Abstract
Despite a higher risk of cardiovascular disease (CVD) events in women cancer survivors than their male counterparts, importance of female sex has been underestimated due to under-representation of women in clinical research and male dominant CVD risk models. This study examined ten-year Atherosclerosis Cardiovascular Disease (ASCVD) risk trajectories in women veterans diagnosed with the ten most common cancers—bladder, breast, colorectal, endometrial/uterine/cervix, leukemia, liver, lung and bronchium, Non-Hodgkin’s lymphoma, melanoma, and thyroid cancer—using United States (US) Veterans Affairs (VA) Electronic Health Records data. The study included 78,556 women veterans aged between 30 and 80 years from diverse backgrounds treated at VA hospitals with ≥2 complete outpatient visit records in the VA health care system between January 01, 2007 and December 31, 2017. A steep rise in ASCVD risk score trajectories post-cancer diagnosis was observed among women diagnosed with bladder, breast, liver, lung and thyroid cancer, melanoma, and Non-Hodgkin’s lymphoma, compared to pre-cancer diagnosis periods, as well as significantly elevated pre-cancer ASCVD risk among all patients with cancer, other than thyroid cancer, compared to the no cancer group (p < 0.0001). ASCVD risk monitoring is highly recommended to reduce adverse cardiovascular events for women diagnosed with cancer, survivors, and for women at risk of future cancer incidences.
Similar content being viewed by others
Introduction
Advances in early detection and treatment of cancer have not only improved survival rates for patients diagnosed with cancer, but also resulted in the emergence of a new collaborative area, cardio-oncology. Cancer survivors are at an increased risk of cardiovascular disease (CVD) and have higher rates of mortality from CVD than those without a history of cancer1. This may be accounted for by the shared predisposed risk factors (i.e., smoking/tobacco use, obesity) between cancer and CVD, as well as the late effect or long-term side effect of certain cancer treatments2. Particularly, the association between cancer diagnosis and increased risk of CVD was stronger for women cancer survivors than their male counterparts3. In addition, sex-specific cardio-oncology is of particular interest due to sex differences in the safety and efficacy of cancer drugs.
The current guidelines recommend using traditional Atherosclerosis Cardiovascular Disease (ASCVD) risk stratification for cardio-oncology practice4,5; however, the evidence from existing literature remains weak on assessing the risk of ASCVD events specifically among women diagnosed with cancer.
Despite rising interest in sex-specific cardio-oncology, the current literature on female sex-specific research has been limited to non-ASCVD events, such as heart failure and cardiomyopathies, among patients diagnosed with breast cancer. Breast cancer is the most common type of cancer in women and therefore has received considerable attention in sex-specific cardio-oncology research6,7,8. Breast cancer survivors were reported to have a greater incidence of developing heart failure, atrial fibrillation/flutter, and cardiac arrhythmias compared to those not diagnosed with cancer7,9. However, the current evidence of elevated CVD risk with an increasing risk of hard ASCVD events, such as myocardial infarction (MI) and stroke, in women diagnosed with cancer is rather limited and inconsistent. In addition, there is a lack of research on CVD risk for women with other types of cancers, beyond breast cancer.
The paucity of research may be due to women being under-studied despite known metabolic and female sex-specific factors—metabolic syndrome during post menopause10, timing of first menstruation11, reproductive history12, types and duration of hormone replacement therapy13, and adverse pregnancy outcomes14. Furthermore, certain cancer drugs15 used to treat female breast cancer are known to be associated with an increase in cardiac adverse events16. Thus, evidence from large-scale, data sets representing females are much needed to support the current guidelines for cardio-oncology practice.
To address these questions, this study used the Veterans Administration (VA) electronic health records (EHR) data—the largest longitudinal EHR data available in the United States—and examined 10-year ASCVD risk score trajectories in women veterans diagnosed with ten of the most common cancer diagnoses in women veterans. We hypothesize CVD risk among women diagnosed with cancer is greater than women without cancer due to not only predisposed shared risk factors but also cancer treatment and its cardiotoxicity. Thus, we expect elevated ASCVD risk among women diagnosed with cancer and a change of ASCVD risk score trajectories after cancer diagnosis when cancer treatment is initiated.
Methods
The study selected 78,556 women veterans aged between 30 and 80 years treated at VA hospitals with ≥2 complete outpatient visit records in the VA health care system between January 01, 2007 and December 31, 2017. Table 1 depicts baseline characteristics of the study cohort.
The study was designed to test the hypothesis that a diagnosis of any of 10 cancer types is independently associated with increased cardiovascular risk based on calculated ASCVD risk scores.
The ten-year ASCVD risk scores at all available visits per patient were calculated using both the VA women CVD risk score calculator17, and the American College of Cardiology (ACC/AHA) American Heart Association ASCVD risk score18. The VA women CVD risk score is a new ASCVD risk score that was developed and validated using women veteran cohorts of Non-Hispanic (N-H) White, N-H Black, and Hispanic women between 30 and 79 years of age17. The ACC/AHA ASCVD risk score was based on data for only N-H White and N-H Black women between ages of 40 and 79. Both the VA women CVD risk and ACC/AHA ASCVD risk scores are sex- and race-specific. ASCVD risk includes hard adverse events of MI, ischemic and hemorrhagic stroke, cardiac arrests, and cardiac death.
The VA women CVD risk score is a non-linear weighted sum of estimated risks of age, systolic blood pressure, total and high density lipoprotein (HDL) cholesterol, presence of Diabetes mellitus, current smoking status, and major depression. The ACC/AHA ASCVD score includes the same set of risk factors, but excludes major depression and adds a squared age term in the N-H White women model only. The VA women CVD risk score was developed and obtained estimated risks using a women veteran cohort, while the ACC/AHA ASCVD score’s development cohort is from pooled data of four epidemiology data sets18,19. Both risk scores were used in this study to examine ASCVD risk in order to better ascertain impact of cancer diagnosis and remove possibility of measurement bias.
Definitions and validation of patients with cancer
The study considered the ten most prevalent cancers among women veterans except kidney cancer. The study defined and validated cancer diagnoses using both International Classification of Diagnosis (ICD) 9 and 10 codes following VA Centralized Interactive Phenomics Resource disease and phenotype definitions20 and EHR chart reviews. For each selected type of cancer, this study utilized two approaches to identify patients with new cancer diagnosis during the study period: (1) ICD 9 and 10 codes from the primary diagnoses were used first and then validated by reviewing outpatient visit charts and (2) review of oncology progress notes. Both outpatient and oncology chart reviews were conducted (1) using Natural Language Processing (NLP) to extract narrative features of each cancer following algorithms developed by the Million Veterans Program data core team21, and (2) followed by manual reviews of extracted narratives. The final set of patients with cancer diagnoses were created by a union of the two data sets created by approaches 1 and 2 above. The chart reviews of patients were conducted iteratively until at least 2 consecutive visit records confirmed the cancer diagnoses per patient (Table 1, ICD 9 and 10 codes and NLP codes for each cancer diagnosis definition).
For example, the final study cohort of patients with breast cancer was determined by joining two data sets extracted using (1) validated cancer diagnoses of ICD 9 and 10 codes by outpatient chart reviews and (2) oncology charts. (1) The study extracted all patients with ICD 9 (174., 175.9, 233.0, V10.3) and 10 codes (C50., D05., Z85.2, Z85.3) and manually reviewed charts of these patients that contained exact or abridged text terms of “diagnosis of breast cancer” or a text of “breast cancer” with an exclusion of any text exact or abridged terms including “family history of breast cancer” and “in situ” using NLP algorithm from VA national Corporate Data Ware house (CDW). This was repeated with modifications of NLP per each extraction followed by manual chart reviews for patients with at least two consecutive visit records until emerging patterns of NLP confirm breast cancer diagnosis. (2) The study separately extracted patients diagnosed with new breast cancer from oncology notes under the chart documents titled “oncology” or “Breast Ca” and searched progress notes containing narrative texts of “Breast Ca.” Of these, the study excluded charts including narrative texts of family history of breast cancer (See Table 1 for other cancers).
Statistical analysis
We used Generalized Linear Mixed model (GLMM) with unstructured covariance structure to estimate the 10-year ASCVD risk score trajectory for each cancer type. Covariates of the GLMM model include: a cancer diagnosis, time (follow up months, outpatient visits), and an interaction term of both cancer diagnosis and time. An intercept and cancer diagnosis were considered to estimate random effects. Following regression discontinuity approach22,23, the linear estimates of the 10-year ASCVD risk score trajectories for each cancer type were then plotted and partitioned by pre- and post-cancer periods with discontinuity at an average onset against an estimated ASCVD risk score trajectory of patients without cancer. In addition, Z statistics was used to test whether linear estimates, intercepts (α) and slope parameters (β), of cancer groups statistically differ from no cancer group and between pre- and post-cancer within the cancer group.
This study was designated exempt by the VA North Texas Institutional Review Board (IRB), approved by the VA North Texas Research and Development Committee, and supported using data from the VA Corporate Data Warehouse. The VA North Texas IRB waived the requirement to obtain informed consents from study subjects.
Because of the sensitive nature of the data collected for this study, requests to access the dataset are limited to qualified VA-affiliated researchers trained in human subject confidentiality. Protocols may be sent to the VA North Texas Health Care System IRB at NTXIRBAdmin@va.gov. SQL and SAS code used in the analysis of this study are available from the corresponding author upon reasonable request. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Cancer incidences
Of the 78,556 women veterans examined during the ten-year follow up period, 49 women were newly diagnosed with bladder cancer (onset, [mean ± SD] 70.60 ± 44.26 follow-up months), 1951 with breast cancer (onset, 63.57 ± 40.78 months), 144 with colorectal cancer (onset, 67.09 ± 38.40 months), 76 with endometrial/uterine/cervix cancer (onset, 66.84 ± 36.48 months), 113 with leukemia (onset, 64.09 ± 42.56 months), 21 with liver cancer (onset, 92.33 ± 30.49 months), 450 with lung and bronchium cancer (onset, 62.66 ± 41.50 months), 16 with Non-Hodgkin’s lymphoma (onset, 74.13 ± 42.94 months), 37 with melanoma (onset, 76.26 ± 39.93 months), and 319 with thyroid cancer (onset, 66.02 ± 41.61 months). During the same ten-year follow-up timeframe, 76,105 women veteran patients did not develop any cancer of interest.
Study cohort
Table 2 depicts characteristics of the study cohort. Forty-six percent of the participants (n = 36,172) were N-H White women, 37% (n = 29,231) N-H Black, 5% (n = 4171) Hispanic, and 11.4% (n = 8982) other race (Asian, American Indians, and Pacific Islanders). Women on average were 45 years old, with a standard deviation (SD) of 8.5 years, at baseline.
Overall ten-year ASCVD risk trajectories
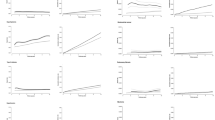
Figure 1 shows the ten-year ASCVD risk score trajectory measured by VA women CVD risk score for each cancer group against a no cancer group (black solid line; intercept 8.3%, slope 0.004; Supplementary Table 1). Discontinuity/kink at the cut-off points of cancer groups’ ASCVD risk score trajectories (pre-cancer vs. post-cancer) mark the average onset of cancer.
A-J depict ten cancer groups: A bladder, B breast, C colorectal, D endometrial/uterine, E leukemia, F liver, G lung, H melanoma, I non-Hodgkin’s (NH) Lymphoma, and J thyroid. Lines represent linear trajectories of ASCVD risk for 10-year follow-up. Discontinuity/kink of trajectories mark average onset of cancer diagnosis. Blue lines are pre-cancer, red lines for post-cancer, and black lines for no cancer. Gray lines marked projected trajectories without cancer onset.
Overall, ASCVD risk score trajectories among women veterans newly diagnosed with cancer during the 10-year follow up showed a faster rate of increase in ASCVD risk than women veterans without cancer during both pre- and post-cancer diagnosis.
Pre-cancer ten-year ASCVD risk trajectories
Before cancer diagnosis (pre-cancer), the ASCVD risks of all patients with cancer (blue lines, Fig. 1), other than thyroid cancer, were significantly elevated compared to the no cancer group (black lines in Fig. 1; Supplementary Table 1). Also, a pre-cancer aging propensity of ASCVD risk in colorectal, endometrial, lung cancer, and melanoma patients was higher than patients without cancer. Patients diagnosed with colorectal, endometrial, lung cancer, and melanoma showed greater ASCVD risk even before cancer diagnosis compared to patients not diagnosed with cancer (steeper blue lines than black lines in Fig. 1; slopes pre-cancer were greater than 0.0004; P < 0.0001, Supplementary Table 1).
Changes in post-cancer ten-year ASCVD risk trajectories
It is noteworthy that ASCVD risks among women with bladder, breast, liver, lung, melanoma, Non-Hodgkin’s lymphoma, and thyroid cancer (seven of the ten cancers examined) were accelerated after cancer diagnosis (post-cancer; Fig. 1; slopes post-cancer greater than slopes pre-cancer, Supplementary Table 1), with liver and thyroid cancer reaching statistical significance, p value < 0.05.
The ASCVD risk among patients diagnosed with colorectal cancer was greater pre-cancer diagnosis, compared to patients without cancer, and continued to increase at a similar rate post-cancer diagnosis (Fig. 1C; Supplementary Table 1), while a decrease in ASCVD risk post-cancer was observed among women veterans diagnosed with endometrial/uterine/cervix cancer (Fig. 1D) and Leukemia (Fig. 1E; Supplementary Table 1).
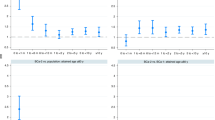
Using the ACC/AHA ASCVD risk scores (Fig. 2), the study found similar results compared to the VA women CVD risk score. On average, the VA women CVD risk score estimated ASCVD risk of women veterans about 2.5% higher than the ACC/AHA ASCVD risk scores.
A–J depict ten cancer groups: A bladder, B breast, C colorectal, D endometrial/uterine, E leukemia, F liver, G lung, H melanoma, I non-Hodgkin’s (NH) lymphoma, and J thyroid. Lines represent linear trajectories of ASCVD risk for 10-year follow-up. Discontinuity/kink of trajectories mark average onset of cancer diagnosis. Blue lines are pre-cancer, red lines for post-cancer, and black lines for no cancer. Gray lines marked projected trajectories without cancer onset.
Discussion
There is a dearth of large-, diverse observational studies investigating ASCVD risk for women diagnosed with cancer beyond breast cancer. This study is one of the few that investigated ten-year ASCVD risk among women diagnosed with cancer before and after their cancer diagnosis. Using the US VA CDW data, the present study examined ASCVD risk associated with the top ten cancers—bladder, breast, colorectal, endometrial/uterine/cervix, leukemia, liver, lung and bronchium, Non-Hodgkin’s lymphoma, melanoma, and thyroid cancer— in women veterans aged between 30 and 80 years from diverse racial, socioeconomic and ethnic backgrounds. Aligning with US cancer prevalence rates, breast cancer was by far the most common cancer type among women veterans in the current study.
This study’s finding, escalation of ASCVD risk post-cancer among women diagnosed with seven cancer types (bladder, breast, liver, lung, melanoma, Non-Hodgkin’s lymphoma, and thyroid), serves as evidence supporting current guidelines’ CVD risk stratification and the use of existing ASCVD risk scores to assess and monitor CVD risk for women patients undergoing cancer treatment24,25.
The study found that female veterans diagnosed with cancer had significantly elevated ASCVD risk during the pre-cancer diagnosis period as well. This is likely due to the increasingly recognized shared pre-disposing risk factors between cancer and ASCVD26. Thus, women at higher risk of cancer incidence are also at a higher risk of ASCVD, suggesting that ASCVD risk factors, such as metabolic syndrome and fatty liver, are commonly associated with cancer and ASCVD. All female veteran patients diagnosed with cancer, except liver cancer (a downward slope in Figs. 1 and 2; Supplementary Table 1), showed evidence of greater ASCVD risk long before their cancer diagnosis (upward and steeper blue lines than the black lines of no cancer group in Figs. 1 and 2). These findings suggest that women patients being monitored for ASCVD risk may benefit from shared risk reduction strategies coupled with heightened cancer screening to aid in the early detection of cancer.
Most of the existing literature on female sex-specific cardio-oncology focuses on breast and endometrial/ovarian cancer, reporting increased risk of certain CVD events24, such as heart failure6,25, cardiac arrhythmias, cardiomyopathy7,8, thromboembolism27, atrial fibrillation/flutter28, and pulmonary heart disease29. Though guidelines recommend using the ACC/AHA ASCVD risk score for cardio-oncology practice, the evidence from existing literature remains weak on increased risk of hard ASCVD events including MI, stroke, and cardiac deaths, among women diagnosed with cancer. Additionally, there is lack of longitudinal data on cardiovascular outcomes and complications of women with cancer before and after cancer diagnosis to understand the epidemiology of CVD risk among female patients with cancer. Given the fact that CVD is the leading cause of death among women, it is important to monitor and manage CVD risk factors before and after cancer diagnosis.
A recent epidemiologic study investigating CVD risk factors in women diagnosed with breast, colorectal, endometrial, ovarian, liver cancer, or Non-Hodgkin’s lymphoma, found that women with 3 to 4 CVD risk factors on average prior to their cancer diagnosis had the highest odds of all-cause mortality30. Shared risk factors between cancer and CVD, such as aging, cigarette smoking, metabolic syndrome, and insulin resistance, may account for higher ASCVD risk among patients with cancer prior to their cancer diagnosis26,31,32. Therefore, ASCVD risk stratification based on predictive CVD risk scores, such as the VA CVD risk score and the ACC/AHA ASCVD score, are recommend as point-of-care tools for not only CVD risk assessment of patients with cancer but also cancer screening31,33,34.
While some studies reported that women with breast cancer had a higher number of CVD risk factors before onset of cancer35, women with breast cancer incidence compared to those without breast cancer were similar or at a lower risk in total and HDL cholesterol, diabetes, current smoking, and Body Mass Index36,37. Instead of using the actual number of CVD risk factors or focusing on one specific risk factor, a patient’s CVD risk is recommended to be assessed using existing prediction risk scores such as the ACC/AHA ASCVD score, and stratified into three ASCVD risk groups, low, mediate, and high risk. This provides a comprehensive assessment of ASCVD risk and guides therapies, management, and prevention. The VA women CVD risk score estimated ASCVD risk higher than ACC/AHA ASCVD score on average by 2.5%, thus lowering risk of undertreated ASCVD. Nonetheless, the present study found similar results using two different ASCVD risk scores in estimating women’s ten-year ASCVD risk score trajectories after cancer diagnosis. Accelerated post-cancer ASCVD risk in women was confirmed by both the VA women CVD risk score and ACC/AHA ASCVD risk score, suggesting results are not due to measurement bias or type of risk score being used. Stratification of CVD risk using ASCVD risk scores helps in preventing, monitoring, and managing CVD risk in women diagnosed with cancer.
In addition to predisposed CVD risk factors in patients with cancer, observed escalated ASCVD risk post-cancer may result from the late effect of certain cancer treatments2. Anthracycline chemotherapy, endocrine therapy (e.g., trastuzumab/pertuzumab), and radiation therapy are well known to be associated with cardiotoxicity and increased risk of heart failure38,39. However, the current evidence of the late effect of these cancer therapies on increased ASCVD risk, with hard ASCVD events such as MI, stroke, and cardiac deaths, is limited and rather inconclusive40, partly due to low participation of females in relevant clinical trials41. Future studies are needed to investigate not only which emergent cancer therapies are associated with significant increases in ASCVD risk among women cancer survivors, but the effects of cumulative cardiotoxicity from multiple cancer therapies as well.
This study also found a dramatic increase in ASCVD risk post-cancer among patients diagnosed with liver cancer; however, this can possibly be explained by sparse data on women liver cancer survivors (n = 21) resulting in overestimating ASCVD risk. The regression results from a small sample data set are known for overestimation.
Patients diagnosed with lung cancer had significantly higher risk of ASCVD pre-cancer than other cancer types, next to bladder and liver cancers, and their ASCVD risk escalated post-cancer with a significant jump at onset of cancer diagnosis. Despite a lower pre-cancer CVD risk among women with thyroid cancer, than the no cancer group, the study found ASCVD risk for women with thyroid cancer had significantly accelerated post-cancer diagnosis. This may be due to receiving radiation therapy and Thyroid Hormone Suppression therapy with or without surgery42. Cancer therapy administered to treat thyroid cancer with or without surgery affects thyroid hormone levels. Either too high or low levels of thyroid hormones can result in cardiac dysfunction43,44.
Contrary to current findings, other studies using the ACC/AHA ASCVD risk score conversely found women with and without breast cancer to have a similar risk of CVD45,46 suggesting the need to examine alternative measures of ASCVD risk, such as the VA women CVD risk score, and recalibration of ACC/AHA ASCVD risk score specific for women diagnosed with cancer.
The VA women CVD risk score was developed using women veterans as a development cohort, thus the VA women CVD risk score may fit better to assess ASCVD risk for the current study population than the ACC/AHA ASCVD scores. In addition, the VA women CVD risk score is an adequate ASCVD assessment tool for both Hispanic women and women between the ages of 30–40 years, while the ACC/AHA ASCVD risks score is not adequate. The ACC/AHA ASCVD risk score was developed using the study cohort of N-H White and N-H Black women aged 40–79, thus is not adequate to assess Hispanic women or women between the ages of 30–40 years. On the contrary, the VA women CVD risk score was developed using the study cohort of women aged 30–79 with three race/ethnic groups—N-H White, N-H Black, and Hispanic.
Our study finding, a greater post-cancer ASCVD risk for women endometrial and gynecological cancer survivors compared to non-cancer women (Fig. 1D), corresponds with prior results29. Interestingly, comparing pre- and post-cancer periods within the endometrial and gynecological cancer group, an increased rate of ASCVD risk was tempered after cancer diagnosis. This result is unexpected and needs further investigation. One possible explanation is heterogeneity among endometrial, uterine, and cervix cancer groups in pathophysiology of cardiotoxicity induced by certain cancer therapies. The current study did not stratify uterine and cervix cancers from endometrial cancer.
Also, it is possible that the observed rise in ASCVD risk scores post-cancer can be accounted for by inflated number of ASCVD risk score data points post-cancer periods. After cancer diagnosis, patients with cancer would require more frequent clinic visits and laboratory test orders compared to pre-cancer to evaluate cancer progression, treatment response, and complications, resulting in more data points post-cancer compared to pre-cancer period. The increased number of data points during the post-cancer period may allow larger variability, including outliers, and result in overestimating of ASCVD trajectory from a linear approximation (GLMM).
The VA’s longitudinal data make it possible to monitor patients’ ASCVD risk before and after cancer diagnosis in women with cancer incidence. The current study was able to compare ASCVD risk score trajectories within and between cancer groups capitalizing on the national VA’s CDW data in the US.
One of the rationales to introduce the VA women CVD risk to assess ASCVD risk for women is a disproportional effect size of aging on ASCVD risk across race groups—N-H White women model includes an age squared term while N-H Black women model does not—in the widely used ACC/AHA ASCVD score19. Despite that lung, bladder, and endometrial cancers were more prevalent among N-H White women veterans than their N-H Black counterparts, the estimates of 10-year ASCVD risk score trajectories for N-H White women between two ASCVD risk scores were similar in these cancer groups (Figs. 1 and 2). Meanwhile, the onset of thyroid cancer was at a significantly younger age (47 years old) than other cancers and the no cancer group (Supplementary Table 1), thus, lower ASCVD risk among women with thyroid cancer is expected.
Despite the study’s strengths, there are several limitations. First, the number of women veteran patients with cancer may have been underestimated since the study only included women diagnosed in the VA health care system. Second, the study’s sample size for VA women patients with liver cancer may be too small for GLMM estimation, which likely accounts for the unexpected finding of a decrease in pre-cancer ASCVD risk in patients with liver cancer. Third, the study did not stratify ASCVD risk based on cancer treatment history and tumor subtypes. Fourth, there were 725 women veterans who developed multiple cancers during the study period. However, the current study did not control for having multiple cancers and its effect on increased ASCVD risk in the model, thus it is possible that ASCVD risk for some cancers was overestimated. Fifth, the study outcome was limited to calculated ASCVD risk scores only and hard cardiovascular events were not evaluated. Lastly, the ACC/AHA ASCVD score may not be appropriate to assess ASCVD risk scores for either women under 40 years of age or those from Hispanic backgrounds. Both VA women CVD risk and AHA ASCVD risk scores may underestimate ASCVD risk for women from other racial and ethnic backgrounds because the current study applied the N-H White ASCVD risk calculator to assess other race and ethnic groups whose calculators are not available. Kidney cancer was excluded due to the scope of the current study, women veterans. Renal cancer incidence rate is significantly greater in the male military population over the age of 40 than in their female counterparts (https://apps.dtic.mil/sti/citations/ADA624265).
In conclusion, accelerated pre- and post-cancer ASCVD risks in women were confirmed by both the VA women CVD risk score and ACC/AHA ASCVD risk score. Women diagnosed with cancer during their lifetime may have faced elevated ASCVD risk long before the onset of their cancer diagnosis which can be further accelerated due to cumulative cardiotoxicity from cancer therapies. The current study added objective evidence of elevated and accelerated ASCVD risk in females diagnosed with cancer, during both pre- and post-cancer periods. This study highlights the need for a more focused cardio-oncology approach on women facing the challenge of cancer care and shared risk reduction strategies (e.g., smoking cessation, diet, and physical activity) coupled with heightened cancer screening in early detection of cancer. Although the current study did not examine a sex difference in ASCVD risk pre- and post-cancer, validated female sex-specific oncology CVD risk assessment tools and prospective clinical studies are needed to expand our knowledge of sex-based differences in risk of ASCVD to further advance the development of cardioprotective treatment strategies. Also, future studies identifying cancer-specific CVD risk factors and incidences other than ASCVD events altered by cancer treatment are warranted.
Data availability
Because of the sensitive nature of the data collected for this study, requests to access the individual-level dataset are limited to qualified VA-affiliated researchers trained in human subject confidentiality. The de-identified summary data will be available upon request. Protocols may be sent to the VA North Texas Health Care System Institutional Review Board (IRB) at NTXIRBAdmin@va.gov. SQL, SAS and R programming code used in the analysis of this study are available from the corresponding author upon reasonable request. All methods were performed in accordance with the relevant guidelines and regulations.
References
Ramin, C. et al. All-cause and cardiovascular disease mortality among breast cancer survivors in CLUE II, a long-standing community-based cohort. J. Natl. Cancer Inst. 113, 137–145 (2021).
Johnson, C. B., Davis, M. K., Law, A. & Sulpher, J. Shared risk factors for cardiovascular disease and cancer: implications for preventive health and clinical care in oncology patients. Can. J. Cardiol. 32, 900–907 (2016).
Florido, R. et al. Cardiovascular disease risk among cancer survivors. J. Am. Coll. Cardiol. 80, 22–32 (2022).
Zamorano, J. L. et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC committee for practice guidelines: the task force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 37, 2768–2801 (2016).
Lyon, A. R. et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS): developed by the task force on cardio-oncology of the European Society of Cardiology (ESC). Eur. Heart J. 43, 4229–4361 (2022).
Bodai, B. I. & Tuso, P. Breast cancer survivorship: a comprehensive review of long-term medical issues and lifestyle recommendations. Perm. J. 19, 48–79 (2015).
Greenlee, H. et al. Risk of cardiovascular disease in women with and without breast cancer: the pathways heart study. J. Clin. Oncol. 40, 1647–1658 (2022).
Chatterjee, K., Zhang, J., Honbo, N. & Karliner, J. S. Doxorubicin cardiomyopathy. Cardiology 115, 155–162 (2010).
Jacobs, J. E. J. et al. Mortality and major adverse cardiac events in patients with breast cancer receiving radiotherapy: the first decade. J. Am. Heart Assoc. 12, e027855 (2023).
Simon, M. S. et al. Cardiometabolic risk factors and survival after breast cancer in the Women’s Health Initiative. Cancer 124, 1798–1807 (2018).
Day, F. R., Elks, C. E., Murray, A., Ong, K. K. & Perry, J. R. B. Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci. Rep. 5, 11208 (2015).
O’Kelly, A. C. et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ. Res. 130, 652–672 (2022).
Collaborative Group on Hormonal Factors in Breast Cancer, Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence, Lancet 394, 1159–1168 (2019).
Parikh, N. I. et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation 143, e902–e916 (2021).
Suter, T. M. & Ewer, M. S. Cancer drugs and the heart: importance and management. Eur. Heart J. 34, 1102–1111 (2012).
Pucci, G. et al. Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: a review of the literature. Pharmacol. Res. 120, 34–42 (2017).
Jeon‐Slaughter, H., Chen, X., Tsai, S., Ramanan, B. & Ebrahimi, R. Developing an internally validated veterans affairs women cardiovascular disease risk score using veterans affairs national electronic health records. J. Am. Heart Assoc. 10, e019217 (2021).
Goff, D. C. et al. 2013 ACC/AHA Guideline on the assessment of cardiovascular risk. Circulation 129, S49–S73 (2014).
Chen, X., Ramanan, B., Tsai, S. & Jeon‐Slaughter, H. Differential impact of aging on cardiovascular risk in women military service members. J. Am. Heart Assoc. 9, e015087 (2020).
Wu, P. et al. Mapping ICD-10 and ICD-10-CM Codes to phecodes: workflow development and initial evaluation. JMIR Med. Inform. 7, e14325 (2019).
Liao, K. P. et al. High-throughput multimodal automated phenotyping (MAP) with application to PheWAS. J. Am. Med. Inform. Assoc. 26, 1255–1262 (2019).
Imbens, G. W. & Lemieux, T. Regression discontinuity designs: a guide to practice. J. Econ. 142, 615–635 (2008).
Hahn, J., Todd, P. & Van der Klaauw, W. Identification and estimation of treatment effects with a regression-discontinuity design. Econometrica 69, 201–209 (2001).
Mehta, L. S. et al. Cardiovascular disease and breast cancer: where these entities intersect: a scientific statement from the American Heart Association. Circulation 137, e30–e66 (2018).
Lyon, A. R. et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur. J. Heart Fail. 22, 1945–1960 (2020).
Koene, R. J., Prizment, A. E., Blaes, A. & Konety, S. H. Shared risk factors in cardiovascular disease and cancer. Circulation 133, 1104–1114 (2016).
Timp, J. F., Braekkan, S. K., Versteeg, H. H. & Cannegieter, S. C. Epidemiology of cancer-associated venous thrombosis. Blood 122, 1712–1723 (2013).
Guha, A. et al. Incidence, risk factors, and mortality of atrial fibrillation in breast cancer: a SEER-Medicare analysis. Eur Heart J. 43, 300–312 (2022).
Soisson, S. et al. Long-term cardiovascular outcomes among endometrial cancer survivors in a large, population-based cohort study. J. Natl. Cancer Inst. 110, 1342–1351 (2018).
Simon, M. S. et al. Cardiometabolic risk factors and survival after cancer in the Women’s Health Initiative. Cancer 127, 598–608 (2021).
Lau, E. S. et al. Cardiovascular risk factors are associated with future cancer. CardioOncology 3, 48–58 (2021).
Zullig, L. L. et al. Cardiometabolic comorbidities in cancer survivors. CardioOncology 4, 149–165 (2022).
Conen, D. et al. Risk of malignant cancer among women with new-onset atrial fibrillation. JAMA Cardiol. 1, 389–396, (2016).
Bell, C. F. et al. Risk of cancer after diagnosis of cardiovascular disease. CardioOncology 5, 431–440, https://doi.org/10.1016/j.jaccao.2023.01.010.
Kim, D. Y. et al. Development and validation of a risk score model for predicting the cardiovascular outcomes after breast cancer therapy: The CHEMO‐RADIAT Score. J. Am. Heart Assoc. 10, e021931 (2021).
Zeng, X. et al. Cardiovascular risk factors and breast cancer incidence in a large middle-aged cohort study. BMC Cancer 22, 534 (2022).
Yandrapalli, S. et al. Risk factors and outcomes during a first acute myocardial infarction in breast cancer survivors compared with females without breast cancer. Am. J. Med. 133, 444–451 (2020).
Denlinger, C. S. et al. Survivorship, Version 2.2018, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 16, 1216–1247 (2018).
Zamorano, J. L. et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines. Eur. J. Heart Fail. 19, 9–42 (2017).
Wilcox, N. S. et al. Sex-specific cardiovascular risks of cancer and its therapies. Circ. Res. 130, 632–651 (2022).
Mahmood, S. S. et al. Myocarditis in patients treated with immune checkpoint inhibitors. J. Am. Coll. Cardiol. 71, 1755–1764 (2018).
Park, J. et al. Risk factors for cardiovascular disease among thyroid cancer survivors: findings from the Utah cancer survivors study. J. Clin. Endocrinol. Metab. 103, 2468–2477 (2018).
Klein, I. & Ojamaa, K. Thyroid hormone and the cardiovascular system. N Engl. J. Med. 344, 501–509 (2001).
Osuna, P. M., Udovcic, M. & Sharma, M. D. Hyperthyroidism and the Heart. Method. Debakey Cardiovasc. J. 13, 60–63, (2017).
Gernaat, S. A. M. et al. The risk of cardiovascular disease following breast cancer by Framingham risk score. Breast Cancer Res. Treat. 170, 119–127 (2018).
Anderson, C., Nichols, H. B., Deal, A. M., Park, Y. M. & Sandler, D. P. Changes in cardiovascular disease risk and risk factors among women with and without breast cancer. Cancer 124, 4512–4519 (2018).
Acknowledgements
This work was supported using resources from the Department of Veterans Affairs (VA) Centralized Interactive Phenomics Resource (CIPHER).
Author information
Authors and Affiliations
Contributions
E.Z.W.: concept and design of the study, literature search, tables and figures, data interpretation, and a manuscript writing. S-H.C.: concept and design of the study, literature search, data interpretation, and a manuscript writing. J.E.D.: literature search, data interpretation, and a manuscript writing. S.D.C.: literature search, data interpretation, and a manuscript writing. H.J-S: concept and design of the study, literature search, tables and figures, study design, data extraction and management, data analysis, data interpretation, and a manuscript writing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Whyne, E.Z., Choi, SH., Dowell, J.E. et al. Ten-year atherosclerotic cardiovascular disease risk trajectories among women veteran cancer patients. npj Womens Health 2, 6 (2024). https://doi.org/10.1038/s44294-024-00007-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44294-024-00007-1