Abstract
Reactive astrocytes play an important role in neurological diseases, but their molecular and functional phenotypes in epilepsy are unclear. Here, we show that in patients with temporal lobe epilepsy (TLE) and mouse models of epilepsy, excessive lipid accumulation in astrocytes leads to the formation of lipid-accumulated reactive astrocytes (LARAs), a new reactive astrocyte subtype characterized by elevated APOE expression. Genetic knockout of APOE inhibited LARA formation and seizure activities in epileptic mice. Single-nucleus RNA sequencing in TLE patients confirmed the existence of a LARA subpopulation with a distinct molecular signature. Functional studies in epilepsy mouse models and human brain slices showed that LARAs promote neuronal hyperactivity and disease progression. Targeting LARAs by intervention with lipid transport and metabolism could thus provide new therapeutic options for drug-resistant TLE.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Raw data of snRNA-seq and bulk RNA-seq of human cortex samples, and RNA-seq of mouse hippocampus samples have been deposited in the Gene Expression Omnibus under accession GSE190453. Raw data of lipidomics of human cortex and mouse hippocampus samples have been deposited in Gene Expression Omnibus under accession GSE190453. Single-cell RNA-seq of glioma were obtained from the European Genome–phenome Archive repository, under accession codes EGAS00001002185, EGAS00001001900 and EGAS00001003845. Quantitative data that support the findings of this study are available within the paper. Source data are provided with this paper. All other data that support the findings of this study are available from the corresponding authors on reasonable request.
References
Bui Anh, D. et al. Dentate gyrus mossy cells control spontaneous convulsive seizures and spatial memory. Science 359, 787–790 (2018).
Löscher, W., Potschka, H., Sisodiya, S. M., Vezzani, A. & Barker, E. L. Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol. Rev. 72, 606–638 (2020).
Maroso, M. et al. Toll-like receptor 4 and high-mobility group box-1 are involved in ictogenesis and can be targeted to reduce seizures. Nat. Med. 16, 413–419 (2010).
Devinsky, O. et al. Epilepsy. Nat. Rev. Dis. Primers 4, 18024 (2018).
Vezzani, A., Balosso, S. & Ravizza, T. Neuroinflammatory pathways as treatment targets and biomarkers in epilepsy. Nat. Rev. Neurol. 15, 459–472 (2019).
Verkhratsky, A. & Nedergaard, M. Physiology of astroglia. Physiol. Rev. 98, 239–389 (2018).
Absinta, M. et al. A lymphocyte–microglia–astrocyte axis in chronic active multiple sclerosis. Nature 597, 709–714 (2021).
Chun, H. et al. Severe reactive astrocytes precipitate pathological hallmarks of Alzheimer’s disease via H2O2− production. Nat. Neurosci. 23, 1555–1566 (2020).
Liddelow, S. A. et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541, 481–487 (2017).
Sanmarco, L. M. et al. Gut-licensed IFN-γ+ NK cells drive LAMP1+TRAIL+ anti-inflammatory astrocytes. Nature 590, 473–479 (2021).
Bedner, P. et al. Astrocyte uncoupling as a cause of human temporal lobe epilepsy. Brain 138, 1208–1222 (2015).
Devinsky, O., Vezzani, A., Najjar, S., De Lanerolle, N. C. & Rogawski, M. A. Glia and epilepsy: excitability and inflammation. Trends Neurosci. 36, 174–184 (2013).
Patel, D. C., Tewari, B. P., Chaunsali, L. & Sontheimer, H. Neuron–glia interactions in the pathophysiology of epilepsy. Nat. Rev. Neurosci. 20, 282–297 (2019).
Wheeler, M. A. et al. MAFG-driven astrocytes promote CNS inflammation. Nature 578, 593–599 (2020).
Wang, C. et al. Selective removal of astrocytic APOE4 strongly protects against tau-mediated neurodegeneration and decreases synaptic phagocytosis by microglia. Neuron 109, 1657–1674 (2021).
Shi, Y. et al. Overexpressing low-density lipoprotein receptor reduces tau-associated neurodegeneration in relation to apoE-linked mechanisms. Neuron 109, 2413–2426 (2021).
Hasel, P., Rose, I. V. L., Sadick, J. S., Kim, R. D. & Liddelow, S. A. Neuroinflammatory astrocyte subtypes in the mouse brain. Nat. Neurosci. 24, 1475–1487 (2021).
Sadick, J. S. et al. Astrocytes and oligodendrocytes undergo subtype-specific transcriptional changes in Alzheimer’s disease. Neuron 110, 1788–1805 (2022).
Escartin, C. et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat. Neurosci. 24, 312–325 (2021).
Brekk, O. R., Honey, J. R., Lee, S., Hallett, P. J. & Isacson, O. Cell-type-specific lipid storage changes in Parkinson’s disease patient brains are recapitulated by experimental glycolipid disturbance. Proc. Natl Acad. Sci. USA 117, 27646–27654 (2020).
Davis Albert, A. et al. APOE genotype regulates pathology and disease progression in synucleinopathy. Sci. Transl. Med. 12, eaay3069 (2020).
Dong, Y. et al. Oxidized phosphatidylcholines found in multiple sclerosis lesions mediate neurodegeneration and are neutralized by microglia. Nat. Neurosci. 24, 489–503 (2021).
Fanning, S. et al. Lipidomic analysis of α-synuclein neurotoxicity identifies stearoyl CoA desaturase as a target for Parkinson treatment. Mol. Cell 73, 1001–1014 (2019).
Xu, Y., Propson, N. E., Du, S., Xiong, W. & Zheng, H. Autophagy deficiency modulates microglial lipid homeostasis and aggravates tau pathology and spreading. Proc. Natl Acad. Sci. USA 118, e2023418118 (2021).
Claes, C. et al. Plaque-associated human microglia accumulate lipid droplets in a chimeric model of Alzheimer’s disease. Mol. Neurodegener. 16, 50 (2021).
Ioannou, M. S. et al. Neuron-astrocyte metabolic coupling protects against activity-induced fatty acid toxicity. Cell 177, 1522–1535 (2019).
Guttenplan, K. A. et al. Neurotoxic reactive astrocytes induce cell death via saturated lipids. Nature 599, 102–107 (2021).
Dossi, E. et al. Pannexin-1 channels contribute to seizure generation in human epileptic brain tissue and in a mouse model of epilepsy. Sci. Transl. Med. 10, eaar3796 (2018).
Hadjiabadi, D. et al. Maximally selective single-cell target for circuit control in epilepsy models. Neuron 109, 2556–2572 (2021).
Liang, L. P., Ho, Y. S. & Patel, M. Mitochondrial superoxide production in kainate-induced hippocampal damage. Neuroscience 101, 563–570 (2000).
Racine, R. J. Modification of seizure activity by electrical stimulation: II. Motor seizure. Electroencephalogr. Clin. Neurophysiol. 32, 281–294 (1972).
Wang, Y. et al. Depolarized GABAergic signaling in subicular microcircuits mediates generalized seizure in temporal lobe epilepsy. Neuron 95, 92–105 (2017).
Li, X. et al. Astrocytic ApoE reprograms neuronal cholesterol metabolism and histone-acetylation-mediated memory. Neuron 109, 957–970 (2021).
Qi, G. et al. ApoE4 impairs neuron–astrocyte coupling of fatty acid metabolism. Cell Rep. 34, 108572 (2021).
Liu, L., MacKenzie, K. R., Putluri, N., Maletic-Savatic, M. & Bellen, H. J. The glia–neuron lactate shuttle and elevated ROS promote lipid synthesis in neurons and lipid droplet accumulation in glia via APOE/D. Cell Metab. 26, 719–737 (2017).
Shi, Y. et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nature 549, 523–527 (2017).
Sienski, G. et al. APOE4 disrupts intracellular lipid homeostasis in human iPSC-derived glia. Sci. Transl. Med. 13, eaaz4564 (2021).
Zhao, N. et al. Alzheimer’s risk factors age, APOE genotype and sex drive distinct molecular pathways. Neuron 106, 727–742 (2020).
Rambold, A. S., Cohen, S. & Lippincott-Schwartz, J. Fatty acid trafficking in starved cells: regulation by lipid droplet lipolysis, autophagy, and mitochondrial fusion dynamics. Dev. Cell 32, 678–692 (2015).
Habib, N. et al. Disease-associated astrocytes in Alzheimer’s disease and aging. Nat. Neurosci. 23, 701–706 (2020).
Batiuk, M. Y. et al. Identification of region-specific astrocyte subtypes at single cell resolution. Nat. Commun. 11, 1220 (2020).
Yang, Y. et al. Protective effects of prenatal choline supplementation on seizure-induced memory impairment. J. Neurosci. 20, RC109 (2000).
El Yacoubi, M. et al. Absence of the adenosine A2A receptor or its chronic blockade decrease ethanol withdrawal-induced seizures in mice. Neuropharmacology 40, 424–432 (2001).
Woods, B. T. & Chiu, T.-M. In vivo 1H spectroscopy of the human brain following electroconvulsive therapy. Ann. Neurol. 28, 745–749 (1990).
Matos, M. et al. Deletion of adenosine A2A receptors from astrocytes disrupts glutamate homeostasis leading to psychomotor and cognitive impairment: relevance to schizophrenia. Biol. Psychiatry 78, 763–774 (2015).
Bu, G. Apolipoprotein E and its receptors in Alzheimer’s disease: pathways, pathogenesis and therapy. Nat. Rev. Neurosci. 10, 333–344 (2009).
Larramona-Arcas, R. et al. Sex-dependent calcium hyperactivity due to lysosomal-related dysfunction in astrocytes from APOE4 versus APOE3 gene targeted replacement mice. Mol. Neurodegener. 15, 35 (2020).
Vossel, K. A. et al. Effect of levetiracetam on cognition in patients with Alzheimer disease with and without epileptiform activity: a randomized clinical trial. JAMA Neurol. 78, 1345–1354 (2021).
Vossel, K. A. et al. Seizures and epileptiform activity in the early stages of Alzheimer disease. JAMA Neurol. 70, 1158–1166 (2013).
Aboud, O., Mrak, R. E., Boop, F. A. & Griffin, W. S. T. Epilepsy: neuroinflammation, neurodegeneration, and APOE genotype. Acta Neuropathol. Commun. 1, 41 (2013).
Tcw, J. et al. Cholesterol and matrisome pathways dysregulated in astrocytes and microglia. Cell 185, 2213–2233 (2022).
Ayhan, F. et al. Resolving cellular and molecular diversity along the hippocampal anterior-to-posterior axis in humans. Neuron 109, 2091–2105 (2021).
Ayhan, F., Douglas, C., Lega, B. C. & Konopka, G. Nuclei isolation from surgically resected human hippocampus. STAR Protoc. 2, 100844 (2021).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Satija, R., Farrell, J. A., Gennert, D., Schier, A. F. & Regev, A. Spatial reconstruction of single-cell gene expression data. Nat. Biotechnol. 33, 495–502 (2015).
Chen, B. et al. A disinhibitory nigra-parafascicular pathway amplifies seizure in temporal lobe epilepsy. Nat. Commun. 11, 923 (2020).
Klein, S., Bankstahl, M. & Löscher, W. Inter-individual variation in the effect of antiepileptic drugs in the intrahippocampal kainate model of mesial temporal lobe epilepsy in mice. Neuropharmacology 90, 53–62 (2015).
Liu, Y. et al. Functions of lactate in the brain of rat with intracerebral hemorrhage evaluated with MRI/MRS and in vitro approaches. CNS Neurosci. Ther. 26, 1031–1044 (2020).
Chen, Z. P. et al. Histamine H1 receptor contributes to vestibular compensation. J. Neurosci. 39, 420–433 (2019).
Wang, Y. et al. Sperm microRNAs confer depression susceptibility to offspring. Sci. Adv. 7, eabd7605 (2021).
Viana da Silva, S. et al. Early synaptic deficits in the APP/PS1 mouse model of Alzheimer’s disease involve neuronal adenosine A2A receptors. Nat. Commun. 7, 11915 (2016).
Shao, W. et al. Suppression of neuroinflammation by astrocytic dopamine D2 receptors via alphaB-crystallin. Nature 494, 90–94 (2013).
Acknowledgements
We thank L. -P. Liang and D. Siegel from the University of Colorado for technical advice and helpful discussions. We thank B. Traw from Nanjing University for help with the manuscript; S. -Y. Peng from Westlake University and Y. Bao from University of Vienna for help with color illustrations. We acknowledge grants from the National Natural Science Foundation of China (21877060 to C.Y., 32070656 to D.C. and 31900824 to Z.-P.C.) and the Postdoctoral Research Foundation of China (2019M651779 to Z.-P.C.).
Author information
Authors and Affiliations
Contributions
C.Y., X.L. and Z.-P.C. designed the study. Z.-P.C. and S.W. performed the primary cell culture. S.W., H.Y. and M.-J.W. conducted the qPCR and western blotting experiments. Z.-P.C. performed the immunofluorescence and whole-cell patch-clamp experiments. X.Z., Z.-P.C. and L.K. performed the EEG and MEA recordings. X.Z., Z.-P.C., Z.W. and P.L. performed the in vivo MRI and MRS recordings. X.L., D.C., W.F. and T.H. prepared human cortex samples and mouse hippocampus samples for snRNA-seq, RNA-seq or lipidomics. D.C. and W.F. performed RNA-seq analyses. X.J., Q.Z. and S.-T.X. established the epilepsy model and took care of the mice. Z.-P.C., S.W., X.Z. and W.F. analyzed the data. C.Y. and Z.-P.C. wrote the manuscript with the help of J.-N.Z., X.J., Q.Z., C.H. and L.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Neuroscience thanks Peter Klink, Afonso Silva, and the other, anonymous, reviewer(s) for their contribution to the peer review process for this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
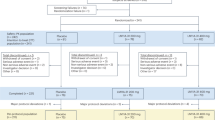
Extended Data Fig. 1 Abnormal lipid accumulation in drug-resistant TLE patients.
MRS of the brain from 4 patients with drug-resistant TLE showing lipid peaks in the lesion side and the contralateral normal side. Data from patient 1 is also shown in Fig. 1a with adjustments.
Extended Data Fig. 2 Abnormal lipid accumulation in the cortex and hippocampus of TLE patients.
a, b, Immunofluorescence detection of lipid accumulation in human cortex samples. a, NG2 (violet) & BD493 (green) double-labeling of LDs in oligodendrocyte progenitor cells (normal, n = 6; TLE, n = 6; scale bar, 10 µm). b, IBA1 (cyan) & BD493 double-labeling in microglia (normal, n = 6; TLE, n = 6; scale bar, 10 µm). c-e, Lipidomic profiling of human cortex samples (normal, n = 6; TLE, n = 6). c, d, Diagrams showing glycerophospholipids levels. e, KEGG pathway enrichment analysis showing activation of lipid metabolism-related pathways in TLE patients. f, g, Immunofluorescence detection of lipid accumulation in two human hippocampus samples. f, Patient 5. Upper, MAP2 (green), IBA1 (cyan) and Nile Red (violet) triple-labeling of LDs; lower, NG2 (cyan) & Nile Red (violet) double-labeling of LDs in oligodendrocyte progenitor cells (scale bars, 25 µm and 10 µm). LD staining in neurons for patient 5 is shown in Fig. 1f. g, LD staining in patient 6 was performed similarly to patient 5. For a-b, data represent the mean ± SEM, n values represent individual patients. Statistical analysis was performed using two-sided unpaired Student’s t-tests (a-b).
Extended Data Fig. 3 Abnormal lipid accumulation in the hippocampus of KA-induced epileptic mice.
a, b, Immunofluorescence detection of c-Fos levels in the hippocampal CA3 and CA1 regions of mice after intrahippocampal injection of KA (n = 5). c, Immunofluorescence detection of LDs in hippocampal CA3 from a (n = 6). d,e, In vivo MRS detection of lipid peaks in the hippocampus of mice from a at the acute stage (24 h post KA injection). d, Lipid levels in the hippocampus of the KA-injected side (n = 6) and the saline-injected side were quantified and compared (n = 5). (e) Lipid levels in the hippocampus of sham operation mice (n = 6) and saline-injected mice (n = 4) were quantified and compared. f, g, Immunofluorescence detection of lipid accumulation in mouse hippocampus from KA-induced epileptic mice (i.p. KA) at the chronic stage. f, IBA1 (red) & BD493 (green) double-labeling in microglia (Ctrl, n = 5; KA, n = 8; scale bar, 25 µm). (g) NG2 (violet) & BD493 double-labeling in oligodendrocyte progenitor cells (Ctrl, n = 6; KA, n = 6; scale bar, 10 µm). h-l, Lipidomic profiling of mouse hippocampus samples at the chronic stage (Ctrl, n = 6; KA, n = 6). h, Diagram showing lipids levels in control and KA-treated mice. i, KEGG pathway enrichment analysis showing upregulation of lipid metabolism-related pathways in epileptic mice. j-l, Heatmap and histogram showing significantly elevated lipids such as TGs, DGs, and CEs in the epileptic mice. For b-g, i, k-l, data represent the mean ± SEM, n values represent individual animals. Statistical analysis was performed using two-sided unpaired Student’s t-tests (b-g and k-l) and two-sided Fisher’s exact test with BH’s post hoc test (i).
Extended Data Fig. 4 Elevated APOE expression in astrocytes of TLE patients.
a-c, Comparison of the expression levels of representative lipid transport- and metabolism-related genes between TLE patients and non-epileptic controls. a, Dot plot depicting selected differentially expressed genes showing their expression in each patient. b, Dot plot depicting selected genes in each cluster. c. Dot plot depicting the difference of APOE expression between TLE patients and non-epileptic controls in each cell cluster. d, Heatmap showing the expression levels of representative lipid transport- and metabolism-related genes between TLE patients and non-epileptic controls analyzed by bulk RNA-seq. e, Immunofluorescence detection of APOE in the cortex of TLE patients and non-epileptic controls (Normal, n = 6; TLE, n = 6; scale bar, 10 µm). f-h, Immunofluorescence detection of APOE colocalization with different cell types. f, MAP2 (cyan) & APOE (green) double-labeling in neurons (Left, Normal, n = 6; TLE, n = 6; right, Normal, n = 8; TLE, n = 8; scale bar, 25 µm and 10 µm). g, IBA1 (cyan) & APOE (red) double-labeling in microglia (Normal, n = 8; TLE, n = 8; scale bar, 10 µm). h, NG2 (green) & APOE (red) double-labeling in oligodendrocyte progenitor cells (Normal, n = 5; TLE, n = 5; scale bar, 10 µm). For f-h, data represent the mean ± SEM, n values represent individual patients. Statistical analysis was performed using two-sided unpaired Student’s t-tests (f-h).
Extended Data Fig. 5 APOE mediated lipid transfer from neurons to astrocytes.
a, Primary neurons were pre-incubated with Red-C12, treated with 100 µM KA for 12 h, then co-cultured with primary astrocytes separated by a cell strainer. b, MAP2 (red) & c-Fos (green) double-labeling in primary neurons treated with KA (Veh, n = 5; 100 µM KA, n = 5; scale bar, 10 µm). c, GFAP (violet), Red-C12 (red) & BD493 (green) triple-labeling in primary astrocytes after co-culture with KA-treated neurons (Veh, n = 7, KA, n = 7; scale bar, 10 µm). d-f, Effect of KA treatment on lipid accumulation in wild-type and APOE−/− neurons. d, WT and APOE−/− neurons in co-culture were treated with 100 µM KA or PBS for 12 h. e, NeuN (magenta), APOE (blue) and BD493 (green) triple-labeling of both WT and APOE−/− neurons (scale bars: left, 10 µm; right, 1 µm). f, Statistics of LD number and volume in WT (APOE+) and APOE−/− (APOE-) neurons (Upper, PBS APOE-, n = 9; PBS APOE+, n = 14; KA APOE-, n = 9; KA APOE+, n = 17; lower, PBS, APOE-, n = 21; PBS APOE+, n = 30; KA APOE-, n = 32; KA APOE+, n = 32 LDs). g-i, WT neurons were treated with 100 µM KA or PBS for 12 h, the NCM were then collected and used to treat WT and APOE−/− astrocytes in co-culture. g, Diagram of treatment. h, GFAP (magenta), APOE (blue) and BD493 (green) triple-labeling of both WT and APOE−/− astrocytes (scale bars: left, 50 µm; right, 10 µm). i, Statistics of LD number and volume in WT (APOE+) and APOE−/− (APOE-) astrocytes (Upper, PBS APOE-, n = 13; PBS APOE+, n = 15; KA APOE-, n = 7; KA APOE+, n = 9; lower, PBS APOE-, n = 79; PBS APOE+, n = 51; KA APOE-, n = 86; KA APOE+, n = 154 LDs). For c, f and i, data represent the mean ± SEM. Statistical analysis was performed using two-sided unpaired Student’s t-tests (c) and two-way ANOVA with Bonferroni’s post hoc test (f and i).
Extended Data Fig. 6 Sub-clustering of astrocytes and the association between APOE levels and lipid accumulation in astrocytes of TLE patients.
a, The astrocyte clusters of TLE patients (n = 4) and non-epileptic controls (n = 4). b, Histogram showing the percentage of different astrocyte subclusters in TLE patients and non-epileptic controls. c, Dot plot depicting selected differentially expressed genes for each subcluster and associated cluster labeling. Dot size corresponds to the percentage of nuclei expressing the gene in each cluster, and color represents the average expression level. d, Dot plot of APOE expression in each subcluster. e-f, Immunofluorescence detection of lipid accumulation in astrocytes of TLE patients. e, GFAP (magenta), APOE (blue) and BD493 (green) triple-labeling in the cortex of TLE patients (scale bars: left, 20 µm; right, 2 µm). f, Astrocytes were categorized into APOE-negative (APOE-) and APOE-positive (APOE+) subpopulations depending on the absence or presence of APOE immunostaining. Statistics of LD number and volume in APOE- or APOE+ astrocytes are shown (Left, Normal APOE-, n = 7; Normal APOE+, n = 12; TLE APOE-, n = 10; TLE APOE+, n = 11; right, Normal APOE-, n = 166; Normal APOE+, n = 84; TLE APOE-, n = 130; TLE APOE+, n = 70 LDs). For f, data represent the mean ± SEM. Statistical analysis was performed using two-way ANOVA with Bonferroni’s post hoc test (f).
Extended Data Fig. 7 Characterization of astrocyte reactivity in epileptic mice and TLE patients.
a-h, Characterization of astrocyte reactivity in the cortex samples of TLE patients. a, Transcriptomic profiling of human cortex samples showing the expression levels of reactive astrocyte marker genes (n = 3). b, KEGG enrichment analysis showing upregulation of reactive astrocyte-related pathways in TLE patients. c, Immunofluorescence detection of GFAP intensity in TLE patients (normal, n = 6; TLE, n = 6; scale bars, 25 and 10 µm). d, iNOS (red) and GFAP (green) double-labeling in human cortex samples (normal, n = 8; TLE, n = 8; scale bar, 5 µm). e, g, Immunoblotting of GFAP protein in human cortex samples (normal, n = 4; TLE, n = 5). f, h, Immunoblotting of iNOS protein in human cortex samples (normal, n = 4; TLE, n = 5). i-n, Characterization of astrocyte reactivity in the hippocampus of epileptic mice. i, KEGG enrichment analysis following bulk RNA-seq showing upregulation of reactive astrocyte-related pathways in epileptic mice. j, NeuN (red) and GFAP (green) double-labeling in the hippocampus of epileptic mice (n = 5; scale bar, 10 µm). k, iNOS (red) and GFAP (green) double-labeling in the hippocampus of epileptic mice (n = 7; scale bars, 25 and 10 µm). l-n, Immunoblotting of GFAP and iNOS proteins in mouse hippocampus with quantification results shown to the right (m, n, n = 6 or 4). For c-d, g-h, j and m-n, data represent the mean ± SEM, n values represent individual patients or animals. Statistical analysis was performed using two-sided unpaired Student’s t-tests (c-d, g-h, j and m-n).
Extended Data Fig. 8 Effect of astrocyte-specific APOE knockout on gliosis and neuronal loss in KA-induced epileptic mice.
a, GFAP (red) and NeuN (green) double-labeling in mouse hippocampus (n = 5 mice in each group, representative images are shown; scale bars, 150 µm & 10 µm). b, IBA1 (violet) and NeuN (green) double-labeling in mouse hippocampus (n = 5 mice in each group, representative images are shown; scale bars, 50 µm & 10 µm). c, Statistical analysis of NeuN+, GFAP+, and IBA1+ cells in WT or APOE cKO mice with or without KA stimulation. For c, data represent the mean ± SEM. Statistical analysis was performed using two-way ANOVA with Bonferroni’s post hoc test (c).
Extended Data Fig. 9 Lipid-accumulated reactive astrocytes promoted both electrographic and behavioral seizures in epileptic mice.
a, Diagram showing the timeline of epileptic model establishment, electrode implantation, EEG recording and MEA recording in APOE−/− mice. b-f, Effect of APOE knockout on KA-induced epilepsy symptoms in mice. b, Behavioral seizures were evaluated at the acute stage using the Racine scale. c, Electrographic seizure-like activities were assessed at the chronic stage by ex vivo MEA recording (WT KA, n = 13; APOE−/− KA, n = 13). The frequency and duration of seizure-like activities were recorded within a 2-min window. d-f, Electrographic seizure-like activities were also assessed by in vivo EEG (WT KA, n = 7; APOE−/− KA, n = 8; APOE−/− KA-CDP choline, n = 10). The number and duration of seizures (EEG) were recorded within a 24-hour window for three continuous days. For b-c and f, data represent the mean ± SEM, n values represent individual animals. Statistical analysis was performed using two-sided unpaired Student’s t-tests (b (left and middle) and c), two-sided Fisher’s exact test (b (right)) and two-way ANOVA with Bonferroni’s post hoc test (f).
Extended Data Fig. 10 Astrocyte-specific knockdown of A2AR or pharmacological blockage of A2AR in mice decreased electrographic seizures.
a-d, Astrocyte-specific knockdown of A2AR or pharmacological blockage of A2AR in mice decreased electrographic seizures. a, Diagram showing the virus injection site confirmed by immunofluorescence detection of GFAP (violet) and AAV-A2AR-shRNA-EGFP co-localization (scale bars, 150 µm and 10 µm). b, Immunoblotting of A2AR protein in the hippocampus of AAV-ctrl-shRNA epileptic mice (n = 3) and AAV-A2AR-shRNA epileptic mice (n = 3). c, Immunofluorescence detection of A2AR (red) intensity in the astrocytes of AAV-ctrl-shRNA epileptic mice (n = 8) and AAV-A2AR-shRNA epileptic mice (n = 9; scale bars, 20 µm and 10 µm). d, Whole-cell current clamp recording of hippocampal neuronal activity in AAV-ctrl-shRNA epileptic mice (n = 11) and AAV-A2AR-shRNA epileptic mice (n = 11). e-j, Pharmacological blockage of A2AR in mice decreased electrographic seizures. e, Diagram showing the timeline of epileptic model establishment, drug administration, electrode implantation, EEG recording and MEA recording. f, g, In vivo EEG recording of epileptic mice treated with vehicle or ZM241385. Number of seizures per day and seizure duration were analyzed (g, left, Veh, n = 8; ZM241385, n = 10 mice; g, right, Veh, n = 19 seizure events from 8 mice; ZM241385, n = 11 from 10 mice; f, scale bars, 1 s and 0.5 mV). h-j, Ex vivo MEA recording of brain slices from epileptic mice. h, Mouse hippocampal slices were incubated with pro-epileptic free Mg2+/high K+ artificial cerebrospinal fluid (ACSF) for 30 min to induce seizure-like discharges. i, j, Bath application of ZM241385 (1 µM, 10 min pretreatment) significantly inhibited seizure-like discharges in the brain slices (12 slices from 5 mice; scale bars, 20 ms and 0.5 mV). For b-d, g, and j, data represent the mean ± SEM. Statistical analysis was performed using two-sided unpaired Student’s t-tests (b-d and g) and two-sided paired Student’s t-tests (j).
Supplementary information
Supplementary Information
Supplementary Figs. 1–16, Supplementary Table 1, titles for Supplementary Tables 2–7 and source data for immunoblots in Supplementary Figs. 1, 2, 10, 11, 12 and 15.
Supplementary Tables 2–7
snRNA-seq and bulk RNA-seq data.
Video-EEG recording for the characterization of epilepsy mouse model.
Supplementary Data
Statistical source data for Supplementary Figs. 1–15.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 2
Unprocessed western blots.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 3
Unprocessed western blots.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 4
Unprocessed western blots.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 7
Unprocessed western blots.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data.
Source Data Extended Data Fig. 10
Statistical source data.
Source Data Extended Data Fig. 10
Unprocessed western blots.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, ZP., Wang, S., Zhao, X. et al. Lipid-accumulated reactive astrocytes promote disease progression in epilepsy. Nat Neurosci 26, 542–554 (2023). https://doi.org/10.1038/s41593-023-01288-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41593-023-01288-6
This article is cited by
-
Cell type-specific roles of APOE4 in Alzheimer disease
Nature Reviews Neuroscience (2024)
-
Disease-Associated Neurotoxic Astrocyte Markers in Alzheimer Disease Based on Integrative Single-Nucleus RNA Sequencing
Cellular and Molecular Neurobiology (2024)
-
The role of ApoE in fatty acid transport from neurons to astrocytes under ischemia/hypoxia conditions
Molecular Biology Reports (2024)
-
Spinal apolipoprotein E is involved in inflammatory pain via regulating lipid metabolism and glial activation in the spinal dorsal horn
Biology Direct (2023)
-
Astrocytes in human central nervous system diseases: a frontier for new therapies
Signal Transduction and Targeted Therapy (2023)