Abstract
Objective
To determine the demographic profile, clinical features and surgical outcomes of giant retinal tear (GRT) related retinal detachments (RD) in children.
Methods
In this retrospective study, medical records of children aged 14 years and below, who underwent surgery for RD at our centre in the last 5 years were reviewed. Among these, we selected medical records of children with RDs with GRT, and examined the coloured retinal drawings, ultrawidefield photographs and/or surgical videos.
Results
Out of 1536 medical records, 91 eyes of 87 children (5.6% of all RDs) were included. Mean age was 10.21 ± 3.08 years with male:female ratio of 8.6:1. The most common aetiologies for GRTs were high myopia (28 cases—32.18%) and trauma (25 cases—28.73%). Bilateral RD were possibly present in 29/87 (33.3%) cases. Six months follow up data was available for 82/91 eyes. Overall retinal re-attachment was achieved in 52/82 (63.41%) eyes; in 33/82 (40.24%) eyes retinal attachment could be achieved by a single surgery. Absence of proliferative vitreoretinopathy (PVR) (OR: 2.44, p-value:0.03, 95%CI: 1.21–5.08) or PVR-A (OR: 3.62, p-value: 0.03, 95%CI: 1.52–12.26) and presence of preexisting posterior vitreous detachment (OR: 7.14, p-value: 0.02, 95%CI: 1.31–38.73) were associated with successful retinal re-attachment after single surgery. Median time to presentation of cases succeeding after 1 surgery was 10 days. Ambulatory vision (1/60 and better) at final followup could be achieved in 45/82 (54.88%) eyes.
Conclusion
GRT relatedRDs constitute a significant proportion of paediatric RDs. Anatomical success can currently be achieved in a large number of cases. Early surgery, absence of PVR and presence of PVD are associated with higher surgical success.
Similar content being viewed by others
Introduction
Giant retinal tears (GRT) are defined as tears that extend more than 90 degrees or 3 clock hours circumferentially [1]. GRT-related retinal detachment (RD) is an emergency demanding prompt management. Delay in surgical intervention can lead to accelerated proliferative vitreoretinopathy (PVR) and/or choroidal detachment jeopardizing reattachment of the retina.
Most of the adult cases of GRT are idiopathic and have a high male preponderance [2]. Other risk factors include trauma, high myopia [3], Marfan’s syndrome [4], Stickler syndrome, hereditary vitreoretinopathies [5], and acute retinal necrosis [6]. Iatrogenic GRTs are also known to occur following fishing for dislocated nucleus during complicated cataract surgeries [7], large sclerotomies, foreign body removal from the vitreous cavity, frequent exchange of instruments during vitrectomy, jamming of instruments at port site in cases of vitreous haemorrhage [8] and following refractive surgeries [9]. Giant retinal dialysis (GRD) on the other hand is pathognomonic of trauma unless proven otherwise [10]. Other rare causes could be iatrogenic or cases of bilateral inferotemporal dialysis of the young (BIRDY) [11].
GRTs are usually classified on the basis of extent of the break in degrees or clock hours and the orientation of flaps as flat, rolled or inverted [12]. The incidence of proliferative vitreoretinopathy (PVR) is higher in cases of GRT as a large area of Retinal Pigment Epithelium is exposed to the vitreous cavity. Following the advent of perfluorocarbon liquids (PFCL), the success rate of GRT surgeries has increased tremendously [13]; nonetheless, paediatric GRT related RDs pose a unique and challenging scenario [14]. Different reasons have been cited for poor prognosis of paediatric RDs compared to adults [15, 16]. Most studies have clubbed paediatric GRTs along with adult cases and have studied both as a single cohort. No study yet has elucidated the clinical and surgical profile of a large paediatric cohort. A study by Mehdizadeh et al., divided cases of GRT based on age (into less than or more than 30 years) and found that younger age was a significant risk factor for occurrence of GRT. However, this distinction is not a true representation of the paediatric age group [17].
A previous study from our centre on surgical outcomes of microincision vitrectomy surgery (MIVS) in GRT, has shown that 53% of cases are of the paediatric age group. The present study aims to detail the demographic profile, common aetiologies, clinical features and surgical outcomes of GRT related RDs in a larger paediatric population over a 5-year period [18].
Materials and methods
The study was conducted at tertiary eye centre in North India. The study was approved by the Institutional Ethics Board (IEB) and was done in accordance with the tenets of the Declaration of Helsinki. In this retrospective study, medical records of consecutive children aged 14 years and below who underwent surgical management for rhegmatogenous RD between January 2015 and December 2019 were reviewed, and those with GRT as a cause for RD were included for the final analysis. A total of 1536 medical records of children with detailed examination and surgical findings, inclusive of Modified Amsler-Dubois scheme based retinal charts which met the consensus of 2 authors (R.C. and N.H.) were included. Cases with retinal tears less than three clock hours, those with tractional, exudative retinal detachment and combined RDs were excluded.
Data including demographic profile, intraocular pressure (IOP), corrected for distance visual acuity (CDVA), anterior segment and posterior examination was examined. We extracted data on extent of RD, retinal breaks with location, retinal lattice degenerations, status of PVR, presence of posterior vitreous detachment (PVD) and choroidal detachment (CD). Presence of myopia, hypotony, lens status, and associated aetiology was also noted. Out of 1536 medical records, 91 eyes of 87 children met the final screening criteria and were included for analysis.
PVR was graded as per Updated Retina Society Classification [19] system while traumatic RDs were identified as per pre-existing criteria defining traumatic RD [20]. Patients with a refractive error > −6 dioptres were considered as having high myopia. Visual acuity was recorded using Snellen’s visual acuity chart and converted to LogMAR scale for statistical analysis. Children with more than 6 month follow up after the last surgery were considered for the second part of the study (surgical outcomes). Surgical details of every surgery including silicon oil removal were analysed. Data were entered in Microsoft excel spreadsheet and analysed using STATA Statistical Software, Version 12 (Statacorp, College Station, Texas, USA). Multivariate logistic regression analyses were used to study risk factors of retinal detachment and potential factors for retinal attachment following single primary vitreo-retinal surgery. P-value of less than 0.05 was considered significant.
Results
A total of 1536 medical records of children with rhegmatogenous RDs over a 5-year period were reviewed, and 91 eyes of 87 children with GRT were included for final analysis (5.6% of all paediatric RDs). Demographic profile of the sample is presented in Table 1. There was a high male preponderance of 8.6:1 (78 boys and 9 girls). The median time of presentation in cases of GRTs (n = 91) was 15 days (1–365 days).
The most common aetiologies were high myopia (28/87—32.18%) and trauma (25/87—28.73%). Five cases had high myopia as well as history of trauma. Two out of these five had other signs of ocular trauma and were grouped under traumatic aetiology, while the other three not having evidence of ocular trauma were included under high myopia. Iatrogenic causes included 2 cases of previous vitreoretinal surgery, one case of buckling surgery with inadvertent globe perforation and one case following removal of an iris cyst. Out of four cases with concurrent bilateral disease, two were high myopes, one had undergone bilateral cataract surgery for congenital cataract and one was idiopathic (Table 2). In cases of high myopia with GRT, the axial length of the fellow eye was available for 11 out of 28 cases and the mean was 28.18± 2.61 mm and the spherical equivalent of the fellow eye was available for 18 out of 28 cases and it was −11.72 ± 4.48 D. In cases of hereditary vitreo-retinopathy (5/13) the mean axial length was 28.38± 2.15 mm and spherical equivalent of the fellow eye was −8.86 ± 4.99 D.
On evaluating the posterior segment, 83/91 (90.3%) eyes had a total RD, 4 eyes had subtotal detachment (attached retina less than 3 clock hours), 2 eyes had nasal detachment, 1 each temporal detachment and superior detachment. In 2 eyes, the macula was attached. Breaks were classified into four groups according to their extent. The average extent of breaks was 6.39 ± 3.05 clock hours, with 60 eyes having an extent of less than 180°. Out of these, the break was found in the temporal quadrant in 35 eyes (58.33%), nasal in 12 (20%), superior in 11 (18.33%) and inferior in 2 (3.33%) eyes. Five eyes with GRTs had a radial rip. Thirteen eyes had a choroidal detachment (CD) associated with the retinal detachment (14.28%). 54 eyes (59.34%) had some form of PVR of which 28 eyes (30.76%) had PVR C and above. Extent of break, classification of PVR and orientation of the flap were recorded (Table 3).
Sixteen children had some form of retinal detachment in the fellow eye (Table 3). In four patients the retinal detachment in both the eyes was visibly due to a GRT. Two of these children had concurrent bilateral GRT related RD on the first presentation itself, one of them had WWOP areas in the fellow eye that were not lasered and developed GRT related RD after 3 years. The fourth child had GRT related RD in one eye and an operculated hole in the fellow eye at presentation. Although the hole was lasered, the patient presented after 6 months with a GRT related RD in the fellow eye (GRT in the quadrant opposite to the lasered hole). Thirteen cases had either atrophic bulbi (6 eyes) or phthisis bulbi (6 eyes) or had an artificial eye (1 eye). If we presume that the loss in vision in these eyes was also secondary to a retinal detachment, then the incidence of bilateral retinal detachment in our series is 33.3% (29/87). This is a presumed figure. However, considering the young age of our cohort it is highly likely that both eyes suffered a similar pathology.
The peripheral retina of the fellow eyes of 13 children could not be examined (phthisis bulbi, atrophic bulbi and artificial eye). Out of the remaining children, 25 had some lesion in the retinal periphery (Table 3). Prophylactic laser treatment was done in 18 out of these 25 children. However, the nature of treatment (extent and configuration) was not uniform and was performed at the discretion of the treating ophthalmologist.
Surgical data
Of the 91 eyes of 87 children with GRT, 6 eyes were deemed inoperable on examination under anaesthesia and 3 children were lost to follow up and were excluded from this analysis. Thus, finally a total of 82 eyes underwent surgery and were followed up for more than 6 months after surgery. The retina was attached in 33/82 eyes (40.24%) eyes following a single vitreo-retinal surgery. These eyes had successfully undergone silicon oil removal. Further 19 eyes were attached following more than one vitreo-retinal surgery. BCVA improved from 2.13 ± 0.37 logMAR to 1.22 ± 1.88 logMAR (p-value-0) in the patients with attached retina (52 eyes). The overall average number of vitreo-retinal surgeries done was 1.57 ± 0.65.
Lens management
Twenty-seven patients underwent some form of lens management. Ten eyes underwent lens aspiration with PCIOL (posterior chamber intraocular lens) of which 8 eyes had cataract and 2 eyes had lens subluxation. Fourteen eyes underwent pars plana lensectomy during the surgery of which 3 eyes had intraoperative lens touch, 4 patients had subluxated cataractous lens and rest 7 eyes had cataract. Three eyes underwent IOL explant of which 2 eyes had de-centred PCIOL and one eye had intraoperative IOL drop.
Intraoperative data
All children underwent primary vitreo-retinal surgery using MIVS with or without encirclage (number 240 band) and silicon oil endotamponade. An encirclage was placed in 28 eyes in the primary surgery itself and in 5 eyes, the encirclage was put during the second vitreo-retinal surgery. Triamcinolone assisted posterior vitreous detachment (PVD) induction was done in 29/82 (35.36%) eyes whereas 53 eyes had preexisting complete PVD. Internal limiting membrane peeling at the posterior pole was done in 16 eyes during the primary surgery and in 15 eyes during the second surgery. PFCL was not used in 6 eyes. Of the remaining 76 eyes in which PFCL was used, 61 eyes underwent direct PFCL-oil exchange and 14 eyes underwent PFCL air exchange followed by silicon oil injection. In one eye with extensive PVR and inferior GRT, PFCL was kept as a short term tamponade for 10 days followed by PFCL-oil exchange.
Postoperative data
Thirty-three eyes had undergone silicon oil removal and were attached at final follow-up following the first surgery whereas 49 developed a re-detachment. Forty children out of this group of cases with re-detachment were taken up again for a second vitreo-retinal surgery. Successful retinal re-attachment was possible only in 17 (42.5%) of these eyes. The retina of two more eyes could be attached after a third vitreo-retinal surgery. Thus, in all retinal re-attachment could be achieved in 52/82 (63.41%) eyes. (Table 4) At 6 months follow up silicon oil removal had been done for 40 out of the 52 eyes with attached retina.
The potential factors for retinal attachment following a single surgery and risk factors for failure to achieve retinal re-attachment at 6 months of follow up were assessed (Table 5). Absence of PVR (OR: 2.44, p-value: 0.033, 95%CI:1.21–5.083), PVR-A (OR: 3.62, p-value: 0.029, 95%CI: 1.52–12.26) and presence of pre-existing PVD (OR: 7.14, p-value:0.023, 95%CI: 1.31–38.73) favoured successful reattachment following a single surgery. The median duration between onset of symptoms to surgery for cases that required only one surgery for retinal attachment was 10 days and for those who underwent more than one surgery was 18 days. This difference was also statistically significant (p −0.026).
Only 360 degree GRT with PVR C or greater could be considered as risk factor for failure to achieve retinal attachment. (OR:4.32, p-value: 0.024, 95%CI: 1.11–7.53).
Complications
Intraoperative complications included subretinal PFCL in 5 patients, intraoperative choroidal detachment in 1 patient, suprachoroidal cannulas in 1 patient and the need for extensive retinectomy in 4 patients. Postoperative complications included hyperoleon in 21 patients, buckle infection in one patient, secondary glaucoma in 8 patients, band shaped keratopathy in 5 patients and postoperative endophthalmitis in one patient. Out of the 8 patients with glaucoma, 5 were controlled with medication, 2 patients underwent diode laser cyclophotocoagulation (DLCP) and in one patient Ahmed Glaucoma Valve was put. Of these 8 eyes, 2 eyes had uncontrolled IOP and developed total glaucomatous cupping.
Discussion
The incidence of rhegmatogenous RD in the paediatric age group is far less than that of adults (0.38–0.69 versus 12.4 cases per 100,000 population which makes only 0.5–8% of all RDs) [21]. The percentage of GRT related RD among paediatric RDs (5.6% in our study) was found comparable to other studies (6.3–12.8%) [21,22,23,24]. The gender ratio was similar to those of adult population [25]. The percentage of GRT related RD in adults is much less at around 1.5% [26]. A high percentage of GRTs seen in the paediatric RDs in our study could possibly be due to a referral bias. Ours is a tertiary care referral institute with good access to an experienced anaesthetic team and facilities for pre and post anaesthesia care, which could have resulted in a larger number of complex paediatric cases being referred to this institution. Cases of adult GRT’s may be taken care of elsewhere where surgery can be done under local anaesthesia. A previous study from our centre on surgical outcomes of MIVS in GRT showed that 53% of cases of GRT were of paediatric age groups.
Trauma and high myopia were the most common causes of GRT in our study which differs from the adult population (mostly idiopathic—54.8%) [25]. Only 6 of our cases were idiopathic with other cases having some form of systemic or ocular association. This data suggests the need for thorough systemic and ocular examination in the paediatric age group. Incidence of trauma in our study (28.73%) was similar to those reported previously (16.2–35.3%) [18, 27]. Similarly, high myopia (32.18%) was also within the range of previous studies (24–35.3%) [17, 18, 25, 28].
Pre-operative visual acuity was found to be counting fingers or less due to early macular involvement and rapid progression to a total RD in most of these cases. Intraocular pressure can be low in RDs and lower still in giant breaks due to the large break providing an alternate pathway for aqueous drainage leading to hypotony and choroidal detachment [27]. However, in our series there were 19 eyes (20.65%) that had raised intraocular pressure which could be due to the trabecular meshwork insult following trauma or severe inflammation that may occur in children.
The time at presentation with GRT was 15 days, which was similar when compared to the normal distribution (13.5–20 days) [18, 25]. Interestingly, even though children with GRT presented within 15 days, 33% of them had lost vision in the fellow eye previously. In all probability, this could be due to a RD going unnoticed in those eyes.
The incidence of bilateral RD (if we attribute the cause of loss of vision in the fellow atrophic/phthisical eyes to RD as hypothesized above) in our series is 33%. This is more than that in the adult population (16.1%) [29]. Loss of vision in one eye in children goes unrecognized or is not reported due to fear or anxiety. Only when a subsequent loss of vision in the only seeing eye incapacitates their daily functioning that an eye problem is acknowledged by their parents or teachers and medical attention is sought. A previous study has also shown that the incidence of bilateral GRT was high (14%) as well as the presence of a break in the fellow eye was 36% [30]. In our study, most patients with peripheral treatable lesions in the fellow eyes underwent prophylactic laser. However, the number of such eyes in our study and the follow up period is small to determine the utility of these interventions. Laser retinopexy and cryopexy in the fellow eye have been suggested in literature but there is no consensus regarding the benefit of fellow eye prophylaxis [31]. A meta analysis on fellow eye intervention by Ang G S et al did not find any strong evidence to support or refute prophylactic treatment [32]. However, a recent retrospective study by Verhoekx et al. have found significantly lower rates of retinal detachment in the fellow eye of idiopathic GRT’s who underwent 360° prophylactic laser [33].
Most cases in our study had a total RD with macular involvement. This highlights rapid progression of RD in cases of GRT. This is in contrast to the study by Rodriguez et al. in the adult population where 35% GRTs had macula on RD [28]. The extent of GRT and location of break were similar to other studies and we similarly observed that the extent of break did not affect the final outcome [28]. Still, PVR is known to be severe as breaks get larger, ultimately affecting retinal reattachment.
30 eyes (29.1%) had significant PVR (PVR C or worse) which was significantly higher compared to the adult population. The British Giant Retinal Tear Epidemiology Eye Study (BGEES) [25] have found only 11.3% of their study population to have significant PVR. PVR depends on a lot of factors like age of the patient, time of presentation, aetiology, other ocular inflammatory disease, presence of choroidal detachment or vitreous haemorrhage, extent and site of the break [34]. It is known that children have greater risk of severe PVR [35]. Thus perhaps the paediatric age group in our cases itself contributed to the higher incidence of PVR. GRTs are also a risk factor for hypotony and CD. In our study 11 (10.6%) children had an associated choroidal detachment. There are no studies in the literature that have recorded the incidence of CD in GRTs. In a study by Azad et al. [36], 4% of all rhegmatogenous RDs had an associated CD. Higher incidence of CD in GRT related RDs may also be responsible for greater PVR in such cases.
Retinal reattachment was achieved in around 63.4% and ambulatory vision (1/60 and better) was achieved in 54.8% of eyes which is similar (68% and 58%) to a clinical trial done by Scott et al. [37] which included 34 eyes with GRT (age less than 16 years). However, these percentages are low when compared to results seen in the adult population [27, 28]. Secondary glaucoma was the most common postoperative complication and two eyes developed near total cupping despite maximal medications and surgery.
To conclude, GRT associated RDs constitute a significant proportion of paediatric detachments. High myopia & trauma are the most common risk factors for giant tears in children. A significant number of cases may also have other associated ocular or systemic disorders. About one-third of children may develop retinal detachment in both eyes. Delay in availing treatment for the first eye leads to irreversible loss of vision in this eye. There is lack of consensus regarding prophylactic treatment of the fellow eye. Early diagnosis and surgery within 10 days of symptoms, lack of PVR and presence of PVD improve chances of retinal re-attachment.
Summary
What was known before
-
Most studies on giant retinal tears have been either done in adults or have clubbed paediatric GRTs with adults.
-
Surgical outcomes are becoming better with the advent of MIVS, widefield view system during surgery and perfluorocarbons.
What this study adds
-
Paediatric GRTs are different than adult GRTs in terms of aetiology, clinical features and surgical outcomes.
-
Surgical success and functional outcomes is lower compared to those of adult GRTs.
References
Freeman HM, Schepens CL, Couvillion GC. Current management of giant retinal breaks. II. Trans Am Acad Ophthalmol Otolaryngol Am Acad Ophthalmol Otolaryngol. 1970;74:59–74.
Ghasemi Falavarjani K, Alemzadeh SA, Modarres M, Alemzadeh SA, Parvarash MM, Naseripour M, et al. Outcome of surgery in patients with giant retinal tear: 10 years experience. Eye Lond Engl. 2017;31:1284–9.
Schepens CL, Dobble JG, McMEEL JW. Retinal detachments with giant breaks: preliminary report. Trans Am Acad Ophthalmol Otolaryngol Am Acad Ophthalmol Otolaryngol. 1962;66:471–9.
Sharma T, Gopal L, Shanmugam MP, Bhende PS, Agrawal R, Shetty NS, et al. Retinal detachment in Marfan syndrome: clinical characteristics and surgical outcome. Retin Philos Pa. 2002;22:423–8.
Shapiro MJ, Blair MP, Solinski MA, Zhang DL, Jabbehdari S. The importance of early diagnosis of Stickler syndrome: Finding opportunities for preventing blindness. Taiwan J Ophthalmol. 2018;8:189–95.
Topilow HW, Nussbaum JJ, Freeman HM, Dickersin GR, Szyfelbein W. Bilateral acute retinal necrosis. Clinical and ultrastructural study. Arch Ophthalmo. 1982;100:1901–8.
Aaberg TM, Rubsamen PE, Flynn HW, Chang S, Mieler WF, Smiddy WE. Giant retinal tear as a complication of attempted removal of intravitreal lens fragments during cataract surgery. Am J Ophthalmol. 1997;124:222–6.
Shinoda H, Nakajima T, Shinoda K, Suzuki K, Ishida S, Inoue M. Jamming of 25-gauge instruments in the cannula during vitrectomy for vitreous haemorrhage. Acta Ophthalmol. 2008;86:160–4.
Ozdamar A, Aras C, Sener B, Oncel M, Karacorlu M. Bilateral retinal detachment associated with giant retinal tear after laser-assisted in situ keratomileusis. Retin Philos Pa. 1998;18:176–7.
Vote BJ, Casswell AG. Retinal dialysis: are we missing diagnostic opportunities? Eye Lond Engl. 2004;18:709–13.
Hollander DA, Irvine AR, Poothullil AM, Bhisitkul RB. Distinguishing features of nontraumatic and traumatic retinal dialyses. Retin Philos Pa 2004;24:669–75.
Albert DM, Miller JW, Azar DT, Giant retinal tears Albert DM, Miller JW, Azar, DT (eds). In: Albert & Jakobiec’s principles and practice of ophthalmology. 2008:2351.
Mikhail MA, Mangioris G, Best RM, McGimpsey S, Chan WC. Management of giant retinal tears with vitrectomy and perfluorocarbon liquid postoperatively as a short-term tamponade. Eye Lond Engl. 2017;31:1290–5.
Chang S, Lincoff H, Zimmerman NJ, Fuchs W. Giant retinal tears. Surgical techniques and results using perfluorocarbon liquids. Arch Ophthalmol. 1989;107:761–6.
Nuzzi R, Lavia C, Spinetta R. Paediatric retinal detachment: a review. Int J Ophthalmol. 2017;10:1592–603.
Wenick AS, Barañano DE. Evaluation and management of pediatric rhegmatogenous retinal detachment. Saudi J Ophthalmol. 2012;26:255–63.
Mehdizadeh M, Afarid M, Haqiqi MS. Risk factors for giant retinal tears. J Ophthalmic Vis Res. 2010;5:246–9.
Kumar V, Kumawat D, Bhari A, Chandra P. Twenty-five-gauge pars plana vitrectomy in complex retinal detachments associated with giant retinal tear. Retin Philos Pa. 2018;38:670–7.
Machemer R, Aaberg TM, Freeman HM, Irvine AR, Lean JS, Michels RM. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–65. 15
Cox MS, Schepens CL, Freeman HM. Retinal detachment due to ocular contusion. Arch Ophthalmol. 1966;76:678–85.
Fivgas GD, Capone A. Pediatric rhegmatogenous retinal detachment. Retin Philos Pa. 2001;21:101–6.
Weinberg DV, Lyon AT, Greenwald MJ, Mets MB. Rhegmatogenous retinal detachments in children: risk factors and surgical outcomes. Ophthalmology. 2003;110:1708–13.
Chen S-N, Jiunn-Feng H, Te-Cheng Y. Pediatric rhegmatogenous retinal detachment in taiwan. Retin Philos Pa. 2006;26:410–4.
Zafar SN, Qureshi N, Azad N, Khan A. Retinal detachment in paediatric patients. J Coll Physicians Surg-Pak. 2013;23:261–4.
Ang GS, Townend J, Lois N. Epidemiology of giant retinal tears in the United Kingdom: the British Giant Retinal Tear Epidemiology Eye Study (BGEES). Invest Ophthalmol Vis Sci. 2010;51:4781–7.
Mitry D, Singh J, Yorston D, Siddiqui MAR, Wright A, Fleck BW, et al. The predisposing pathology and clinical characteristics in the Scottish retinal detachment study. Ophthalmology. 2011;118:1429–34.
Scott IU, Murray TG, Flynn HW, Feuer WJ, Schiffman JC, Perfluoron Study Group. Outcomes and complications associated with giant retinal tear management using perfluoro-n-octane. Ophthalmology. 2002;109:1828–33.
Rodriguez M, Lin J, Townsend JH, Smiddy WE, Albini TA, Berrocal AM, et al. Giant retinal tears: clinical features and outcomes of vitreoretinal surgery at a university teaching hospital (2011–2017). Clin Ophthalmol Auckl Nz. 2018;12:2053–8.
Lee SY, Ong SG, Wong DWK, Ang CL. Giant retinal tear management: an Asian experience. Eye Lond Engl. 2009;23:601–5.
Freeman HM. Fellow eyes of giant retinal breaks. Trans Am Ophthalmol Soc. 1978;76:343–82.
Ang A, Poulson AV, Goodburn SF, Richards AJ, Scott JD, Snead MP. Retinal detachment and prophylaxis in type 1 Stickler syndrome. Ophthalmology. 2008;115:164–8.
Ang GS, Townend J, Lois N. Interventions for prevention of giant retinal tear in the fellow eye. Cochrane Database Syst Rev. 2012;15:CD006909.
Verhoekx JSN, van Etten PG, Wubbels RJ, van Meurs JC, van Overdam KA. Prophylactic laser treatment to decrease the incidence of retinal detachment in fellow eyes of idiopathic giant retinal tears. Retin Philos Pa. 2020;40:1094–7.
Girard P, Mimoun G, Karpouzas I, Montefiore G. Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. Retin Philos Pa. 1994;14:417–24.
Chang S, Lopez JM Giant retinal tears and proliferative vitreoretinopathy. In: Ryan SJ, editor. Retina.4th ed. St. Louis: Mosby; 2006. pp. 2345–51.
Azad R, Tewari HK, Khosla PK. Choroidal detachment in association with retinal detachment. Indian J Ophthalmol. 1984;32:143–7.
Scott IU, Flynn HW, Azen SP, Lai MY, Schwartz S, Trese MT. Silicone oil in the repair of pediatric complex retinal detachments: a prospective, observational, multicenter study. Ophthalmology. 1999;106:1399–407. discussion 1407–1408.
Author information
Authors and Affiliations
Contributions
NH, SVA and RC were responsible for designing the protocol and methodology of the study. NH, AK and SV were involved in patient recruitment. NH and AK were involved in data acquisition and creating the excel spreadsheet. NH, RC, SVA and VK were responsible for writing the manuscript. NH and DS were involved in analysis of data and interpretation of results. PC, PV, AK and RV were involved in final editing of the manuscript and provided feedback on the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hasan, N., Azad, S.V., Kaginalkar, A. et al. Demography, clinical profile and surgical outcomes of paediatric giant retinal tear related retinal detachments. Eye 35, 3041–3048 (2021). https://doi.org/10.1038/s41433-021-01621-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01621-y
This article is cited by
-
Management, risk factors and treatment outcomes of rhegmatogenous retinal detachment associated with giant retinal tears: scoping review
International Journal of Retina and Vitreous (2024)
-
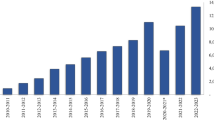
The rising tide of rhegmatogenous retinal detachment in Germany: a nationwide analysis of the incidence, from 2005 to 2021
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)