Abstract
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are menstrual cycle-related disorders characterised by psychological and physical symptoms which impact functioning. Little is known about avenues for help-seeking for these disorders. Therefore, we sought to examine help-seeking behaviours and experiences. An online survey was delivered and data from 530 participants whose mental health was affected by their menstrual cycle were analysed. All participants endorsed at least one premenstrual symptom, with 97.17% experiencing functional impairment. Help was sought by 64.91% (online: 29.81%; formal: 7.36%; online and formal: 27.74%), with 78.49% perceiving that their symptoms were not taken seriously when seeking formal help. Most sought help online to look up symptoms (85.57%) and treatment options (39.67%). The study revealed an association between premenstrual symptoms and mental wellbeing, as well as revealing a high prevalence of online help-seeking, emphasising the need for high-quality, evidence-based online resources and improvement of formal care provision.
Similar content being viewed by others
Introduction
Premenstrual symptoms encompass a range of physical, behavioural, and psychological symptoms, with their presentation varying between individuals1. Many women of reproductive age will experience at least some premenstrual symptoms2, with up to 90% experiencing at least one symptom3. For some, the severity of premenstrual symptoms interferes with daily functioning, meeting the threshold for premenstrual syndrome (PMS) or in more extreme cases, premenstrual dysphoric disorder (PMDD). PMS and PMDD are cyclical recurrent disorders occurring during the luteal phase of the menstrual cycle, with symptoms typically improving following onset of menses4. A systematic review and meta-analysis of 17 studies found a pooled prevalence estimate of around 48% for PMS5. Moreover, commonly cited prevalence estimates of PMDD are between 3 and 8%3 but may be as high as 13 to 18% depending on the stringency of the diagnostic criteria applied2. These estimates, even the more conservative ones for PMDD, indicate that these disorders may be more prevalent than some mood disorders, such as bipolar disorder2.
There is evidence of a substantial burden associated with PMS and PMDD, including increased work absenteeism, decreased productivity, and lowered quality of life3,4,6. Additionally, PMS and PMDD are associated with an increased risk profile including suicidal ideation7,8, with PMDD being further associated with risk of suicide planning and attempts7. In fact, a diagnosis of PMDD increases suicidal ideation four-fold and risk of suicide attempts seven-fold7. Moreover, individuals with a formal diagnosis of PMDD report emotional self-regulation using substance use or self-harm as a coping mechanism9. Therefore, early and accurate identification of individuals experiencing mental health symptoms related to their menstrual cycle and provision of appropriate symptom management is essential to minimise associated burdens and the risk of suicidality or engaging in risky self-regulating behaviours.
Typically, a primary care health care provider (HCP), such as a General Practitioner (GP), serves as the initial point of contact for formal support and also plays the role of a gatekeeper to more specialised health care services. However, HCPs in the United Kingdom (UK) report a lack of training and knowledge about PMDD10 and there are reports of delays to a correct diagnosis10 and misdiagnosis of PMDD with bipolar disorder11. Moreover, those who have sought formal support from a HCP for PMDD describe interactions as unsupportive and even dismissive, with a perception of an unwillingness to acknowledge mental health symptoms related to the menstrual cycle9, perhaps due to a lack of knowledge of PMDD12. In contrast, the internet is becoming a much more frequent source of health-related information gathering and can empower individuals by equipping them with increased understanding of disorders and management options, as well as increasing access to self-help resources. Women are more likely to search for health information from online sources (i.e., using search engines, looking for relevant forums) than from their HCP13. However, for mental health symptoms related to the menstrual cycle, little is known about the specific types of information which are searched for and engaged with online. In fact, to the best of our knowledge, there are no recent studies examining the help-seeking behaviours of individuals in the UK who experience mental health symptoms related to their menstrual cycle. Beyond elucidating insights as to the primary avenues for help-seeking (e.g., formal, online, or both), understanding perceptions of the usefulness of online resources and formal care quality can inform the design of improved formal care provision and high-quality online resources to be accessed independently by patients or through signposting or referral by a HCP.
With this in mind, the current study aimed to (1) investigate the association between premenstrual symptoms and mental wellbeing in a study population who reports mental health symptoms related to the menstrual cycle; and, (2) explore help-seeking behaviours and experiences of individuals who experience mental health concerns in relation to the menstrual cycle. Additionally, differences in help-seeking behaviours and experiences associated with different severity levels and burden of premenstrual mental health symptoms were examined. To achieve this, the frequency of premenstrual symptoms are reported and the incidence of PMS and PMDD in the study population was estimated using the premenstrual symptom screening tool (PSST; 14). The PSST was selected over a prospective tool due to concerns about potential study dropout15. Examining the association between premenstrual symptoms and mental wellbeing is important in providing a more comprehensive understanding of the broader individual implications of these symptoms, beyond functional impairment, as well as contributing to an increase in public and healthcare professionals’ knowledge of associated impacts. Moreover, investigating help-seeking patterns and experiences for mental health symptoms associated with the menstrual cycle can inform public health services by identifying gaps in current health care provision and identify priorities for the development of engaging high-quality resources.
Results
578 participants who had completed at least 97% of the survey indicated that their menstrual cycle had negatively affected their mood or mental health. Three participants were excluded as optional free text responses indicated they were in the menopause or menopause transition. Of the remaining participants, 91.70% (n = 530) had complete data, and data from these participants were analysed (N = 530). Comparison groups for the current study were created using the PSST, which was composed of 20-items (α in the current sample = 0.93). 32.45% (n = 172) met the threshold for no or mild PMS, 46.79% (n = 248) met the threshold for moderate to severe PMS, and 20.75% (n = 110) met the threshold for PMDD.
Sociodemographic characteristics
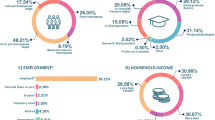
Participants’ sociodemographic information can be found in Table 1. The average age was 35.85 (SD = 7.28, range: 18–57), with the majority of respondents identifying as female (95.66%, n = 507), and being white (94.15%, n = 499). The majority of participants reported their highest educational attainment as at least an undergraduate degree (71.89%, n = 381) and were employed (either part-time, full-time, or self-employed; 83.02%, n = 440). Most participants had an annual household income, before tax, of between £35,001 and £65,000 (35.85%, n = 190) per annum.
A summary of group differences in sociodemographic characteristics can be found in Multimedia Appendix 1. There was a significant group difference in employment characteristics, with a higher proportion of individuals in full-time employment in the no or mild PMS group than both the moderate to severe and PMDD groups (χ2 = 11.82, df = 2, p = 0.003, φc = 0.15). No other significant group differences were observed.
Mental health characteristics
The mean WEMWBS score (α in the current sample = 0.93) across the whole sample was 40.95 (SD = 8.72). A one-way ANOVA revealed a significant difference in WEMWBS scores between all the groups (F(2, 527) = 22.70, p < .001, η2 = 0.08), with lowest wellbeing scores in the PMDD group (mean = 36.62, SD = 9.65) relative to both other groups. Further, significantly lower wellbeing scores were observed in the moderate to severe PMS group (mean = 41.09, SD = 7.45) than in the no or mild PMS group (mean = 43.51, SD = 8.71).
The entire sample endorsed at least one premenstrual symptom to at least a mild severity. The most frequently endorsed premenstrual symptoms screened for using the PSST in the overall sample were physical symptoms (e.g., breast tenderness, headaches; 96.42%; n = 511; Fig. 1) followed by psychological symptoms related to increased anger and irritability (95.85%, n = 508). The symptom most frequently reported as severe in the overall sample was fatigue/lack of energy (36.23%, n = 192). 97.17% (n = 515) of the overall sample stated that premenstrual symptoms had affected their functioning to at least a mild extent in at least one domain. The most frequent domain of functional impairment was in work/studies (83.40%, n = 442), with the most severely impaired domain reported as romantic or intimate relationships (15.85%, n = 84).
In the no or mild PMS group (Fig. 2), physical symptoms (e.g., breast tenderness, headaches) were the most frequently endorsed symptoms (93.02%, n = 160), with fatigue/lack of energy being most frequently endorsed as severe (11.05%, n = 19). The most frequent domain of functional impairment arising from premenstrual symptoms was work/studies (68.02%, n = 117). Social life was also the domain which was most frequently endorsed as being severely impacted (1.16%, n = 2).
In the moderate to severe PMS group (Fig. 3), the most frequently reported symptoms were anger irritability and tearfulness/sensitivity to rejection (99.19%, n = 246). The symptom most frequently endorsed as severe was fatigue/lack of energy (40.73%. n = 231). The most frequently impaired domain of functioning reported was home responsibilities (95.15%, n = 205), with the domain most endorsed as severe being romantic or intimate relationships (7.66%, n = 19).
In the PMDD group (Fig. 4), the most frequent symptom, endorsed by all individuals in this group (100%, n = 110), was anxiety/tension. The most frequently endorsed severe symptoms were depressed mood/hopelessness and tearfulness/increased sensitivity to rejection (70.91%, n = 78). The domain of functioning which was reported to be most frequently impaired was home responsibilities (98.18%, n = 108), and the most severely impaired domain of functioning being romantic or intimate relationships (58.18%, n = 64).
Significant group differences were observed in the frequency (Hs(2) ≥ 8.47, Ps ≤ 0.014, η2s ≥ 0.02) and severity (Hs(2) ≥ 22.91, Ps < 0.001, η2s ≥ 0.04) of premenstrual symptoms and associated functional impairment (Multimedia Appendix 1).
Significant differences were observed for the frequency of all symptoms between the no or mild PMS and the moderate to severe PMS groups, with the latter having a higher proportion of individuals who endorsed each PMS symptom (Us ≥ 12622.00, Ps ≤ 0.11, rs ≥ −0.12). Similarly, when comparing the frequency of premenstrual symptoms between the no or mild PMS and PMDD groups, the PMDD group had a higher proportion of individuals who endorsed each symptom (Us≥19950.00, Ps ≤ 0.019, rs ≥ 0.14), aside from physical symptoms, where no significant difference was observed (U = 8972.00, P = .052, r = −0.12). Significant differences were identified between the moderate to severe PMS and PMDD groups for the frequency of the following premenstrual symptoms: decreased interest in work (U = 12,568.00, P = 0.008, r = −0.14), home (U = 12,293.00, P = 0.002, r = −0.16) and social activities (U = 12,279.00, P = 0.001, r = −0.17), and in difficulty concentrating (U = 12,733.00, P = 0.018, r = −0.12).
With regard to differences in the frequency of severely reported symptoms between groups, both the moderate to severe PMS and PMDD groups more frequently reported severe symptoms than the no or mild PMS group for all symptoms (Us ≥ 3027.00, Ps ≤ .010, rs ≥ −0.14). Moreover, there were significant differences between the moderate to severe PMS and PMDD groups, with all symptoms more likely to have been reported as severe in the PMDD group than the moderate to severe PMS group (Us≥6168.00, Ps ≤ .034, rs ≥ 0.11).
Regarding the frequency of functional impairment, there were significant differences between the no or mild PMS group and both the moderate to severe PMS and PMDD groups, with the moderate to severe PMS and PMDD groups being more likely to endorse impairments in every domain of functioning relative to the no or mild PMS group (Us ≥ 5072.00, Ps < .001, rs ≥ −0.12). Between the moderate to severe PMS and PMDD groups, there were significant differences in the frequency of impairment in relationships with co-workers (U = 11,873.00, P = 0.017, r = −0.13) and home responsibilities (U = 12,953.00, P = 0.050, r = −0.10), with the PMDD group being more likely to have experienced impairment in these domains.
In terms of group differences in severe functional impairment, the moderate to severe PMS group had a higher proportion of individuals reporting severe impairment in the domains of family (U = 19,818.00, P < 0.001, r = −0.25) and home responsibilities (U = 20,592.00, P = 0.30, r = −0.48) relative to the no or mild PMS group. Furthermore, the PMDD group reported severe functional impairment in all domains more frequently than both the no or mild and the moderate to severe PMS groups (Us ≥ 4011.00, Ps < .001, rs ≥ −0.29).
Help-seeking characteristics
Data was collected on formal help seeking (i.e., through a HCP such as a National Health Service (NHS) GP) and online self-help seeking. In the overall sample, 64.91% (n = 344) had sought help (either only formal, only-online, or blended online and formal; Fig. 5). Overall, 35.09% (n = 186) of participants stated that they had visited a HCP to discuss their mental health symptoms in relation to their menstrual cycle. Furthermore, in the overall sample, 57.55% (n = 305) had searched online for help (Fig. 6). In the overall sample, 7.36% (n = 39) had only sought formal help, 29.81% (n = 158) had only sought online help, and 27.74% (n = 147) had sought both formal and online help.
A Proportion of online and formal help-seeking overall and in comparison groups, B breakdown of help-seeking behaviours in the overall sample (N = 530), C breakdown of help-seeking behaviours in the no or mild PMS group (n = 172), D breakdown of help-seeking behaviours in the moderate-to-severe PMS group (n = 248), E breakdown of help-seeking behaviours in the PMDD group (n = 110).
Within the groups, 47.67% (n = 82) of the no or mild PMS group, 66.94% (n = 166) of the moderate to severe PMS, and 87.27% (n = 96) of the PMDD group had sought help. A chi-squared test explored group differences in help-seeking behaviours, revealing significant group differences (χ2 = 79.21, df = 6, p < 0.001, φc = 0.39) in not seeking help and blended help-seeking. The proportion of those engaged in blended help-seeking increased with symptom severity, with the PMDD group having the highest proportion of blended help-seekers (55.45%, n = 61) compared to both the no or mild (25.81%, n = 64) and moderate to severe PMS (12.79%, n = 22) groups. Similarly, the highest proportion of those who had sought no help were the no or mild PMS group where symptom severity is lowest (52.33%, n = 90) as compared to the moderate to severe (33.06%, n = 82) and PMDD groups (12.73%, n = 14). There were no significant group differences between groups in the proportion of individuals who had only sought online or only sought formal help.
The most frequent type of help searched-for online (Fig. 6) was looking up mental health symptoms related to the menstrual cycle (85.57%, n = 261), followed by looking up information related to available treatment options (including therapy, counselling, and online cognitive behavioural therapy; 39.67%, n = 121), taking an online mental health test (34.43%, n = 105), and searching for relevant apps (33.44%, n = 102).
Group differences in the type of help sought online (n = 304) were explored using chi-squared tests. There were significant group differences in online searching for treatment options (χ2 = 9.79, df = 2, p = 0.007, φc = 0.18), looking online for a mental health assessment (χ2 = 7.92, df = 2, p = 0.019, φc = 0.16), looking online for peer support (χ2 = 12.79, df = 2, p = 0.002, φc = 0.21), and looking online for relevant apps (χ2 = 27.22, df = 2, p < 0.001, φc = 0.30). Specifically, a significantly higher proportion of the PMDD group had searched online for information on treatment options, an online mental health test, peer support, and relevant apps than both the no or mild and moderate to severe PMS groups.
Overall, regarding the quality of consultations with HCPs (n = 186), only 21.51% (n = 40) of participants stated that they felt their mental health symptoms related to the menstrual cycle were taken at least moderately seriously. 45.16% (n = 84) of participants who had visited a HCP stated that their mental health symptoms related to their menstrual cycle were not taken seriously at all, and a further 33.33% (n = 62) stated that they were only taken slightly seriously. No significant group differences were found for perceived quality of consultations with HCPs.
Discussion
The current study aimed to investigate the association of premenstrual symptoms on mental wellbeing and help-seeking patterns and experiences among those who self-reported experiencing menstrual-cycle-related mental health symptoms. Retrospectively identified premenstrual symptoms were frequent in the current sample, with the entire sample endorsing at least one symptom of at least a mild severity. Moreover, 97% of respondents experienced functional impairment in at least one domain. The estimated prevalence of PMS in the current sample of just over 47% is similar to previous estimates5. The estimated prevalence of PMDD is higher in the current study population at 20% when compared to estimates in previous reports16. There are several factors which may underpin this disparity in the prevalence of PMDD; firstly, evidence suggests that the PSST may overestimate the prevalence of PMDD when compared to prospective symptom tracking intended to establish the presence of premenstrual symptoms in two-consecutive menstrual cycles15. Secondly, the study may have been subject to recruitment bias, as individuals with more severe mental health symptoms associated with the menstrual cycle may have been more inclined to participate. These factors should be taken into consideration when interpreting the findings and extrapolating them to the wider UK population.
Regarding mental health characteristics, our findings indicate a link between mental wellbeing scores and the severity and burden of premenstrual symptoms, with individuals who screened positive for PMDD experiencing the lowest mental wellbeing scores. However, it should be noted that the current study did not control for other factors which may impact mental wellbeing. Additionally, it is possible that poor wellbeing could contribute to a higher PSST score, as such the directionality of the observed association between mental wellbeing and premenstrual symptoms cannot be conclusively determined in the current study. Despite this, previous work has reported an increased risk of engaging in emotional self-regulation through self-harm or substance use behaviours9, as well as an increased risk for suicidal ideation7,8. Considering the potential risk profile associated with PMS and PMDD, in addition to the potential impact on mental wellbeing observed in the current study, ensuring timely diagnosis and access to support and treatment is crucial. However, there is evidence of long waits to receive a diagnosis of PMDD, with a newly published report setting the UK’s PMDD research agenda citing waits of between 4 and 14 years10. Therefore, considering the reported delays to diagnosis9, the risk of poor mental wellbeing, and the reported years negatively affected due to being undiagnosed9, a formal PMDD diagnosis should not be a gatekeeper to accessing appropriate and evidence-based support.
The current study reveals patterns of help-seeking behaviours in individuals who experience mental health concerns in relation to their menstrual cycle, with around 65% having sought either online or formal help. Individuals who self-report mental health concerns related to their menstrual cycle were more likely to endorse having searched online for information and support, than through formal care pathways via a HCP. There were differences observed in help-seeking behaviours, with higher severity and burden of premenstrual symptoms in the PMDD group associated with increased utilisation of blended formal and online help-seeking, indicating a symptom severity threshold past which individuals feel they need to consult a healthcare professional. Moreover, it reveals an opportunity for clinician signposting and referral to high-quality online resources to supplement formal care for PMDD. However, concerningly, in the group who screened positive for PMDD, around 13% had sought no help at all. This indicates that there is a significant proportion of individuals who are not receiving or have not sought any support for their mental health symptoms related to the menstrual cycle despite endorsing high symptom severity and disease burden, potentially representing a significant amount of unmet clinical need and risk.
Almost sixty percent of the overall current sample had sought help online, with the proportion of online help-seekers in the PMDD group being almost eighty percent. The most frequent online searches were to look up mental health symptoms and to research treatment options. The majority of those who had sought help online, had looked up their mental health symptoms related to their menstrual cycle. This indicates that online searching is an easily accessible, and well accepted method of mental health information gathering and help-seeking. Given how frequently online information resources appear to be leveraged for self-help, it is important that quality audits of publicly available information are conducted, especially as in the Royal College of Obstetricians and Gynaecologists (RCOG) ‘Better for Women’ report, fifty-two percent of women surveyed stated that they considered online searches to be a reliable source for information17. However, trusted online resources for PMDD information may be hard to find. For instance, there is no dedicated page for PMDD on the NHS website, which is considered a trusted source of information by women in the UK13,17. Moreover, a review of available online resources for information on PMDD revealed that the quality is highly varied, and that comprehensive content is often lacking18. The review determined that no websites identified during searches were rated excellent in terms of both general quality (including domains such as usability, authorship, ownership transparency) and the quality of information provided about PMDD, with risks of inaccurate or out-of-date information. Considering that most women who experience PMS receive the initial suggestion of the condition from a non-medical source19 and that many self-diagnose prior to obtaining a formal diagnosis20, it is vital that sources of information are accurate. Such resources should enable individuals to self-assess whether the diagnostic label accurately describes their symptoms, allowing them to make well-informed decisions about seeking support and pursuing a formal diagnosis and treatment. With the potential for the landscape of online spaces such as websites to rapidly change, the re-review of such resources should be a priority. Re-reviews should examine the current risk of misinformation and identify reliable resources. Identifying high-quality online resources and potentially creating a dedicated database would be helpful to both individuals who engage in self-initiated online searching and clinicians for signposting patients to additional information.
Additionally, many individuals surveyed within the current study reported having looked online for treatment information. Effective treatments for PMS and PMDD are available21, with current treatment recommendations including exercise, Selective Serotonin Uptake Inhibitors (SSRIs), combined oral contraceptives, and Cognitive Behavioural Therapy (CBT) as potential first-line treatment options22. Prescribing patterns in the UK indicate that prescriptions of SSRIs and combined oral contraceptives are commonplace for PMS23. Non-pharmacological treatments, such as CBT, appear to be effective for premenstrual symptoms, demonstrating improvement in symptoms, which are sustained over time with no recorded side-effects24. Such non-pharmacological interventions can be effectively adapted for digital delivery and have been demonstrated to be acceptable25 and effective in other mood disorders such as Major Depressive Disorder26. Early evidence demonstrates that digital interventions, specifically internet-delivered CBT, are effective in both PMS27 and PMDD28 in reducing symptom severity and alleviating symptom burden. Given the frequency of online searches for treatment information online, alongside the effectiveness of digitally delivered non-pharmacological treatments, there is a potential to widen access to evidence-based psychological support. This can be achieved by offering such support digitally to individuals who are actively searching online for treatment information, where appropriate. This would offer those experiencing mental health symptoms related to the menstrual cycle a sense of self-efficacy, by utilising digital psychological interventions either independently in milder presentations or as an adjunct to formally delivered psychological or pharmacological treatment in more severe presentations. Moreover, similarly to other digitally delivered psychological interventions29, it would provide individuals experiencing mental health symptoms related to the menstrual cycle the opportunity to conveniently access treatment resources. Additionally, this would address potential barriers to help-seeking such as concerns of potential stigma28 and allow for easy re-access to such tools when needed during successive menstrual cycles.
Whilst there appears to be interest in online resources for help-seeking in those who experience mental health symptoms related to the menstrual cycle, such resources are not a replacement for formal care, especially for more severe symptom presentations. Within the overall current sample, around thirty-five percent had sought formal help for their premenstrual symptoms. The proportion of individuals seeking formal help was higher in the moderate to severe PMS and PMDD groups, indicating that increased symptom severity and burden are factors that drive individuals to seek professional support, corroborating previous findings30. However, it is worth noting that even in the PMDD group, characterised by the most severe symptoms, around thirty percent had not sought formal help, meaning that there may be a significant proportion who are not receiving appropriate medical support. A barrier to formal help-seeking in those who experience mental health symptoms related to the menstrual cycle regards symptoms being considered “normal” and not warranting formal care31. This sentiment is expressed frequently even in those who screen positive for PMDD31, and individuals with more severe symptoms tend to believe that treatment would not be effective30. In addition, it is well documented that women frequently do not feel acknowledged or taken seriously by HCPs13, with both anecdotal and research evidence of perceived negative or even dismissive attitudes32. This perception of dismissive attitudes is also reported by those who have sought help specifically for PMS and PMDD symptoms9. Concerningly, a perception of premenstrual symptoms not being taken seriously or a lack of confidence in the ability of a HCP to accurately identify and offer effective support was cited as a barrier to formal help-seeking33. In the current study, one concerning finding was the perception of interactions with HCPs when seeking formal support for mental health symptoms related to the menstrual cycle. Just under eighty percent of participants who’d sought formal help reported that they felt as though their HCP took their concerns only slightly seriously or not seriously at all. These findings align with previous research where women diagnosed with PMDD reported that HCPs frequently fail to acknowledge or address their condition, despite having a formal diagnosis9. Consequently, these individuals often feel that their symptoms are not taken seriously or even dismissed by their HCP9.
There are some limitations of the current study which should be considered alongside the findings. Firstly, a retrospective screening approach was used to determine prevalence estimates of PMS and PMDD, this will have most likely introduced bias in the current sample, when compared to prospective symptom tracking across at least two consecutive menstrual cycles15. However, the PSST was deemed a suitable tool for screening and research application as longitudinal prospective PMS symptom tracking is associated with non-engagement and drop-out15. Additionally, given that the sample was comprised of individuals reporting mental health symptoms related to the menstrual cycle, the estimated incidence of PMS and PMDD will likely be higher in the current study than in the general UK population. Therefore, the estimated incidence of PMS and PMDD reported in the current study should be viewed as information to contextualise the study findings. The figures do not reflect the true prevalence rate in the wider population.
Furthermore, due to the primary method of recruitment via social media, individuals surveyed are more likely to be digitally literate and so perhaps more likely to use digital methods such as online searches for self-help. Additionally, some evidence indicates that online health resources are potentially more accessible to individuals from well-educated and high-earning groups34. Considering the current sample was predominantly comprised of individuals from these groups (with the majority of the sample holding at least an undergraduate degree and earning above £35,000) the proportion of online help-seekers may have been over-represented in our sample.
In summary, the current study further establishes an association between premenstrual symptoms, functional impairment and poorer mental wellbeing. Additionally, the findings provide insights into which online resources are deemed useful by those who experience mental health symptoms related to the menstrual cycle, informing opportunities for resource development. Given the reported widespread use of online resources as sources of mental health information, there is a need to undertake reviews of publicly available online information to ascertain quality, prevent misinformation, and maximise clinical effectiveness both outside and alongside formal care. Concurrently, more work is needed to understand the barriers to accessing help either via a HCP or self-initiated online searches, given the significant proportion of individuals not seeking help identified in this study. The current findings corroborate previous reports regarding negative perceptions of care interactions with HCPs, emphasising the need to increase HCP awareness and training to improve the time to diagnosis and to ensure attentive care experiences for premenstrual symptoms.
Methods
Participants
Recruitment was conducted between January 2023 and March 2023 via paid Facebook and Instagram advertisements, posts on the Cambridge Centre for Neuropsychiatric Research (CCNR) Facebook and Twitter pages, and Reddit. Additionally, individuals who had previously participated in CCNR research studies and expressed openness to being recontacted for future studies were contacted via email. The content of recruitment materials primarily emphasised a focus on mental healthcare throughout the menstrual cycle for individuals who have had a period. Inclusion criteria for the study were:(1) ≥ 18 years, (2) UK residence, (3) must have had a period and self-describe as premenopausal (i.e., no significant change to menstrual bleeding patterns, unless changes are caused by contraception), and (4) not currently pregnant or breastfeeding.. Participants did not have to have been diagnosed with a mental health condition to take part in the study. There were no other inclusion criteria. Due to the adaptive nature of the survey, only individuals who endorsed their mental health being affected by their menstrual cycle were asked about formal help seeking for such symptoms. Therefore, only those who endorsed experiencing mental health symptoms related to their menstrual cycle were included in the analysis. Participants were invited to enter their email for the chance to win one of three £50 (US $60) Highstreet vouchers.
Materials and procedure
An anonymous online survey was created using Qualtrics XM®. The survey could be completed in 15–20 min and comprised four sections: (1) socio-demographic information, (2) mental health characteristics including the premenstrual symptoms screening tool (PSST; 14) and the Warwick Edinburgh Mental Wellbeing Scale (WEMWBS; 35) (3), help-seeking characteristics, and (4) perspectives toward, interest in, and preferences regarding using digital technology for mental health symptoms related to the menstrual cycle. Data from section 4 of the survey were not included in the current analysis and are in preparation for a future publication. The survey was adaptive in nature, such that only relevant questions were asked based on previous responses. The survey questions and accompanying study materials were designed in consultation with an experienced psychiatrist (SB).
The PSST is a screening tool for premenstrual symptoms14 composed of 19 items measuring the presence and severity of premenstrual symptoms, and associated functional impairment in a range of domains, to indicate PMS and PMDD. As disruption to relationships with partners is a frequent functional consequence of PMDD36, a further item was added to examine whether the symptoms had interfered in romantic or intimate relationships, taking the total number of items up to 20. Items in the PSST are scored on a 4-point scale, ranging from ‘Not at all’ to ‘Severe’. The PSST was scored using the scoring instructions of Steiner et al (2003; 14), which reflect the diagnostic criteria for PMDD from the diagnostic statistical manual (DSM-IV; 37). To screen for PMDD, at least one core symptom must be rated as severe with a further 4 symptoms rated as moderate to severe, with associated severe impairment reported in at least one domain of functioning. To screen for moderate to severe PMS, at least one core symptom must be rated moderate to severe with a further 4 symptoms rated as moderate to severe, with associated moderate to severe impairment reported in at least one domain of functioning. Any individuals not meeting either of these scoring criteria were labelled as no or mild PMS.
The WEMWBS35 is a 14-item scale of wellbeing. Each item in the WEMWBS is scored on a 5-point scale, ranging from 1=’None of the time’ to 5=’All of the time’. The minimum score of the WEMWBS is 14 and the maximum score is 70, with a higher score indicating higher mental wellbeing.
Data analysis
Comparison groups were determined using the PSST. The internal consistency of the PSST and WEMWBS was examined with Cronbach’s alpha. Group differences in normally distributed continuous variables were explored using one-way ANOVAs, and effect sizes were calculated as eta-squared (η2; small ≥0.01, medium ≥0.06, large ≥0.14; 39). Where indicated, a Bonferroni correction was conducted for multiple comparisons. Group differences in ordinal data and non-normally distributed continuous data were investigated using Kruskal Wallis tests, with effect sizes are reported as eta-squared (η2; small ≥0.01, medium ≥0.06, large ≥0.14; 38). Where indicated, Mann–Whitney U tests, subject to the Bonferroni correction method, were conducted post-hoc to check for multiple comparisons. Group differences in categorical variables were explored using chi-square tests, and effect sizes were calculated as Cramer’s V (φc; small ≤0.10, medium ≤0.30, large ≤0.50; 38).
Descriptive data analyses (i.e., frequencies and percentages) were analysed and processed in Excel, version 22006 (Microsoft Office 365). Cronbach’s alpha for internal consistency and the tests for group comparisons (i.e., one-way ANOVAs, Kruskall wallis and Chi squared tests) and associated post-hoc tests were conducted in SPSS, version 28.0.1.1. Figures were created using Excel version 2206 and PowerPoint version 2206 (Microsoft Office 365).
Data availability
The data that support the findings of this study are available from the corresponding author, S.B., upon reasonable request.
References
Ryu, A. & Kim, T.-H. Premenstrual syndrome: a mini review. Maturitas 82, 436–440 (2015).
Halbreich, U., Borenstein, J., Pearlstein, T. & Kahn, L. S. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology 28, 1–23 (2003).
Dennerstein, L., Lehert, P. & Heinemann, K. Epidemiology of premenstrual symptoms and disorders. Menopause Int. 18, 48–51 (2012).
Rapkin, A. J. & Winer, S. A. Premenstrual syndrome and premenstrual dysphoric disorder: quality of life and burden of illness. Expert Rev. Pharmacoecono. Outcomes Res. 9, 157–170 (2009).
Direkvand-Moghadam, A., Sayehmiri, K., Delpisheh, A. & Kaikhavandi, S. Epidemiology of Premenstrual Syndrome (PMS)-a systematic review and meta-analysis study. J. Clin. Diagnos. Res. 8, 106–109 (2014).
Hardy, C. & Hunter, M. S. Premenstrual symptoms and work: exploring female staff experiences and recommendations for workplaces. Int. J. Environ. Res. Public Health 18, Article 7 (2021).
Prasad, D., Wollenhaupt-Aguiar, B., Kidd, K. N., De Azevedo Cardoso, T. & Frey, B. N. Suicidal risk in women with premenstrual syndrome and premenstrual dysphoric disorder: a systematic review and meta-analysis. J. Women’s Health 30, 1693–1707 (2021).
Wikman, A. et al. Prevalence and correlates of current suicidal ideation in women with premenstrual dysphoric disorder. BMC Women’s Health 22, 35 (2022).
Osborn, E., Wittkowski, A., Brooks, J., Briggs, P. E. & O’Brien, P. M. S. Women’s experiences of receiving a diagnosis of premenstrual dysphoric disorder: a qualitative investigation. BMC Women’s Health 20, 242 (2020).
Matthews, L., Riddell, J. Premenstrual Dysphoric Disorder (PMDD): The UK research agenda. University of the West of Scotland. www.uws.ac.uk/pmdd. (2023)
Studd, J. Severe premenstrual syndrome and bipolar disorder: A tragic confusion. Menopause Int. 18, 82–86 (2012).
Freeman, E. W. Premenstrual syndrome and premenstrual dysphoric disorder: definitions and diagnosis. Adapted from the symposium on premenstrual syndrome and premenstrual dysphoric disorders, July 17, 2000, Rhodes, Greece. Psychoneuroendocrinology 28, 25–37 (2003).
Department of Health & Social Care. Women’s Health Strategy for England. Department of Health & Social Care. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1100721/Womens-Health-Strategy-England-web-accessible.pdf. (2022).
Steiner, M., Macdougall, M. & Brown, E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch. Women’s Mental Health 6, 203–209 (2003).
Henz, A. et al. Premenstrual syndrome diagnosis: a comparative study between the Daily Record of Severity of Problems (DRSP) and the Premenstrual Symptoms Screening Tool (PSST). Revista Brasileira de Ginecologia e Obstetrícia/RBGO Gynecol. Obstetrics 40, 20–25 (2018).
Tschudin, S., Bertea, P. C. & Zemp, E. Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch. Women’s Mental Health 13, 485–494 (2010).
Royal College of Obstetricians & Gynaecologists. Better for women: Improving the health and wellbeing of girls and women. Royal College of Obstetricians & Gynaecologists. https://www.rcog.org.uk/media/h3smwohw/better-for-women-full-report.pdf. (2019)
Hardy, C. & Sillence, E. What are women being exposed to? A review of the quality, content and ownership of websites on premenstrual dysphoric disorder. Women’s Health Issues 26, 183–189 (2016).
Kraemer, G. R. & Kraemer, R. R. Premenstrual syndrome: diagnosis and treatment experiences. J. Women’s Health 7, 893–907 (1998).
Chan, K., Rubtsova, A. A. & Clark, C. J. Exploring diagnosis and treatment of premenstrual dysphoric disorder in the U.S. healthcare system: a qualitative investigation. BMC Women’s Health 23, 272 (2023).
Carlini, S. V., Lanza Di Scalea, T., McNally, S. T., Lester, J. & Deligiannidis, K. M. Management of premenstrual dysphoric disorder: a scoping review. Int. J. Women’s Health ume 14, 1783–1801 (2022).
Green, L. J., O’Brien, P. M. S., Panay, N. & Craig, M., on behalf of the Royal College of Obstetricians and Gynaecologists. Management of Premenstrual Syndrome. BJOG: An Int. J. Obstetrics Gynaecol. 124, e73–e105 (2017).
Sammon, C. J., Nazareth, I., & Petersen, I. Recording and treatment of premenstrual syndrome in UK general practice: A retrospective cohort study. BMJ Open, 6. https://doi.org/10.1136/bmjopen-2015-010244 (2016).
Landolt, N. K., & Ivanov, K. Short report: Cognitive behavioral therapy - a primary mode for premenstrual syndrome management: systematic literature review. Psychol. Health Med. https://doi.org/10.1080/13548506.2020.1810718 (2020).
Rost, T. et al. User acceptance of computerized cognitive behavioral therapy for depression: systematic review. J. Med. Internet Res. 19, e7662 (2017).
Kambeitz-Ilankovic, L. et al. A systematic review of digital and face-to-face cognitive behavioral therapy for depression. Npj Digital Med. 5, Article 1 (2022).
Borji-Navan, S., Mohammad-Alizadeh-Charandabi, S., Esmaeilpour, K., Mirghafourvand, M. & Ahmadian-Khooinarood, A. Internet-based cognitive-behavioral therapy for premenstrual syndrome: a randomized controlled trial. BMC Women’s Health 22, 5 (2022).
Weise, C. et al. Internet-based cognitive-behavioural intervention for women with premenstrual dysphoric disorder: a randomized controlled trial. Psychother. Psychosomatics 88, 16–29 (2019).
Webb, C. A., Rosso, I. M. & Rauch, S. L. Internet-based cognitive-behavioral therapy for depression: current progress and future directions. Harvard Rev. Psychiatry 25, 114 (2017).
Hylan, T. R., Sundell, K. & Judge, R. The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: experience from the United States, United Kingdom, and France. J. Women’s Health Gender-Based Med. 8, 1043–1052 (1999).
Lete, I. et al. Attitudes of Spanish women toward premenstrual symptoms, premenstrual syndrome and premenstrual dysphoric disorder: Results of a nationwide survey. Eur. J. Obstet. Gynecol. Reprod. Biol. 159, 115–118 (2011).
Winchester N. 2021, July 01. Women’s health outcomes: Is there a gender gap? House of Lords Library. https://lordslibrary.parliament.uk/womens-health-outcomes-is-there-a-gender-gap/.
Labots-Vogelesang, M. S., Kooiman-Andringa, R., Teunissen, T. A. M. & Lagro-Janssen, A. L. M. Perspectives of Dutch women on premenstrual disorder. A qualitative study exploring women’s experiences. Eur. J. General Pract. 29, 2166033 (2023).
Luo, A. et al. The effect of online health information seeking on physician-patient relationships: systematic review. J. Med. Internet Res. 24, e23354 (2022).
Tennant, R. et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Quality Life Outcomes 5, 63 (2007).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Publishing, Inc. (2022).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.). American Psychiatric Publishing, Inc. (1994).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences. Academic Press. (2013).
Acknowledgements
We are thankful to the participants who contributed time and data to the current study. This study was funded by the Stanley Medical Research Institute (grant number 07R-1888).
Author information
Authors and Affiliations
Contributions
E.L.F., N.A.M.-.K., B.S. and S.B. conceived the study focus and materials. E.L.F. coordinated and conducted participant recruitment. Data analysis was performed by E.L.F. E.L.F. and N.A.M.-K. prepared the manuscript with revisions from B.S. and S.B. All authors contributed to the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
Author S.B. holds shares in Psynova Neurotech Ltd and Psyomics Ltd but declares no non-financial competing interests. Author E.L.F. is a paid consultant for Psyomics Ltd but declares no non-financial competing interests. Authors N.A.M.-K. and B.S. declare no financial or non-financial competing interests.
Ethical approval and informed consent
The study was approved by the University of Cambridge Human Biology Research Ethics Committee (approval number PRE.2022.110). All participants provided informed consent to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Funnell, E.L., Martin-Key, N.A., Spadaro, B. et al. Help-seeking behaviours and experiences for mental health symptoms related to the menstrual cycle: a UK-wide exploratory survey. npj Womens Health 2, 2 (2024). https://doi.org/10.1038/s44294-023-00004-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44294-023-00004-w