Abstract
Excessive salt intake is an established risk factor for hypertension. We conducted a cross-sectional study to examine the association between salty taste recognition and estimated salt intake and masked hypertension in a healthy Japanese normotensive population. The participants were 892 apparently healthy community residents (246 men and 646 women) aged between 40 and 74 years with blood pressure below 140/90 mm Hg. Salty taste recognition was assessed using a salt-impregnated taste strip. Daily salt intake was calculated as estimated 24 h urinary sodium excretion using spot urine tests. Each participant performed home blood pressure measurements for a minimum of 5 days per week. The participants were classified into three groups according to their salty taste recognition threshold evaluated by the salt concentrations of the taste strips (0.6%, 0.8%, and ≥ 1.0%). In women, the multivariate odds ratio (95% confidence interval) for masked hypertension ( ≥ 135/85 mm Hg) was 2.98 (1.16–7.64) in the ≥ 1.0% group compared with that in the 0.6% group. In men, the proportion of masked hypertension in the ≥ 1.0% group did not differ from that in the 0.6% group, and no correlation was identified between estimated daily salt intake and the salty taste recognition threshold. In conclusion, impairment of salty taste recognition was associated with masked hypertension in women even with normal blood pressure in the clinical setting.
Similar content being viewed by others
Introduction
Excessive salt intake is an established risk factor for hypertension [1]. Clinical studies have reported that salt restriction lowers the threshold for salty taste [2, 3]. In an epidemiological study in a Japanese rural population, impaired taste of salt was associated with a high prevalence of hypertension based on blood pressure measurements taken at health check-ups [4].
Home blood pressure (HBP) measurement has been shown to have a stronger predictive power for mortality than blood pressure measurements taken at health check-ups in the Japanese general population [5]. Furthermore, HBP measurement is useful to detect masked hypertension among individuals defined as normotensive based on clinical measurement [6]. Ohkubo et al. [7]. reported that the composite risk of cardiovascular mortality and stroke morbidity was high in subjects with masked hypertension, as well as in those with sustained hypertension. It is important to obtain evidence on lifestyle factors and masked hypertension. However, to our knowledge, there is no community-based study examining the association between impaired taste of salt and masked hypertension. Thus, we conducted this cross-sectional study involving an urban Japanese population with no reported hypertension or anti-hypertensive medication in the clinical setting.
Materials and methods
Study participants
The KOBE study is a population-based cohort study on the risk factors for worsening quality of life or cardiovascular disease, such as hypertension, diabetes mellitus, and dyslipidemia [8,9,10]. The study participants were healthy community residents of Kobe City, one of the major urban areas in Japan, between 40 and 74 years of age. The participants were recruited by the public relations office of the Kobe municipal government through advertisements in magazines, newspapers, posters, and leaflets distributed among public facilities. The inclusion criteria were as follows: (1) no current medication for dyslipidemia, hypertension, or diabetes mellitus, and (2) no history of cardiovascular disease or cancer. A total of 1117 individuals participated in the baseline survey conducted between July 2010 and December 2011 at the Institute of Biomedical Research and Innovation. We performed a cross-sectional analysis by using the baseline data from an examination of a prospective cohort study (KOBE study). We excluded 225 subjects for the following reasons: missing data (n = 1), hypertension ( ≥ 140/90 mm Hg) diagnosed on the basis of measurement at the time of the baseline survey (n = 137), and failure to measure HBP appropriately in the required manner for 5 days or more (n = 87). Finally, 892 individuals (246 men and 646 women) were included in the present study.
Written informed consent was obtained from each participant. The present study was approved by the ethics committee of the Institute of Biomedical Research and Innovation (Approval number 10-02).
Data collection
At the baseline survey, the participants were asked to respond to questionnaires about smoking and alcohol consumption over the preceding month. Research physicians, nurses, and nutritionists then performed face-to-face interviews with each participant and reviewed their answers to the questionnaire questions.
After a 5 min resting period, blood pressure was measured twice, consecutively, in each participant using an automatic sphygmomanometer (BP-103i II; Nihon Colin, Tokyo, Japan), and the mean value was recorded. Height and weight were measured using combined equipment (U-WELL2; Elk Corp., Osaka, Japan), while wearing socks and light clothing. Body mass index (BMI) was calculated as the weight (kg) divided by the height squared (m2). Waist circumference was measured at the umbilical level in the standing position.
Blood samples were collected after the participants had fasted for at least 10 h and were tested in the same commissioned clinical laboratory center (SRL Inc., Tokyo, Japan). The levels of serum total cholesterol, high-density lipoprotein cholesterol, and triglycerides were measured by enzymatic methods. The low-density lipoprotein cholesterol levels were estimated using the Friedewald formula [11]. Estimation of glomerular filtration rate (eGFR) was calculated by the Japanese equation using serum creatinine [12] for evaluating kidney function.
Assessment of salty taste recognition and salt intake
Salty taste recognition was assessed by a salt-impregnated taste strip (Salsave; Advantech Toyo Co., Tokyo, Japan). This method was developed by Maruyama et al. [13,14,15] and validated by Nishimoto et al. [16]. Nishimoto et al. [16] compared the Salsave test with other taste tests such as the whole-mouth method, the micropipette salty taste quantity test, and the electric taste threshold; the results of the Salsave test correlated significantly with the results of the other taste tests [16]. The strips were impregnated with sodium chloride in concentrations of 0, 0.6, 0.8, 1.0, 1.2, 1.4, and 1.6%. We assessed salty taste recognition using the modified version described by Michikawa et al. [4]. First, the participants were asked to rinse their mouths with fresh water to neutralize their oral conditions as much as possible. Next, they were asked to place a strip impregnated with 0% sodium chloride on their tongue for 3 s to familiarize themselves with the taste of the blank strip. Then they sequentially tasted the remaining taste strips in the same way, beginning with the lowest concentration of sodium chloride. Participants were asked to report and describe any taste perceived. The concentration at which they identified the salt taste was defined as the salty taste recognition threshold.
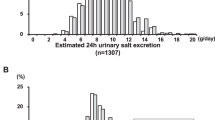
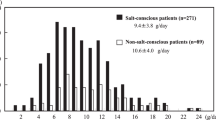
Daily salt and potassium intakes were evaluated by estimating the 24 h urinary sodium chloride and potassium excretion using spot urine, and were calculated by the equation developed by Tanaka et al. [17].
Measurement of HBP
Participants with clinical systolic/diastolic blood pressures below 140/90 mm Hg at the baseline survey were asked to perform HBP measurements using an Omron HEM-747IC device (Omron Healthcare, Kyoto, Japan). They received written and oral instructions from the research staff on how to perform the measurements, based on the 2009 Japanese Society for Hypertension guidelines for the management of hypertension [18]. The participants were asked to measure HBP immediately after awakening and before bedtime, for 1 week. The participants measured their blood pressure in the sitting position on two consecutive occasions after resting for at least 2 min. Blood pressure measurements in the morning were taken (1) after voiding and (2) before breakfast. We analyzed data including blood pressure measurements completed in the morning and evening for 5 days or more. The mean values of all measurements were used for the analyses.
Statistical analysis
The participants were classified into three groups according to the salty taste recognition threshold (0.6, 0.8, and ≥ 1.0%) and stratified by sex. Data are presented as the means ± SDs for continuous variables and as percentages for categorical variables. Non-normal variables are presented as the median values and range (minimum–maximum values). Differences in continuous variables were tested using analysis of variance (ANOVA) or the Kruskal–Wallis test. The Bonferroni-corrected χ2-test was used for categorical variables. According to the 2014 guidelines for the management of hypertension [6], each HBP value was classified into normal blood pressure ( < 125/75 mm Hg), normal high blood pressure (125–134/75–84 mm Hg), or hypertension ( ≥ 135/85 mm Hg). Logistic regression analyses were performed to estimate the age- and multivariate-adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for masked hypertension between the groups of salty taste recognition threshold, with the group of 0.6% set as the reference. The differences were evaluated after adjusting for age, BMI, smoking status (never-, former-, and current smokers) and ethanol intake (never, former ≤ 22, 23–45, and ≥ 46 g/day). Similar analyses for non-normal HBP ( ≥ 125/75 mm Hg) were also performed.
All p-values were two-sided, with p < 0.05 considered statistically significant. All statistical analyses were performed using SPSS 22.0 J for Windows (SPSS Inc., Tokyo, Japan).
Results
Among all participants stratified by sex, the proportions of subjects with salty taste recognition thresholds of 0.6, 0.8, and ≥ 1.0% were 69.5%, 16.7%, and 13.8%, respectively, in men, and 83.6%, 9.4%, and 7.0%, respectively, in women. The proportions of high normal blood pressure (125–134/75–84 mm Hg) based on HBP were 35.0% in men and 20.3% in women. The proportions of masked hypertension ( ≥ 135/85 mm Hg) were 13.8% in men and 6.5% in women.
Table 1 shows the participant characteristics according to the salty taste threshold and by sex. In men, the proportion of current smokers was significantly higher in the ≥ 1.0% salty taste threshold group than in the 0.6% group. The proportion of current drinkers ( ≥ 23 g ethanol/day) was also significantly higher in the 0.8% and ≥ 1.0% groups than in the 0.6% group. There was no significant difference in serum creatinine levels and eGFR levels among the three groups of different salty taste recognition threshold in both men and women. In women, no significant difference was observed in the clinical measures among the three groups related to the salty taste threshold.
Table 2 shows the HBP characteristics according to the salty taste threshold by sex. In men, there was no significant difference in the mean HBP values between the groups. In women, the mean systolic blood pressure in the evening for the ≥ 1.0% salty threshold group was significantly higher than that in the 0.8% group. In men, the proportions of those with non-normal HBP ( ≥ 125/75 mm Hg) and masked hypertension ( ≥ 135/85 mm Hg) were the highest in the 0.8% group. In women, the proportions of those with non-normal HBP ( ≥ 125/75 mm Hg) tended to increase with increases in salty taste threshold. The proportion of those with masked hypertension ( ≥ 135/85 mm Hg) in women was significantly higher in the ≥ 1.0% group than in the 0.6% group.
The ORs and 95% CIs for non-normal HBP and masked hypertension in relation to the salty taste threshold by sex are shown in Table 3. In men, the age-adjusted OR for non-normal HBP ( ≥ 125/75 mm Hg) was significantly higher in the 0.8% salty taste threshold group than in the 0.6% group. However, this association was not significant after adjusting for BMI, smoking, and drinking status. In women, the ORs for masked hypertension ( ≥ 135/85 mm Hg) were significantly higher in the ≥ 1.0% group than in the 0.6% group in both the age-adjusted and multivariate analyses. The multivariate OR for masked hypertension was 2.98 (95% CI: 1.16–7.64).
Discussion
Although it increases the risk of stroke, most individuals are generally unaware of masked hypertension [7]. Herein, we examined the association of salty taste recognition with masked hypertension. Impaired salty taste recognition was found to be associated with masked hypertension based on HBP measurement in women, but not in men. Michikawa et al. [4]. also reported that impaired salty taste recognition was associated with hypertension based on blood pressure measurements at health check-ups in women. Sub-analysis of the data of 77 married couples suggested that impairment of salty taste recognition in women was associated not only with their hypertension but also with hypertension of their husbands [4]. The researchers considered that salt intake among their husbands and family members may depend on the women’s salty taste preference, as most family meals in Japan across this age group are prepared by women. Our findings were comparable to the findings by Michikawa et al. [4] and the association was observed even at the stage of masked hypertension. Confounding by smoking is another possible reason for the lack of association between impaired salty taste recognition and masked hypertension in men. Cigarette smokers exhibited lower taste sensitivity than non-smokers in previous studies [19, 20], although it has not been confirmed whether and how smoking habits affect blood pressure [6]. In our study, current smoking was significantly associated with impaired salty taste recognition (Table 1) but not with masked hypertension in men. In men, the association between impaired salty taste recognition and masked hypertension may be attenuated due to the high percentage of current smokers in the ≥ 1.0% salty taste threshold group.
Long-term adherence to a low-sodium diet has been reported to improve the threshold for salty taste in clinical studies [21], and a high threshold of salty taste reflects salty taste preference and, therefore, habitual high salt intake [22]. In normotensive adults adhering to a low-sodium diet for 1 year, the mean preferred salt concentrations declined from 0.72% to 0.33% after 3 months of sodium restriction [21]. Conversely, in another study in which healthy university students participated in a diet intervention trial (ad libitum salt intake for 3 weeks [pre-diet], followed by 12 g of crystalline salt added to food daily for 4 weeks [high salt], followed by ad libitum salt intake for 3 weeks [post-diet]), the mean preferred concentrations of salt increased by 0.09 mol/L compared with that at the beginning of the trial [22].
There are few studies clarifying the association between habitual salt intake and blood pressure [23,24,25]. Bursztyn et al. [23] estimated the salt-sensitivity risk by a combination of 10% or less mean arterial pressure reduction during sleep and 24 h heart rate at least 70 bpm during 24 h ambulatory blood pressure monitoring, and reported that the prevalence of high salt-sensitivity was higher in women than in men [23, 24]. According to the Dietary Approaches to Stop Hypertension-Sodium Trial, the effect of lower sodium intake on blood pressure was more pronounced in women than in men [25]. It is a reasonable method to estimate daily salt intake by using spot urine, and the estimated daily salt intake correlated with salt-intake behaviors in previous studies [26, 27]. In the present study, no association was found between estimated daily salt intake and the salty taste recognition threshold. The estimated daily salt intake calculated by a urine sample might reflect salt intake behavior for a short period. When individual salt intake behavior has been recently modified, the threshold for salty taste may not be improved immediately, as found in previous clinical studies using normotensive participants [21, 22]. In Japan, from the 1960s, community-based hypertension control programs have been established in order to prevent stroke [28, 29], and health education for reducing salt intake has been implemented. All participants in the present study had normal blood pressure at the baseline clinical measurements; however, there is the potential for reducing salt intake in people concerned with increases in blood pressure within the normal range. If behavior modification occurred recently among some participants, the associations between estimated daily salt intake with salty taste recognition threshold and the HBP level could be attenuated or disappear. However, further prospective studies are needed to confirm this speculation.
Taste acuity including salty taste is impaired in kidney disease patients with hemodialysis or continuous ambulatory peritoneal dialysis [30, 31]. However, there was no significant difference in serum creatinine and eGFR levels among the three groups of different salty taste recognition threshold in both men and women. Thus, renal function is not directly related to salty taste recognition in our apparently healthy population.
The present study has several limitations. First, daily salt intake was estimated using single spot urine. It has been shown that both estimations using spot and 24 h urine show intra-individual variability at the individual level [32]. The accuracy of our analysis may be improved by expanding the sample size, by collecting multiple spot urine samples, or by 24 h urine collection. Second, we could not collect detailed information on dietary habits, such as vegetable intake, which affect blood pressure mainly through potassium intake, although we assessed estimated potassium intake by spot urine samples. Third, the association between salty taste recognition and masked hypertension may be potentially attenuated due to the cross-sectional study design, as individuals with high blood pressure make an effort to decrease their blood pressure by lifestyle modification, such as salt intake reduction. We did not examine recent modifications in salt intake among individual participants. Accordingly, our findings should be verified by prospective studies.
In conclusion, impairment of salty taste recognition was associated with masked hypertension in women. Preference for light salty taste should be recommended for the prevention of masked hypertension. Further prospective cohort studies are needed to corroborate this hypothesis.
References
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. BMJ. 1988;297:319–28.
Mattes RD. The taste for salt in humans. Am J Clin Nutr. 1997;65(2 Suppl):692S–697S.
Kusaba T, Mori Y, Masami O, Hiroko N, Adachi T, Sugishita C et al. Sodium restriction improves the gustatory threshold for salty taste in patients with chronic kidney disease. Kidney Int. 2009;76:638–43.
Michikawa T, Nishiwaki Y, Okamura T, Asakura K, Nakano M, Takebayashi T. The taste of salt measured by a simple test and blood pressure in Japanese women and men. Hypertens Res. 2009;32:399–403.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–15.
Higashiyama A, Wakabayashi I, Kubota Y, Adachi Y, Hayashibe A, Nishimura K et al. Does high-sensitivity C-reactive protein or low-density lipoprotein cholesterol show a stronger relationship with the cardio-ankle vascular index in healthy community dwellers?: the KOBE study. J Atheroscler Thromb. 2014;19:1027–34.
Kubota Y, Higashiyama A, Imano H, Sugiyama D, Kawamura K, Kadota A et al. Serum polyunsaturated fatty acid composition and serum high-sensitivity C-reactive protein levels in healthy Japanese residents: The KOBE Study. J Nutr Health Aging. 2015;19:719–28.
Kuwabara K, Harada S, Sugiyama D, Kurihara A, Kubota Y, Higashiyama A et al. Relationship between non-high-density lipoprotein cholesterol and low-density lipoprotein cholesterol in the general population. J Atheroscler Thromb. 2016;23:477–90.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K et al. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Maruyama C, Nakamori T, Nakanishi Y, Hayashida M, Fukushima S. Development and study of salt taste sensitivity test for evaluation of diet therapy. Jpn J Nutr. 1988;46:211–6.
Maruyama C, Murata M, Tomiyama J, Kumamoto E, Matsuo S, Nunokawa N et al. Study of salty taste in healthy subjects and hypertensive patients (First report). Jpn J Nutr. 1990;48:121–6.
Maruyama C, Amagai K, Higashi C, Matsuzawa M, Okuwaki I, Kichimi C et al. A study of salt taste in healthy subjects and patients with hypertension (Second report). Jpn J Nutr. 1990;48:267–71.
Nishimoto K, Hirota R, Egawa M, Furuta S. Clinical evaluation of taste dysfunction using a salt-impregnated taste strip. ORL J Otorhinolaryngol Relat Spec. 1996;58:258–61.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension 2009. Hypertens Res. 2009;32:3–107.
Chéruel F, Jarlier M, Sancho-Garnier H. Effect of cigarette smoke on gustatory sensitivity, evaluation of the deficit and of the recovery time-course after smoking cessation. Tob Induc Dis. 2017;15:15. 10.1186/s12971-017-0120-4. eCollection 2017
Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. J Neurol. 2008;255:1121–6.
Blais CA, Pangborn RM, Borhani NO, Ferrell MF, Prineas RJ, Laing B. Effect of dietary sodium restriction on taste responses to sodium chloride: a longitudinal study. Am J Clin Nutr. 1986;44:232–43.
Bertino M, Beauchamp GK, Engelman K. Increasing dietary salt alters salt taste preference. Physiol Behav. 1986;38:203–13.
Bursztyn M, Ben-Dov IZ. Sex differences in salt-sensitivity risk approximated from ambulatory blood pressure monitoring and mortality. J Hypertens. 2013;31:900–5.
Castiglioni P, Parati G, Brambilla L, Brambilla V, Gualerzi M, Di Rienzo M et al. Detecting sodium-sensitivity in hypertensive patients: information from 24-hour ambulatory blood pressure monitoring. Hypertension. 2011;57:180–5.
Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, et al. DASH-Sodium Trial Collaborative Research Group. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135:1019–28.
Ohta Y, Iwayama K, Suzuki H, Sakata S, Hayashi S, Iwashima Y et al. Salt intake and eating habits of school-aged children. Hypertens Res. 2016;39:812–7.
Uechi K, Asakura K, Masayasu S, Sasaki S. Within-country variation of salt intake assessed via urinary excretion in Japan: a multilevel analysis in all 47 prefectures. Hypertens Res. 2017;40:598–605.
Shimamoto T, Komachi Y, Inada H, Doi M, Iso H, Sato S et al. Trends for coronary heart disease and stroke and their risk factors in Japan. Circulation. 1989;79:503–15.
Yokota K, Harada M, Wakabayashi Y, Inagawa M, Oshima M, Toriumi S et al. Evaluation of a community-based health education program for salt reduction through media campaigns. Nihon Koshu Eisei Zasshi. 2006;53:543–53. (Article in Japanese)
Burge JC, Park HS, Whitlock CP, Schemmel RA. Taste acuity in patients undergoing long-term hemodialysis. Kidney Int. 1979;15:49–53.
Fernström A, Hylander B, Rössner S. Taste acuity in patients with chronic renal failure. Clin Nephrol. 1996;45:169–74.
Brown IJ, Dyer AR, Chan Q, Cogswell ME, Ueshima H, Stamler J et al., INTERSALT Co-Operative Research Group. Estimating 24-hour urinary sodium excretion from casual urinary sodium concentrations in Western populations: the INTERSALT study. Am J Epidemiol. 2013;177:1180–92.
Acknowledgements
This study was supported by grants from the Regional Innovation Cluster Program, Global Type, Ministry of Education, Culture, Sports, Science and Technology, by grants-in-aid for scientific research (C) 24590844 and (B) 23390178, and for Young Scientists (B) 15K19232 from the Japan society for the promotion of science, and by a grant-in-aid from the Ministry of Health, Labour and Welfare, Comprehensive Research on Cardiovascular and Life-Style Related Disease: H29-Junkankitou-Ippan-003. We thank Dr. Kazuyo Kuwabara, Dr. Yukako Tatsumi, Dr. Hironori Imano, Dr. Kunihiro Nishimura, Dr. Tomofumi Nishikawa, and other research staff members for their professional assistance in conducting KOBE study. We also thank all the volunteers who participated in the KOBE study, Center for Cluster Development and Coordination, and the Kobe municipal government for supporting the survey.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kubota, Y., Higashiyama, A., Sugiyama, D. et al. Association between impairment of salty taste recognition and masked hypertension based on home blood pressure in Japanese residents: the KOBE study. Hypertens Res 41, 756–762 (2018). https://doi.org/10.1038/s41440-018-0074-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0074-9
This article is cited by
-
Umami and salt reduction
Hypertension Research (2020)
-
Validation of preferred salt concentration in soup based on a randomized blinded experiment in multiple regions in Japan—influence of umami (l-glutamate) on saltiness and palatability of low-salt solutions
Hypertension Research (2020)
-
Quantitative verification of the effect of using an umami substance (L-glutamate) to reduce salt intake
Hypertension Research (2020)