Abstract
Background
To compare productivity of National Health Service cataract lists performing unilateral cataract (UC) surgery vs Immediate Sequential Bilateral Cataract Surgery (ISBCS).
Methods
Five 4-hour lists with ISBCS cases and five with UC were observed using time and motion studies (TMS). Individual tasks and timings of each staff member in theatre was recorded by two observers. All operations were performed by consultant surgeons under local anaesthesia (LA).
Results
Median number of eyes operated per 4-hour list was 8 (range 6–8) in the ISBCS group and 5 (5–7) in the UC group (p = 0.028). Mean total theatre time (defined as time between the entry of the first patient and the exit of the last patient from theatre) was 177.12 (SD 73.62) minutes in the ISBCS group and 139.16 (SD 47.73) minutes in the UC group (p = 0.36). Mean time to complete two consecutive unilateral cataract surgery operations was 48.71 minutes compared to 42.23 minutes for a single ISBCS case (13.30% time saved). Based on our collected TMS data, a possible 5 consecutive ISBCS cases and 1 UC (total 11 cataract surgeries) could be performed during a four-hour theatre session, with a theatre utilisation quotient of 97.20%, contrasting to nine consecutive UC, with a theatre utilisation quotient of 90.40%.
Discussion
Performing consecutive ISBCS cases under LA on routine cataract surgery lists can increase surgical efficiency. TMS are a useful way to investigate surgical productivity and test theoretical models for efficiency improvements.
Similar content being viewed by others
Introduction
Cataract Surgery (CS) is the commonest elective operation in the United Kingdom (UK) National Health Service (NHS) with 452,000 performed in England during 2018–2019 [1]. With increasing life expectancy [2], it has been estimated there will be a 50% increase in the number of CS operations by 2035 [3]. Furthermore, because of increases in chronic age-related conditions which are associated with the development of cataracts, such as diabetes, and surgical backlog due to COVID-19 pauses in elective surgery [4, 5], this demand may be greater than anticipated.
More ophthalmologists are performing immediate sequential bilateral cataract surgery (ISBCS), with surveys showing 86% and 67% of surgeons in the United States and Europe, respectively, undertaking ISBCS [6, 7]. However, in the UK in 2018–2019, only 379 ISBCS cases were performed by 173 surgeons, suggesting that UK Ophthalmologists may still have reservations concerning routine ISBCS surgery [1]. To date, three randomised control trials comparing ISBCS to delayed sequential bilateral cataract surgery (DSBCS) have shown refractive outcomes and complication rates to be similar [8,9,10]. The risks of bilateral simultaneous endophthalmitis are low, with only nine reported cases reported in the literature to date [11,12,13,14,15,16,17,18,19]. Economically, cost-analysis has shown DSBCS to be more costly than ISBCS [20], and patients who undergo ISBCS require fewer hospital visits, less travel time, and faster post-operative recovery times compared to DSBCS [21].
The efficient utilisation and organization of operating rooms (OR) are important and have potential to improve surgical productivity to address CS demand [22, 23]. Our published study using Time and Motion Studies (TMS) to measure OR efficiency indicated that theatre productivity could be improved by adjusting the number of allied health professionals (AHPs) and their given tasks, allowing for a greater number of CS operations to be performed per list [22]. Using our TMS data, we constructed a hypothetical model for ISBCS, which showed a mean time saved of 15.80% when performing a single ISBCS case compared to two unilateral cases (UC) [23]. To test this hypothetical model and to investigate possible efficiencies of ISBCS within the OR, we conducted this present study in a “real world” setting. TMS was used to compare OR efficiency of ISBCS only theatre lists to lists with only UC. The study was performed in an NHS setting during a post-COVID lockdown period.
Methods
This was a quality improvement project to assess the efficiency of the operating room theatre in a teaching hospital by measuring the time taken for the key tasks of surgeons and allied health professionals. The project was approved by the Guys and St.Thomas’ Ophthalmology Audit and Quality Improvement Project Team (audit number 11620). Data was collected in accordance with the tenets of the Declaration of Helsinki and the UK Data Protection Act. TMS was used to continuously observe five lists consisting of only ISBCS cases, and five lists consisting of only unilateral cases. Each of the ten observed lists was a 4-hour cataract theatre session in a UK university teaching hospital on a Saturday morning. Each CS was performed by using micro-incision phacoemulsification technique and intraocular lens implantation. All listed cases were performed under local anaesthesia (LA) by one of two consultant ophthalmic surgeons and were non-training lists. For ISBCS cases, the cases were listed based on a specific listing criterion which includes the absence of factors which render the case high risk, including the absence of previous ocular surgery, diabetes mellitus, or corneal dystrophies [24]. Patients were counselled as to the specific risks and benefits of ISBCS prior to listing.
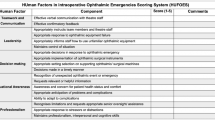
Each CS list was observed by two observers using a macros-enabled Excel template spreadsheet (Microsoft, Redmond, Washington, USA) to allow accurate live recordings of each pre-defined key task by the ophthalmic surgeon and each AHP. The key tasks (Table 1) have been defined in our previously published papers [22, 23]. In this study we added the additional key task of the instillation of povidone iodine and surgical draping of the patient. The measurement of ‘eye-to-eye’ was used as further proxy measure of patient turnover and was defined as the interval between removal of the lid speculum from the eye of one patient (or first eye of a patient) and insertion of a lid speculum in the eye of the next patient (or second eye of the same patient). Three previously defined theatre quotients [22, 23] were measured based on the TMS data: the theatre utilisation quotient (TUQ) (time between commencement of the first case on the list (patient entry into OR) and the end of the last case on the list (patient exit from OR)/four hours); the surgery quotient (SQ) (the proportion of time that the operating surgeon was performing surgery/total theatre time), and the efficiency quotient (EQ) (the proportion of time that the operating surgeon was engaged in a key task/total theatre time). The total theatre time was defined as the time (minutes) between the entry of the first patient on the list into the OR and the exit of the last patient out of the OR.
Subgroup statistical analysis was performed using GraphPad Prism version 8.0.0 for Mac (GraphPad Software, San Diego, California USA). Data are presented as parametric and non-parametric as appropriate.
Results
Ten theatre lists were observed, with 5 lists consisting of only UC, and 5 consisting of exclusively ISBCS cases (Table 2). TMS of a total of 65 individual CS operations were prospectively recorded, of which 18 were ISBCS cases (36 eyes) and 29 were UC. In patients undergoing ISBCS, following completion of the first eye CS, the operating surgeon verbally checked with each patient to check if they were comfortable to proceed with the second eye. In two cases of planned ISBCS, the second eye CS was cancelled due to the posterior capsular rupture of the first eye in one patient, and a patient declining to proceed with the second eye. The TMS of these two cases were still included in the final statistical analysis as they were planned ISBCS cases. Surgeon A completed 6 surgical lists (3 ISBCS, 3 UC) and surgeon B completed 4 surgical lists (2 ISBCS lists and 2 UC). The median number of individual CS operations performed was 8 (range 6-9) in the ISBCS lists and 5 [5,6,7] in the unilateral lists (UC) (p = 0.028) (Table 2). The median number of AHPs was 4 [4, 5] in the ISBCS lists and 4 [4] in the UC (p = 1.0). The median patient turnover was 7.29 minutes (6.15–11.15) in the ISBCS lists and 12.14 minutes in the UC (7.55–37.68) (p < 0.0001).
Table 3 displays the mean durations duration of the key tasks observed in minutes. Significant differences were found for several time parameters. The mean patient time in theatre was 40.17 (12.83) for ISBCS and 20.11 (8.96) for UC (p < 0.0001). The mean patient exit time was 3.43 (1.37) for ISBCS and 1.46 (0.70) for UC (p < 0.0001). The mean time for instillation of povidone iodine and surgical draping of the patient was 1.14 (0.55) for ISBCS and 1.56 (0.78) for UC (p = 0.012). The mean time for the scrub nurse to prepare the phacoemulsification machine was 3.05 (1.32) for ISBCS and 2.20 (0.90) for UC (p = 0.0053). Mean scrub nurse clearing up time of the trolley was 4.46 (1.19) for ISBCS and 5.70 (2.28) for UC (p = 0.03).
The mean TUQ was 73.80% (30.67) for ISBCS and 57.98% (19.89) for UC (p = 0.36) (Table 3). The mean SQ was 38.96% (21.57) for ISBCS and 30.1% (13.58) for UC (p = 0.46). The mean EQ was 53.29% (26.73) for ISBCS and 40.78% (15.65) for UC (p = 0.39).
Figure 1 displays the mean TMS of one ISBCS case (both eyes of one patient) compared to two UC (one eye of two consecutive patients). The mean time to complete one ISBCS case was 42.23 minutes compared to 48.71 minutes for two unilateral cases, leading to 6.48 minutes time saved (13.30%).
From our collected TMS data (Table 3), it would to be possible to complete in our OR, a maximum of 5 consecutive ISBCS cases plus a unilateral case, leading to a total theatre time of 233.26 minutes, a TUQ of 97.19%, and the completion of 11 CS operations. Similarly, for UC, nine cases are possible during a 240-minute period, with a total theatre time of 216.95 minutes and a possible TUQ of 90.40%.
Discussion
This study utilises TMS to compare OR efficiency of ISBCS lists compared to UC, in a “real world” setting of a public sector (NHS) teaching hospital in the UK. We found that compared to completing two consecutive unilateral cases, the completion of a single ISBCS case led to 13.30% time saved (6.48 minutes). Our TMS data (Table 3) for our unit indicates that a possible 5 consecutive ISBCS cases and 1 additional UC (under LA) could be performed during a 240-minute theatre session, with a possible TUQ of 97.19% (total theatre time 211.15 minutes). Conversely, only 9 UC could be performed, with a TUQ of 90.40% (total theatre time 216.95 minutes). This gives ISBCS-only lists a potential productivity gain of 22% (2 eyes). Increasing the number of cases booked onto the ISBCS and UC lists is also likely enhance the mean surgery quotients of 38.96 (21.57) and 30.10 (13.58), respectively.
A theoretical TUQ of 97.19%, as suggested above, might appear unrealistic in a “real world setting”, considering the risk of any complications and need for anterior vitrectomy which would prolong overall surgical time. This risk of potential complications on an ISBCS list can be reduced by selecting low-risk cases and even if we factor in ‘buffer time’ to deal with any potential complications, it should still be possible to perform 5 ISBCS cases (10 eyes) during a 240-minute theatre list (a TUQ of 87.98%, allowing for 28.85 minutes of “buffer” time). This gain of 11% in surgical productivity (1 eye) may appear minimal but equates to 10 extra eyes over the course of ten 240-minute lists during a five-day week.
Our figure of 13.30% time saved for one ISBCS compared to 2 UC, is slightly lower than our hypothesised figure of 15.80% (6.62 minutes) from our previous study [23]. In this current study, the mean time to switch to the second eye following completion of CS in the first eye was 7.56 minutes during an ISBCS case (Fig. 1), a turnover time which was more than double our hypothesised time of 3.75 minutes from previous studies [23]. This discrepancy in turnover time highlights an area which might be improved to enhance OR efficiency when completing an ISBCS case and highlighted the role of TMS in improving surgical productivity.
During the completion of an ISBCS case, we found that the mean time for a patient to exit the OR following completion of second eye CS was 3.43 minutes, which was significantly higher than then 1.43 minutes for UC cases (p < 0.0001). Following CS, we typically tape clear eye shields to the operated eye, and we noted and postulate that following ISBCS, patients (many of whom are elderly) may need more time to be escorted out of the OR, because of bilateral visual impairment due to bilateral eye shield placement.
The AHPs primed the phacoemulsification machine in a shorter time during UC lists compared to the ISBCS lists (2.20 minutes vs 3.05 minutes, p = 0.0053) (Table 3). This difference may partly be accounted for by 2 case outliers (6.45 minutes and 6.22 minutes) in the same ISBCS list where the irrigation tubing needed to be replaced. AHPs were able to clear the operating trolley in a shorter time in ISBCS lists (4.46 vs 5.70, p = 0.03) and we postulated that this difference may partly be due to presence of an extra AHP on one of the ISBCS lists. The cleaning and preparation of the operating bed between patients was completed in a shorter time during UC lists (1.13 vs 1.63, p = 0.0078) and may be partly explained by extra time needed for an AHP to escort each ISBCS patient out of theatre prior to aiding with cleaning of the operating bed. The surgeon-performed iodine cleaning and draping of the patient was slightly longer during UC lists (1.56 vs 1.14, p = 0.012) and may be partly due to the surgeon already being familiar with how best to drape and position the patient’s first eye during an ISBCS case.
Appropriate patient selection for ISBCS, along with appropriate patient counselling is essential to ensure that ISBCS lists can be run safely and efficiently [24], and we have devised a detailed protocol for selecting patients who are suitable and low risk for ISBCS under LA. Indeed, a patient survey of 267 patients in our unit showed that ISBCS was acceptable to 45%, suggesting that patients are open to undergoing ISBCS [25]. However, a study on current ISBCS practice in the UK showed that ISBCS is typically being performed on more challenging cases, with patients being of a younger age group, of higher surgical complexity, positioning difficulties, and a greater use of general anaesthesia (GA), rather than routine LA cases [26]. Although there is a strong argument for booking select cases for ISBCS under GA, the effect on OR efficiency is unclear. It can be postulated, however, that completion of 4 consecutive ISBCS cases may not be possible during a 240-minute theatre session, considering the administration of GA and post-operative recovery time [23]. TMS of both UC and ISBCS lists under GA would be beneficial in evaluation OR efficiency in such settings.
ISBCS has been shown to allow cost-savings for hospitals as well as patients themselves compared to DSBCS [20, 21, 27] The findings of the multi-centre BICAT-NL study showed that the mean total savings when performing ISBCS was €403 compared to DSBCS [27]. Our TMS is the first study to show potential theatre efficiencies in practice. Our previous TMS study on unilateral lists showed that in some high-volume centres up to 13.5 eyes were undergoing CS on a 240-minute list [22]. Hence, in centres where high-volume cases are being performed by experienced surgeons, there is potential for even more efficient use of ISBCS lists.
We appreciate the limitations of our study. Ten lists were observed (5 ISBCS, 5 UL). We acknowledge that this is a small number. Conducting a TMS study to evaluate OR efficiency is both time consuming and labour intensive. Furthermore, ensuring that consecutive ISBCS cases are booked on the same list is challenging both for the hospital administrator staff, as well as for patients themselves. Moreover, the surgical pauses of elective CS during the pandemic have had a significant negative impact on the surgical training of residents [28]. To ensure that this study did not impact training, each list was observed on a Saturday morning, thereby ensuring that the weekday trainee teaching lists were not affected. Our findings may have limited applicability to the potential efficiency of training lists which consist of ISBCS cases. However, we believe that senior trainees with adequate CS experience would be qualified to operate on ISBCS cases who are listed under LA. Further TMS studies comparing the efficiency of UL and ISBCS training lists would shed more light on identifying any surgical productivity gains. It must be noted that lists performed on a Saturday could possibly be more efficient than weekday lists due to less disruption from collateral clinical services.
The median number of eyes operated was 8 (range 6-9) on the ISBCS lists and 5 [5,6,7] for UC (p = 0.028) (Table 2). This study was conducted during the COVID-19 pandemic where several additional precautions were implemented into our cataract surgery pathway in accordance with national recommendations to reduce patient and staff exposure to COVID-19. This included mandatory COVID-19 swabbing of patients 3 days prior to surgery, followed by patient self-isolation prior. Due to these additional steps and challenges with COVID-19 testing and isolation, with short-notice cancellations that could not be replaced, it was not always possible to completely fill the observed lists. The authors appreciate that efficient listing of cases to ensure full lists and therefore aid in maximising theatre utilisation is an important aspect of overall OR productivity.
Each list was run by one of two experienced consultant surgeons, with surgeon A running 6 lists (3 ISBCS, 3 UL) and surgeon B running four lists (2 ISBCS, 2 UL). This was an attempt to limit inter-surgeon variability regarding key tasks such as surgical time, draping time and surgeon note taking. The same group of AHPs were present for each list. AHP paperwork time was not recorded. One of the reasons was that more than one AHP may be making recordings during each session (which may not be related to the case) and it was challenging to record these timings accurately in real time by the observers.
Adhering to safety protocols is essential to conducting safe ISBCS surgery and in our unit, separate batches of consumables and disposables for each eye of an individual patient were identified by theatre nurses the day before the theatre list to ensure that adequate equipment and intra-ocular lenses are available to adhere to local protocol. This additional step in preparation for ISBCS lists was not measured in this study and must be taken into consideration when preparing for ISBCS lists to avoid on the day setbacks in the OR. Efficient use of the OR begins prior to the day of surgery, with ‘one-stop’ cataract clinics (to minimise hospital visits) where future dates for CS are provided during the pre-assessment are essential for efficient booking of lists and better theatre utilisation. Such steps are increasingly practiced in NHS practices, as well as in ophthalmology departments around the world such as the Aravind Eye Care System in India [29].
We have previously highlighted that a significant hurdle which limits the more widespread use of ISBCS in the UK public healthcare sector is the lack of hospital reimbursement following simultaneous second eye CS, leaving units at a financial disadvantage when conducting ISBCS [23]. The current evidence shows the cost-effectiveness of ISBCS compared to DSBCS in both adult and paediatric patients [21, 27, 30, 31]. There are also financial benefits to the patient who undergo DSBCS, as patients who undergo ISBCS have less total travel time to and from hospital, and in turn, there is the further potential benefit of each patient leaving a smaller carbon footprint due to less carbon emission [20, 26]. Hence, the consideration of non-punitive tariffs for ISBCS in the NHS may enable its more widespread use [23].
Conclusions
This study compares the surgical efficiency in the ophthalmic OR between ISBCS and UC lists by utilising TMS. Our findings suggest that listing more ISBCS cases (which are of low surgical complexity) under LA on routine surgical lists has the potential to enhance productivity of cataract surgery lists, with potential surgical gains in our unit of 11–22%. Utilisation of ISBCS in high-volume cataract surgery units, has great potential to enhance operating room efficiency to complement the cost savings associated with ISBCS.
Summary
What was known before
-
The safety profile and refractive outcomes of immediately sequential bilateral cataract surgery (ISBCS) is comparable to delayed sequential bilateral cataract surgery (DSBCS).
-
ISBCS is more cost-effective than DSBCS with reduced hospital expenditure and reduced patient travel time.
-
Time and motion studies can be utilised to evaluate surgical efficiency within the operating room.
What this study adds
-
ISBCS has the potential to improve the productivity of cataract surgery within the National Health Service compared to unilateral cataract (UC) lists.
-
Selection of appropriate low-risk surgical cases can allow multiple ISBCS to be performed under local anaesthesia.
-
The introduction of ISBCS under local anaesthesia can potentially enhance operating room efficiency and reduce hospital expenditure.
How might these results change the focus of research or clinical practice
-
Utilisation of ISBCS under local anaesthesia in high-volume cataract surgery units have potential to enhance operating room efficiency.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author (DOB) on reasonable request.
References
The Royal College of Ophthalmologists. National Ophthalmology Database Audit. 2020. https://www.nodaudit.org.uk/u/docs/20/hqsrgmurnv/NOD%20Audit%20Full%20Annual%20Report%202020.pdf. Accessed on 3rd March 2022.
Office for National Statistics. Overview of the UK population: February 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/november2018. Accessed 3rd March 2022.
The Royal College of Ophthalmologists. The Way Forwards: options to help meet demand for the current and future care of patients with eye disease. https://www.rcophth.ac.uk/wp-content/uploads/2021/12/RCOphth-The-Way-Forward-Cataract-Summary-300117.pdf. Accessed 3rd March 2022.
Stevens S, Pritchard A. Next steps on NHS response to COVID-19. NHS England and NHS Improvement. 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf. Accessed 3rd March 2022.
Robman L, Taylor H. External factors in the development of cataract. Eye. 2005;19:1074–82. https://doi.org/10.1038/sj.eye.6701964.
Amsden LB, Shorstein NH, Fevrier H, Liu L, Carolan J, Herrinton LJ. Immediate sequential bilateral cataract surgery: surgeon preferences and concerns. Can J Ophthalmol. 2018;53:337–41.
Mills EC, Zarei-Ghanavati M, Liu CSC. Immediate sequential bilateral cataract surgery: The rationale, implementation, and beliefs of ophthalmic surgeons across Europe. J Cataract Refract Surg. 2019;45:1725–31.
Lundstrom M, Albrecht S, Nilsson M, Astrom B. Benefit to patients of bilateral same-day cataract extraction: Randomized clinical study. J Cataract Refract Surg. 2006;32:826–30.
Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Leivo T, Kivela T. Simultaneous bilateral versus sequential bilateral cataract surgery: Helsinki Simultaneous Bilateral Cataract Surgery Study Report 1. J Cataract Refract Surg. 2011;37:992–1002.
Serrano-Aguilar P, Ramallo-Farina Y, Cabrera-Hernandez JM, Perez-Silguero D, Perez-Silguero MA, Henriquez-de la Fe F, et al. Immediately sequential versus delayed sequential bilateral cataract surgery: safety and effectiveness. J Cataract Refract Surg. 2012;38:1734–42.
Ozdek SC, Onaran Z, Gurelik G, Konuk O, Tekinsen A, Hasanreisoglu B. Bilateral endophthalmitis after simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2005;31:1261–2.
Puvanachandra N, Humphry RC. Bilateral endophthalmitis after bilateral sequential phacoemulsification. J Cataract Refract Surg. 2008;34:1036–7.
Benezra D, Chirambo MC. Bilateral versus unilateral cataract extraction: advantages and complications. Br J Ophthalmol. 1978;62:770–3.
Kashkouli MB, Salimi S, Aghaee H, Naseripour M. Bilateral Pseudomonas aeruginosa endophthalmitis following bilateral simultaneous cataract surgery. Indian J Ophthalmol. 2007;55:374–5.
Mota SH. Pseudomonas aeruginosa-induced bilateral endophthalmitis after bilateral simultaneous cataract surgery: case report. Arq Bras Oftalmol. 2018;81:339–40.
Qi SR, Hebert M, Chen MY, Arshinoff SA, Tourville E. “Bilateral Endophthalmitis After Immediately Sequential Bilateral Cataract Surgery (ISBCS) in an Immunodeficient Patient”. Acta Sci Ophthalmol. 2022;5.4:73–76.
Chen MY, Qi SR, Kratholm J, Arshinoff SA. “Burkholderia Postoperative Endophthalmitis and an Outbreak Including Bilateral Simultaneous Postoperative Endophthalmitis”. Acta Sci Ophthalmol. 2022;5.2:43–52.
Friling E, Johansson B, Lundström M, Montan P. Postoperative Endophthalmitis in Immediate Sequential Bilateral Cataract Surgery: A Nationwide Registry Study. Ophthalmology 2022;129:26–34.
Callaway NF, Ji MH, Mahajan VB, Moshfeghi DM. Bilateral Endophthalmitis after Immediately Sequential Bilateral Cataract Surgery. Ophthalmol Retin. 2019;3:618–9.
Lundstrom M, Albrecht S, Roos P. Immediate versus delayed sequential bilateral cataract surgery: an analysis of costs and patient value. Acta Ophthalmol. 2009;87:33–8.
Rush SW, Gerald AE, Smith JC, Rush JA, Rush RB. Prospective analysis of outcomes and economic factors of same-day bilateral cataract surgery in the United States. J Cataract Refract Surg. 2015;41:732–9.
Roberts HW, Myerscough J, Borsci S, Ni M, O’Brart DPS. Time and motion studies of National Health Service cataract theatre lists to determine strategies to improve efficiency. Br J Ophthalmol. 2018;102:1259–67.
O’Brart DP, Roberts H, Naderi K, Gormley J. Economic modelling of immediately sequential bilateral cataract surgery (ISBCS) in the National Health Service based on possible improvements in surgical efficiency. BMJ Open Ophthalmol. 2020;5:e000426. https://doi.org/10.1136/bmjophth-2019-000426.
Low S, Tran J, McGurk C, Gupta A, Roberts HW, O’Brart D. Cat-12 Tool to reduce intraoperative complications for phacoemulsification and femtosecond laser assisted cataract surgery. Curr Eye Res. 2021;46:1071–2.
Shah V, Naderi K, Maubon L, Jameel A, Patel DS, Gormley J, et al. Acceptability of immediate sequential bilateral cataract surgery (ISBCS) in a public health care setting before and after COVID-19: a prospective patient questionnaire survey. BMJ Open Ophthalmol. 2020;5:e000554. https://doi.org/10.1136/bmjophth-2020-000554.
Buchan JC, Donachie PHJ, Cassels-Brown A, Liu C, Pyott A, Yip JLY, et al. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: Report 7, immediate sequential bilateral cataract surgery in the UK: Current practice and patient selection. Eye 2020;34:1866–74. https://doi.org/10.1038/s41433-019-0761-z.
Simons R. Will we all be doing bilateral cataract surgery because of superior cost effectiveness? In: 39th ESCRS Congress, October 8–11, 2021; Amsterdam. Available from: https://escrs.conference2web.com/#!resourcegroups/order=relevant&query=r.simons.
Campbell S, Hind J, Lockington D. Engagement with ophthalmic simulation training has increased following COVID-19 disruption—the educational culture change required? Eye. 2021;35:2660–1. https://doi.org/10.1038/s41433-021-01494-1.
Ravilla T, Ramasamy D. Efficient high-volume cataract services: the Aravind model. Community Eye Health. 2014;27:7–8.
Leivo T, Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Kivelä T. Simultaneous bilateral cataract surgery: economic analysis; Helsinki Simultaneous Bilateral Cataract Surgery Study Report 2. J Cataract Refract Surg. 2011;37:1003–8.
Cernat A, Jamieson M, Kavelaars R, Khalili S, Bhambhwani V, Mireskandari K, et al. Immediate versus delayed sequential bilateral cataract surgery in children: a cost-effectiveness analysis. Br J Ophthalmol 2022;106:211–7. https://doi.org/10.1136/bjophthalmol-2020-316507.
Funding
DOB holds non-commercial research grants with Rayner Ltd and J & J Inc. He holds stock in Sparca Inc. HR has undertaken paid consultancy work for Alcon Inc (Fort Worth, TX, USA) in the past 36 months and has received educational honoraria from Thea Pharmaceuticals Ltd (Keele, UK). SR has undertaken consultancy work for Sanofi and Leo Pharma.
Author information
Authors and Affiliations
Contributions
DOB, KN, and HR contributed to the study design, data interpretation, and preparation of the manuscript. MB, SL, CFJL, AJ, KT, LOG, SR and LL contributed to the data collection and revision of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Naderi, K., Lam, C.F.J., Low, S. et al. Time and Motion Studies to assess surgical productivity in cataract theatre lists within the National Health Service: Immediate Sequential Bilateral Cataract Surgery versus Delayed Sequential Bilateral Cataract Surgery. Eye 37, 3751–3756 (2023). https://doi.org/10.1038/s41433-023-02593-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02593-x