Abstract
While home blood pressure (BP) measurement is recommended for hypertension management, the clinical implications of peak home BP values have not been well studied. This study investigated the association between pathological threshold or frequency of peak home BP and cardiovascular events in patients with ≥1 cardiovascular risk factor. The Japan Morning Surge-Home Blood Pressure (J-HOP) study enrolled participants from 2005–2012 with extended follow-up from December 2017 to May 2018, which generated the dataset for this analysis. Average peak home systolic BP (SBP) was defined as average of the highest three BP values on 14-day measurement period. Patients were divided into quintiles of peak home BP, and the risk of stroke, coronary artery disease (CAD) and atherosclerotic cardiovascular disease (ASCVD; stroke+CAD) was determined. In 4231 patients (mean 65 years) followed for 6.2 years there were 94 strokes and 124 CAD events. The adjusted hazard ratio (HR) (95% CI) for the risk of stroke and ASCVD in patients with average peak home SBP in the highest versus lowest quintile was 4.39 (1.85–10.43) and 2.04 (1.24–3.36), respectively. Risk was greatest for stroke in the first 5 years: HR 22.66 (2.98–172.1). The pathological threshold of average peak home SBP for 5-year stroke risk was 176 mmHg. There was a linear association between the number of times peak home SBP > 175 mmHg and stroke risk. Peak home BP was a strong risk factor for stroke, especially within the first 5 years. We propose exaggerated peak home SBP > 175 mmHg as an early and strong novel risk factor for stroke.

Similar content being viewed by others
Introduction
There is a good body of evidence supporting the fact that home blood pressure (BP) is more closely associated with hypertensive organ damage and future cardiovascular events in patients with hypertension than office BP [1,2,3,4,5,6,7]. In addition, key hypertension guidelines recommend the measurement of home BP to facilitate the diagnosis and management of hypertension [8,9,10,11,12,13]. Home BP measurements became increasingly important during the COVID-19 pandemic, when patients were unable to attend in-person clinic visits, and are an essential component of new digital hypertension strategies [14,15,16,17,18,19,20].
With respect to home BP measurements, the diagnosis of hypertension and target threshold for home BP are based on the average of home BP readings [8,9,10,11,12,13], and average home BP is a well-established cardiovascular risk factor in both community- and clinic-based cohorts [1, 2, 5, 21,22,23,24,25]. In contrast, the clinical implications of peak home BP have not been well studied. In fact, in clinical practice, a single high peak home BP measurement over a measurement period of a few weeks might be excluded as an outlier.
A previous analysis of data from the general practitioner-based nationwide Japan Morning Surge-Home Blood Pressure (J-HOP) study, a prospective, observational study of outpatients with a history of or risk factors for cardiovascular disease, found that maximum mean home systolic BP (SBP), defined as the maximum mean value of three BP readings over a 14-day home BP monitoring period, was significantly associated with organ damage (left ventricular mass index, carotid intima media thickness and urinary albumin-to-creatinine ratio) and future stroke events [26,27,28]. These associations were independent of other measures of home BP variability such as coefficient of variation (CV) and average real variability (ARV). However, these analyses were limited by a comparatively short follow-up duration, whereas longer-term prospective data are needed to clarify the clinical implications of different definitions of peak home BP in patients with hypertension.
This analysis used data from a longer-term follow-up of patients enrolled in the J-HOP study (extended from 3.9 years to 6.2 years) to investigate associations between peak home BP (using different definitions, and based on pathological thresholds, frequency of exaggerated peak home BP, and duration of risk) and the risk of stroke events.
Methods
Study design
The multicenter, prospective, observational J-HOP study (University Hospital Medical Information Network Clinical Trials Registry, UMIN000000894) enrolled participants from 2005 to 2012, with follow-up through to March 2015 [1]. Seventy-five physicians from 71 institutions enrolled patients into the study (see online-only Data Supplement for full details). An extended follow-up survey to reconfirm the clinical outcomes was performed from December 2017 to May 2018, and generated the final dataset for the present analysis. The study protocol was approved by the Institutional Review Board of Jichi Medical University School of Medicine, Tochigi, Japan. Written informed consent was obtained from all patients.
Study population
Participants were ambulatory outpatients who had at least one of the following cardiovascular risk factors: hypertension; hyperlipidemia; diabetes (fasting blood sugar ≥126 mg/dL or treatment with antidiabetic agents); glucose intolerance; metabolic syndrome; chronic kidney disease (estimated glomerular filtration rate <60 mL/min/1.73 m2); history of cardiovascular disease (including coronary artery disease [CAD], stroke, aortic dissection, peripheral artery disease, congestive heart failure); atrial fibrillation; current smoking; chronic obstructive pulmonary disease; and/or sleep apnea syndrome (see online-only Data Supplement for full details).
Outcomes
Cardiovascular disease outcomes included fatal or nonfatal stroke, fatal or nonfatal CAD, and fatal or nonfatal atherosclerotic cardiovascular disease (ASCVD; the combination of stroke and CAD). Full definitions of each type of event have been reported previously [1] and are provided in the online-only Data Supplement.
Assessments
Home BP measurements were performed using a validated cuff oscillometric device (HEM-5001; Medinote; Omron Healthcare, Co., Ltd) in accordance with hypertension guidelines that were current at the time assessments were performed [29]. The device automatically takes three separate measurements of BP at 15-second intervals for each assessment. All recorded BP parameters are stored in the device memory, with identification of measurements as morning, evening or during sleep. Home BP values were recorded over a period of 14 days. Subjects were asked to measure morning BP within 1 h of waking, after urination, before breakfast and before taking antihypertensive medication. Evening BP was measured before going to bed, and the patients were instructed to avoid measuring their BP just after taking a bath, drinking alcohol or smoking. Morning and evening BP data stored on each device were downloaded to a computer by a physician or nurse during clinic visits. These data were then sent to the study control center (Jichi Medical University, Tochigi, Japan). After exclusion of the data from the first day, the averages of all home BP measurements taken three times in the morning (morning home BP) and three times in the evening (evening home BP) for 13 days (78 readings in total) were calculated by the study coordinator who was blinded to the clinical characteristics of study participants. Details of clinic BP measurements and determination of laboratory and other parameters are provided in the online-only Data Supplement.
Data on cardiovascular outcomes were obtained from a general physician at each study center. Incident stroke and CAD outcomes were also ascertained by regular (annual or more frequent) review of participants’ medical records. When patients did not come to the hospital, they or their family members were interviewed by telephone. All endpoint events were adjudicated by an endpoint committee who were unaware of individual clinical characteristics, including home BP data.
Definitions of peak home BP
The average peak home SBP was defined as the average of the highest three BP values for each individual over the 13-day home BP assessment period. Maximum mean home SBP was defined as the highest value of mean home BP on one occasion (average of three consecutive measurements), and maximum home SBP was defined as the highest of all home BP values measured.
Patient groups
The rate of outcome events was determined in patient subgroups defined based on quintiles of home BP (average peak, maximum mean home, and maximum home, as described above).
Statistical analyses
Descriptive statistics are presented as mean ± standard deviation, or number and proportion. A one-way analysis of variance was performed to detect between-group differences in mean values, and the Chi-squared test or Fisher’s exact test was used to detect differences in prevalence rates between groups.
The Kaplan-Meier cumulative incidence of stroke events in each BP quintile group was calculated. Using Cox proportional hazards models, hazard ratio (HR) and 95% confidence interval (CI) values were calculated for ASCVD, stroke or CAD events based on the average peak SBP value or the average of morning and evening (MEave) home SBP value with adjustment for the following: baseline demographic (age and sex) and clinical characteristics (body mass index, smoking status); presence of diabetes; preexisting angina pectoris, myocardial infarction or stroke; total cholesterol to high-density lipoprotein cholesterol ratio; use of antihypertensives, statins, and aspirin); and office SBP.
To identify multicollinearity, the variation inflation factor was assessed. Variation inflation factor values of >5 were considered to indicate multicollinearity. Using a spline regression analysis, cut-off values for average peak home BP and MEave home BP were determined for the occurrence of incident stroke events. Heat maps were used to visually represent the associations between average peak home SBP and MEave home SBP quintile groups and the occurrence of stroke events.
All statistical analyses were performed with SAS system, v9.4 (SAS Institute, Cary, NC). Two-sided P values < 0.05 were defined as statistically significant.
Results
Participants
Of the 4310 patients enrolled in the J-HOP study, 32 were lost to follow-up, 17 had missing data for B-type natriuretic peptide or urine albumin-to-creatinine ratio, and 30 had missing home BP readings (Supplementary Fig. 1), leaving 4231 patients (mean age 64.9 ± 10.9 years, 46.7% male, 79% taking antihypertensive medication) for inclusion in the current analysis (Table 1). Baseline patient characteristics in subgroups based on quintile of average peak home SBP and MEave home SBP are shown in Supplementary Table 1. There were significant differences in BMI (p < 0.001), chronic kidney disease (p = 0.009), HDL cholesterol (p < 0.001) and all BP values (p < 0.05) between group of average peak upper quintile but not MEave upper quintile and group of not average peak upper quintile but MEave upper quintile.
BP measurements
Patients were instructed to take BP measurements three times in the morning and three times in the evening for 13 days (total 78 measurements), but the average number of actual measurements was 69 ± 14. A total of 293,509 home BP readings were included in this analysis. Of all home BP values recorded, the highest three home BP values occurred as the first of the three consecutive measurements for nearly half (49%) of all measurements, in the second measurement on 33% of occasions and in the third measurement in 18% of occasions. Average peak home SBP was a morning recording in 65% of cases and an evening recording in 35%.
Stroke risk
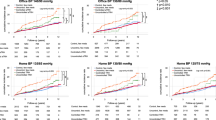
During a mean follow-up of 6.2 ± 3.8 years (26,205 person-years) there were 218 ASCVD events (94 strokes and 124 CAD). During the first 5 years, patients with average peak home SBP based on morning and evening values in the highest quintile (Q5; ≥173.0 mmHg) were at higher risk of experiencing a stroke than those with average peak home SBP in all other quartiles, and patients with average peak home SBP in the lowest quartile (Q1; <142.7 mmHg) had very few stroke events (Fig. 1). Findings were consistent when looking at average peak home SBP based on only morning or only evening readings (Fig. 1), and when data were stratified based on patient age (<65 vs. ≥65 years) and the presence versus absence of a history of ASCVD (Fig. 2). From 5 years onwards, cumulative stroke incidence rates for patients with average peak home SBP in quartile 4 (Q4) began to approach those of patients with average peak home SBP in Q5 (Fig. 1). CAD risk was not related to quintiles of average peak home SBP (data not shown).
Cumulative incidence of stroke events by average peak home systolic blood pressure quintile (mean follow-up 6.2 ± 3.8 years; 26,205 person-years). Average peak home systolic blood pressure was calculated using both morning and evening home systolic blood pressure values (A), only morning home systolic blood pressure values (B), and only evening home systolic blood pressure values (C). Q indicates quartile; SBP systolic blood pressure
Cumulative incidence of stroke events by average peak home systolic blood pressure quintile, stratified by age or history of atherosclerotic cardiovascular disease. Average peak home systolic blood pressure was calculated using both morning and evening home systolic blood pressure values. ASCVD indicates atherosclerotic cardiovascular events (stroke and coronary artery disease); Q quartile, SBP systolic blood pressure
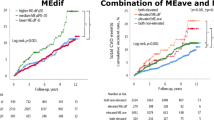
Compared to patients with average peak home SBP in Q1, the adjusted risk of ASCVD and of stroke alone over the first 5 years and the whole follow-up period was significantly increased in patients with average peak home SBP in Q4 and Q5. When MEave home SBP were used instead of peak average home SBP, only the risk of stroke was significantly higher in patients with MEave home SBP in Q5 versus Q1 (Table 2). The similar results were found when average peak home SBP was based morning home SBP, but the event risk was not related to quintiles of average peak evening home SBP and evening home SBP (Supplementary Table 2 and 3). The same results as in Table 2 were found after additional adjustment for the CV and ARV of home SBP MEave (Supplementary Table 4), when average peak home SBP was based only on the first and second measurements on one occasion (Supplementary Table 5), and when average peak home SBP was based only on the second and third measurements on one occasion (Supplementary Table 6), and when maximum mean home SBP (Supplementary Table 7) or a single maximum home SBP reading (Supplementary Table 8) were used instead of peak average home SBP.
Spline regression analysis identified an average peak home SBP cut-off value for incident stroke of 176 mmHg in the first 5 years and 163 mmHg over the whole follow-up period (Fig. 3). In addition, average peak home SBP only had to exceed these thresholds once for the risk of stroke to increase, and stroke risk increased substantially as the number of times the threshold value specified from the average peak home SBP increased (Fig. 4).
Spline regression analysis of the relationship between average peak home systolic blood pressure and incident stroke risk. Mean values and 95% confidence interval are shown. Data were adjusted for age, sex, body mass index, current smoking, history of diabetes, statin use, aspirin use, antihypertensive medication use, history of cardiovascular disease, total cholesterol to high-density lipoprotein cholesterol ratio, and office systolic blood pressure. Average peak home systolic blood pressure was calculated using both morning and evening home systolic blood pressure values. SBP indicates systolic blood pressure
Spline regression analysis of the relationship between the number of times peak home systolic blood pressure exceeded 165 mmHg or 175 mmHg and incident stroke risk. Mean values and 95% confidence interval are shown. Data were adjusted for age, sex, body mass index, current smoking, history of diabetes, statin use, aspirin use, antihypertensive medication use, history of cardiovascular disease, total cholesterol to high-density lipoprotein cholesterol ratio, and office systolic blood pressure. Average peak home systolic blood pressure was calculated using both morning and evening home systolic blood pressure values. SBP indicates systolic blood pressure
Heat map of stroke risk by quintiles of average peak home SBP showed that stroke risk increased as average peak home SBP increased across all MEave home SBP groups (Fig. 5).
Heat map of stroke event (95% confidence interval) by average peak home systolic blood pressure quintile and average of morning and evening home systolic blood pressure quintile. Average peak home systolic blood pressure was calculated using both morning and evening home systolic blood pressure values. MEave indicates morning-evening average; Q quartile, SBP systolic blood pressure
Discussion
This analysis of the general practitioner-based nationwide J-HOP study showed that average peak home SBP (defined as the average of the top three BP values for each individual) was an early and strong predictor of stroke risk in patients with hypertension and at least one cardiovascular risk factor. The pathological threshold was 176 mmHg, and the more times that peak home SBP exceeded this threshold, the higher the risk of stroke. The stroke risk associated with peak home SBP was independent of other home BP variability measures such as CV and ARV, and the heat maps show that stroke risk was higher in patients with peak home SBP in higher versus lower quintiles across all quintiles of MEave home SBP. This suggests that peak home BP, as well as average home BP, should be taken into account when evaluating stroke risk in clinical practice.
The association between average peak home SBP and stroke risk was seen early, and was strongest in the first 5 years of follow-up. In addition, findings were consistent when peak home SBP was determined using all morning and evening home BP data (Fig. 1A), and only morning or only evening home BP values (Fig. 1B, C). The adjusted HR for stroke risk in patients with average peak home SBP in the highest quintile (Q5; ≥173.0 mmHg) compared with the lowest quintile (Q1) was 4.39 over the entire follow-up period and 22.7 over the first 5 years. We also found that the risk of stroke for patients with peak home SBP in Q4 increased from 5 years onwards to be similar to that in patients with peak home SBP in Q5. This differential impact of the average peak home SBP over shorter and longer follow-up durations is a novel finding of the current study, and could not be determined in previous J-HOP studies with a shorter follow-up (mean 3.9 years) [1, 30].
In addition to the linear association between the frequency of exaggerated peak home SBP and stroke risk, an average peak home SBP of >163 mmHg significantly increase stroke risk throughout the follow-up period. The lowest risk appeared to be when average peak SBP was <145 mmHg (Fig. 3, right). This suggests that consistently having an average peak home SBP below 145 mmHg should be almost free of stroke risk. However, the pathological peak home BP thresholds identified in this study will need to be evaluated in different patient cohorts to allow definitive conclusions to be drawn.
The risk of stroke associated with elevated peak home SBP was consistent across three different definitions (average of the top three BP values for each individual in a 13-day period [average peak home SBP], highest value of the average of three consecutive home SBP measurements on one occasion [maximum mean home SBP]), and the highest value of all home BPs measured [peak home SBP]). We also defined peak home BP based on the recommended measurement schedule for home BP (i.e. twice in the morning and twice in the evening) [8,9,10,11,12,13], and the findings were essentially the same. In addition, the impact of peak home SBP on stroke risk was similar when both morning and evening measurements were taken into account, or when only morning or only evening measurements were used. Although the definition of peak home BP did not alter the association with stroke risk in this study, there is still a need to agree a precise definition for this important parameter for use in future trials and guideline documents.
Another key finding of this study was that the early and strong association between average peak home BP and stroke events was independent of other measures of home BP variability (Supplementary Table 4). In current hypertension management guidelines, the definition of hypertension and target BP is based on the average of office, home, and ambulatory BPs [10,11,12,13], the accuracy of which increases as the number of BP measurements increases. However, BP variability is another measure that needs to be taken into account. There is growing evidence that increased variability in office, home, and ambulatory BP values increases the risk of cardiovascular events independently of the averaged BP values [30,31,32,33]. The CV and ARV are well-known indicators of BP variability. In a previous analysis of J-HOP study data, CV and ARV of home BP measurements were associated with stroke risk independently of the average home BP [30]. In the current analysis, a model that included the CV and ARV of home BP readings showed that average peak home SBP remained a strong predictor of stroke risk in the first 5 years of follow-up (HR for average peak home SBP in Q5 vs Q1 of 16.8). Thus, average peak home SBP could provide additional prognostic information, over and above that of BP variability measures. Despite the important contribution of BP variability to cardiovascular risk, no hypertension management guidelines have yet described how to incorporate the assessment of BP variability into clinical practice. This is also the case for peak home BP.
Strengths and limitations
The J-HOP study includes an elderly Japanese cohort with at least one cardiovascular risk factor. Therefore, our novel finding that average peak home BP is associated with increased stroke risk need to be replicated in other populations, including a community-dwelling sample, normotensive individuals, younger people, and different ethnic groups. In addition, because this is an observational study it is not possible to definitively state causality for the identified associations. It is also important to note that nearly 80% of the J-HOP study population were receiving antihypertensive drug therapy, and therefore there is potential for the relationships identified in the current study to have been modified by the presence of pharmacological antihypertensive agents. All home BP measurements taken during this study were taken when patients were in a sitting position, which may underestimate the risk of BP surge. Use of wearable BP monitoring devices could measure several peak BP values under different conditions throughout each day [34], and therefore may increase the sensitivity of peak home BP measurements for determining cardiovascular risk. This needs to be investigated in future studies.
Conclusions
This analysis identified for the first time an early and strong association between average peak home BP and stroke risk. The simplicity of this measurement and the ease with which it can be determined using home BP monitoring make it ideally suited for evaluation of stroke risk in clinical practice.
References
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan morning surge-home blood pressure study. Hypertension. 2016;68:54–61.
Kario K, Saito I, Kushiro T, Teramukai S, Ishikawa Y, Mori Y, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–96.
Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, et al. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST study. J Am Coll Cardiol. 2016;67:1519–27.
Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–51.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30:449–56.
Asayama K, Ohkubo T, Kikuya M, Metoki H, Hoshi H, Hashimoto J, et al. Prediction of stroke by self-measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the Joint National Committee 7 classification: the Ohasama study. Stroke. 2004;35:2356–61.
Parati G, Stergiou GS, Bilo G, Kollias A, Pengo M, Ochoa JE, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the working group on blood pressure monitoring and cardiovascular variability of the European Society of Hypertension. J Hypertens. 2021;39:1742–67.
Shimbo D, Artinian NT, Basile JN, Krakoff LR, Margolis KL, Rakotz MK, et al. Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation. 2020;142:e42–63.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269–324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Fujiwara T, McManus RJ, Kario K. Management of hypertension in the digital era: perspectives and future directions. Hipertens Riesgo Vasc. 2022;39:79–91.
Kario K, Morisawa Y, Sukonthasarn A, Turana Y, Chia YC, Park S, et al. COVID-19 and hypertension-evidence and practical management: guidance from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:1109–19.
Khan NA, Stergiou GS, Omboni S, Kario K, Renna N, Chapman N, et al. Virtual management of hypertension: lessons from the COVID-19 pandemic-International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. J Hypertens. 2022;40:1435–48.
Omboni S, Padwal RS, Alessa T, Benczúr B, Green BB, Hubbard I, et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health. 2022;1:7–35.
Shibata S, Arima H, Asayama K, Hoshide S, Ichihara A, Ishimitsu T, et al. Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19. Hypertens Res. 2020;43:1028–46.
Wang JG, Li Y, Chia YC, Cheng HM, Minh HV, Siddique S, et al. Telemedicine in the management of hypertension: evolving technological platforms for blood pressure telemonitoring. J Clin Hypertens (Greenwich). 2021;23:435–9.
Kario K, Tomitani N, Kanegae H, Yasui N, Nagai R, Harada H. The further development of out-of-office BP monitoring: Japan’s ImPACT Program Project’s achievements, impact, and direction. J Clin Hypertens (Greenwich). 2019;21:344–9.
Okumiya K, Matsubayashi K, Wada T, Fujisawa M, Osaki Y, Doi Y, et al. A U-shaped association between home systolic blood pressure and four-year mortality in community-dwelling older men. J Am Geriatr Soc. 1999;47:1415–21.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Ntineri A, Kalogeropoulos PG, Kyriakoulis KG, Aissopou EK, Thomopoulou G, Kollias A, et al. Prognostic value of average home blood pressure and variability: 19-year follow-up of the Didima study. J Hypertens. 2018;36:69–76.
Bobrie G, Genès N, Vaur L, Clerson P, Vaisse B, Mallion JM, et al. Is “isolated home” hypertension as opposed to “isolated office” hypertension a sign of greater cardiovascular risk? Arch Intern Med. 2001;161:2205–11.
Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–7.
Fujiwara T, Hoshide S, Kanegae H, Kario K. Clinical impact of the maximum mean value of home blood pressure on cardiovascular outcomes: a novel indicator of home blood pressure variability. Hypertension. 2021;78:840–50.
Kaihara T, Hoshide S, Tomitani N, Kanegae H, Kario K. Maximum home systolic blood pressure is a marker of carotid atherosclerosis. Clin Exp Hypertens. 2019;41:774–8.
Matsui Y, Ishikawa J, Eguchi K, Shibasaki S, Shimada K, Kario K. Maximum value of home blood pressure: a novel indicator of target organ damage in hypertension. Hypertension. 2011;57:1087–93.
Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, et al. Japanese society of hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003;26:771–82.
Hoshide S, Yano Y, Mizuno H, Kanegae H, Kario K. Day-by-day variability of home blood pressure and incident cardiovascular disease in clinical practice: the J-HOP study (Japan morning surge-home blood pressure). Hypertension. 2018;71:177–84.
Mehlum MH, Liestøl K, Kjeldsen SE, Julius S, Hua TA, Rothwell PM, et al. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J. 2018;39:2243–51.
Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, et al. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016;354:i4098.
Mena LJ, Felix VG, Melgarejo JD, Maestre GE. 24-hour blood pressure variability assessed by average real variability: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6:e006895.
Kario K. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension. 2020;76:640–50.
Acknowledgements
Medical writing support was provided by Nicola Ryan, independent medical writer, and by Ayako Okura, English publication coordinator, funded by Jichi Medical University.
Funding
This study was financially supported in part by a grant from the Foundation for the Development of the Community (Tochigi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KK has received research funding from Omron Healthcare Co, Fukuda Denshi, and A&D Co. None of the other authors have any conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kario, K., Tomitani, N., Fujiwara, T. et al. Peak home blood pressure as an earlier and strong novel risk factor for stroke: the practitioner-based nationwide J-HOP study extended. Hypertens Res 46, 2113–2123 (2023). https://doi.org/10.1038/s41440-023-01297-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01297-9
Keywords
This article is cited by
-
Evidence for the surge blood pressure resonance hypothesis as a trigger for cardiovascular disease events
Hypertension Research (2023)
-
Exercise training improves blood pressure reactivity to stress: a systematic review and meta-analysis
Scientific Reports (2023)
-
Peak home blood pressure: new heights for SMBP
Hypertension Research (2023)
-
The Promise and Illusion of Continuous, Cuffless Blood Pressure Monitoring
Current Cardiology Reports (2023)