changes to PRN. Studies like RISE and RIDE [4] have shown that monthly RBZ injections were capable of a sustained improvement of vision during 24 months of follow-up, reducing the risk of further vision loss. In an attempt to reduce the burden and costs of this treatment plan, other regimens as PRN [33] or treat-and-extend [34] have been evaluated with non-inferior results. DRCR.net Protocol V [35] recently suggested that patients with centre-involved DMO and good vision can confidently be managed just by observation, scheduling anti-VEGF injections only if vision deteriorates. However, all these studies and treatment regimen, based their retreatment decision on BCVA number of letters. Our data show a maintenance of BCVA results during the PRN regimen but a deterioration of macular function evaluated with both MP and mfERG. Baget-Bernaldiz et al. [36] reached similar conclusions, emphasizing that BCVA and OCT CRT may be insufficient criteria to sustain medical decisions related to re-treatment, since patients quality of vision may suffer a significant impairment not adequately assessed by VA only, possibly losing the opportunity for future recovery.
The major strength of our study is the fact of being one of few studies that quantitatively evaluated the effects of anti-VEGF treatment in DMO visual function, using mfERG and MP and correlating them to BCVA and CRT. While another study has evaluated the effects on RBZ therapy in DMO using mfERG, it used arbitrary categories of improvement and failed to report any inferential statistics or correlations with other markers [37]. It also used pattern ERG for evaluation in DMO, which by the authors own admission, might be an inadequate exam in DMO since it covers a large retinal area and therefore is not sensitive enough for localized changes in the central macular/foveal region. Regarding MP, Malagola et al. [38] have also established a positive correlation between anti-VEGF therapy effects on CRT and functional outcomes (BCVA and MP), but included non-treatment naïve patients with persistent DMO and previous laser therapy, compromising retinal sensitivity values. Other strengths of our study include the prospective, self-controlled design and the comparative baseline evaluation versus age-matched controls. This approach contributes to a thorough evaluation of MP and mfERG changes in DMO, both at baseline and after different treatment stages, allowing the evaluation of functional/structural correlations.
Despite the demonstrated value of both functional methods, mfERG can be a longstanding and complex examination, with wide variability, expensive equipment and specifically built normative databases [39], adding more burden to anti-VEGF therapy which already represents a huge burden for clinicians, particularly considering the increasing number of patients to be evaluated monthly. That said, of both used methods, MP show clear advantages to be applied to clinical practice as it is less time consuming and more reliable and reproductible, giving immediate information about macular functional status that can be compared during treatment course.
The major limitation of this study is the sample size, especially due to the categorization of the patients in three groups of BCVA treatment response. However, the percentage of good responders, poor responders and responders in our sample, is in agreement with previously reported information in other larger studies [3, 22, 24, 25]. Therefore, we believe it can be a representation of what happens in the generality of DMO patients submitted to ranibizumab monotherapy.
In conclusion, MP and mfERG show clear differences between patients with DMO and age-matched controls. Monthly anti-VEGF injections improve not only foveal VA but also macular function as shown by MP and mfERG, while PRN regimen leads to a decrease in these parameters, particularly in retina sensitivity. A combined evaluation of different functional and structural parameters should be considered for an efficient DMO treatment management in order to achieve the best visual results.
Summary
What was known before
-
Visual Acuity is a limited representation of the visual function.
-
New functional endpoints for assessing clinical trials outcomes are needed in diabetic macular oedema.
-
mfERG and microperimetry are objective methods for assessing retinal function.
-
However, there is still a lack of validation of these techniques to be used as functional markers.
What this study adds
-
Microperimetry and mfERG show clear differences between patients with DMO and age-matched controls.
-
Monthly anti-VEGF injections improve not only foveal visual acuity but also macular function as shown by MP and mfERG, while a PRN regimen led to a decrease in these parameters, particularly in retina sensitivity.
-
A combined evaluation of different functional and structural parameters should be considered for an efficient DMO treatment management in order to achieve the best visual results.
References
Bunce C, Wormald R. Leading causes of certification for blindness and partial sight in England & Wales. BMC Public Health. 2006;6:58.
Heier JS, Korobelnik J-F, Brown DM, Schmidt-Erfurth U, Do DV, Midena E, et al. Intravitreal aflibercept for diabetic macular edema: 148-week results from the VISTA and VIVID studies. Ophthalmology. 2016;123:2376–85.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmol. 2011;118:615–25.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase iii randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Csaky KG, Richman EA, Ferris FL. Report from the NEI/FDA ophthalmic clinical trial design and endpoints symposium. Investig Ophthalmol Vis Sci. 2008;49:479–89.
Ranibizumab (Lucentis): Visual Impairment due to Choroidal Neovascularization Secondary to Pathologic Myopia. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2015. https://pubmed.ncbi.nlm.nih.gov/26962598/
Beck RW, Maguire MG, Bressler NM, Glassman AR, Lindblad AS, Ferris FL. Visual acuity as an outcome measure in clinical trials of retinal diseases. Ophthalmology. 2007;114:1804–9.
Chakravarthy U, Pearce I, Banerjee S, Burton BJL, Downey L, Gale R, et al. Patient-reported outcomes in the RELIGHT clinical trial of ranibizumab in diabetic macular oedema. BMJ Open Ophthalmol. 2019;4:1–8.
Gardner TW, Antonetti DA, Barber AJ, LaNoue KF, Nakamura M. New insights into the pathophysiology of diabetic retinopathy: potential cell-specific therapeutic targets. Diabetes Technol Ther. 2000;2:601–8.
Barber AJ. A new view of diabetic retinopathy: a neurodegenerative disease of the eye. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:283–90.
Jackson GR, Barber AJ. Visual dysfunction associated with diabetic retinopathy. Curr Diabetes Rep. 2010;10:380–4.
Santos AR, Ribeiro L, Bandello F, Lattanzio R, Egan C, Frydkjaer-Olsen U, et al. Functional and structural findings of neurodegeneration in early stages of diabetic retinopathy: cross-sectional analyses of baseline data of the EUROCONDOR project. Diabetes. 2017;66:2503–10.
Yohannan J, Bittencourt M, Sepah YJ, Hatef E, Sophie R, Moradi A, et al. Association of retinal sensitivity to integrity of photoreceptor inner/outer segment junction in patients with diabetic macular edema. Ophthalmology. 2013;120:1254–61.
Shen Y, Liu K, Xu X. Correlation between visual function and photoreceptor integrity in diabetic macular edema: spectral-domain optical coherence tomography. Curr Eye Res. 2016;41:391–9.
Wang J, Jie C, Tao Y, Meng N, Hu Y, Wu Z. Macular integrity assessment to determine the association between macular microstructure and functional parameters in diabetic macular edema. Int J Ophthalmol. 2018;11:1185–91.
Sutter EE, Tran D. The field topography of ERG components in man–I. The photopic luminance response. Vis Res. 1992;32:433–46.
Han Y, Adams AJ, Bearse MA, Schneck ME. Multifocal electroretinogram and short-wavelength automated perimetry measures in diabetic eyes with little or no retinopathy. Arch Ophthalmol. 2004;122:1809–15.
Schneck ME, Bearse MA, Han Y, Barez S, Jacobsen C, Adams AJ. Comparison of mfERG waveform components and implicit time measurement techniques for detecting functional change in early diabetic eye disease. Doc Ophthalmol. 2004;108:223–30.
Tehrani NM, Riazi-Esfahani H, Jafarzadehpur E, Mirzajani A, Talebi H, Amini A, et al. Multifocal electroretinogram in diabetic macular edema; correlation with visual acuity and optical coherence tomography. J Ophthalmic Vis Res. 2015;10:165–71.
Greenstein VC, Chen H, Hood DC, Holopigian K, Seiple W, Carr RE. Retinal function in diabetic macular edema after focal laser photocoagulation. Investig Ophthalmol Vis Sci. 2000;41:3655–64.
Bearse MA, Ozawa GY. Multifocal electroretinography in diabetic retinopathy and diabetic macular edema. Curr Diabetes Rep. 2014;14:526.
Santos AR, Costa MÂ, Schwartz C, Alves D, Figueira J, Silva R, et al. Optical coherence tomography baseline predictors for initial best-corrected visual acuity response to intravitreal anti-vascular endothelial growth factor treatment in eyes with diabetic macular edema: the CHARTRES Study. Retina. 2018;38:1110–9.
Hood DC, Bach M, Brigell M, Keating D, Kondo M, Lyons JS, et al. ISCEV standard for clinical multifocal electroretinography (mfERG) (2011 edition). Doc Ophthalmol. 2012;124:1–13.
Elman MJ, Ayala A, Bressler NM, Browning D, Flaxel CJ, Glassman AR, et al. Intravitreal ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology. 2015;122:375–81.
Massin P, Bandello F, Garweg J, Hansen L, Harding S. Efficacy of ranibizumab in diabetic macular edema (RESOLVE Study*). Diabetes Care. 2010;33:2399–405.
Vujosevic S, Midena E, Pilotto E, Radin PP, Chiesa L, Cavarzeran F. Diabetic macular edema: correlation between microperimetry and optical coherence tomography findings. Investig Ophthalmol Vis Sci. 2006;47:3044–51.
Bonnin S, Tadayoni R, Erginay A, Massin P, Dupas B. Correlation between ganglion cell layer thinning and poor visual function after resolution of diabetic macular edema. Investig Ophthalmol Vis Sci. 2015;56:978–82.
Mendoza-Santiesteban CE, Fernández-Cherkasova L, Echavarria OH, Rodríguez RC, Columbié-Garbey Y, Riesgo TJ. Multifocal electroretinography. Semin Ophthalmol. 2010;25:155–64.
Weiner A, Christopoulos VA, Gussler CH, Adams DH, Kaufman SR, Kohn HD, et al. Foveal cone function in nonproliferative diabetic retinopathy and macular edema. Investig Ophthalmol Vis Sci. 1997;38:1443–9.
Drum B, Calogero D, Rorer E. Assessment of visual performance in the evaluation of new medical products. Drug Discov Today Technol. 2007;4:55–61.
Hafner J, Karst S, Schmidt-Erfurth U. Potential imaging biomarkers in the development and progression of diabetic retinopathy. In book: Early events in diabetic retinopathy and intervention strategies. IntechOpen; 2018. p. 9–36.
Diabetic Retinopathy Clinical Research Network, Browning DJ, Glassman AR, Aiello LP, Beck RW, Brown DM, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114:525–36.
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmol. 2010;117:1064–77.e35.
Prünte C, Fajnkuchen F, Mahmood S, Ricci F, Hatz K, Studnička J, et al. Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema: the RETAIN study. Br J Ophthalmol. 2016;100:787–95.
Baker CW, Glassman AR, Beaulieu WT, Antoszyk AN, Browning DJ, Chalam KV, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA. 2019;321:1880–94.
Baget-Bernaldiz M, Romero-Aroca P, Bautista-Perez A, Mercado J. Multifocal electroretinography changes at the 1-year follow-up in a cohort of diabetic macular edema patients treated with ranibizumab. Doc Ophthalmol. 2017;135:85–96.
Comyn O, Sivaprasad S, Peto T, Neveu MM, Holder GE, Xing W, et al. A randomized trial to assess functional and structural effects of ranibizumab versus laser in diabetic macular edema (the LUCIDATE study). Am J Ophthalmol. 2014;157:960–70.
Malagola R, Spinucci G, Cofone C, Pattavina L. Prospective microperimetry and OCT evaluation of efficacy of repeated intravitreal bevacizumab injections for persistent clinically significant diabetic macular edema. Int Ophthalmol. 2013;33:261–7.
Wu Z, Ayton LN, Guymer RH, Luu CD. Comparison between multifocal electroretinography and microperimetry in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2014;55:6431–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santos, A.R., Raimundo, M., Alves, D. et al. Microperimetry and mfERG as functional measurements in diabetic macular oedema undergoing intravitreal ranibizumab treatment. Eye 35, 1384–1392 (2021). https://doi.org/10.1038/s41433-020-1054-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1054-2