Abstract
NDM-1 comprises a carbapenemase that was first detected in 2008 in New Delhi, India. Since then, NDM-1-producing Klebsiella pneumoniae strains have been reported in many countries and usually associated with intra and inter-hospital dissemination, along with travel-related epidemiological links. In South America, Brazil represents the largest reservoir of NMD-1-producing K. pneumoniae. Here, we focused on the detection and molecular/structural characterization of the blaNDM-1 resistance gene/enzyme from 24 K. pneumoniae clinical isolates in the Midwest region of Brazil. Antimicrobial susceptibility assays showed that all isolates are resistant to carbapenems. Molecular typing of the isolates revealed seven clonal groups among the K. pneumoniae isolates, which may indicate intra or inter-hospital dissemination. Moreover, the blaNDM-1 gene was detected in all 24 K. pneumoniae isolates and the full blaNDM-1 gene was cloned. Bioinformatics analysis showed that the NDM-1 enzyme sequence found in our isolates is highly conserved when compared to other NDM-1 enzymes. In addition, molecular docking studies indicate that the NDM-1 identified binds to different carbapenems through hydrogen and zinc coordination bonds. In summary, we present the molecular characterization of NDM-1-producing K. pneumoniae strains isolated from different hospitals, also providing atomic level insights into molecular complexes NDM-1/carbapenem antibiotics.
Similar content being viewed by others
Introduction
Klebsiella pneumoniae is a Gram-negative bacterium belonging to the Enterobacteriaceae family. This bacterium is a major pathogen associated with nosocomial infections and, for this reason, it is part of the so-called ESKAPE group (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter species), as an analogy to “escape” from the lethal action of antibiotics [1]. K. pneumoniae can be an opportunistic pathogen causing pulmonary, urinary tract, and bloodstream infections, as well as septicemia [2, 3]. Drug-resistant K. pneumoniae isolates are rapidly spreading and have become an important clinical challenge [4]. Carbapenems are last resort β-Lactam drugs used to treat serious bacterial infections [5]. Yet, diverse β-lactamases produced by bacteria can degrade β-lactam antibiotics by cleaving the β-lactam ring (CO–N bond), rendering them inactive [6, 7].
β-Lactamases can be classified according to their primary structure (classes A–D) or their biological function (groups 1–3) [8, 9]. The metallo-β-lactamases (MBLs) are classified as class B members and functional group 3. MBL enzymes require bivalent zinc ions as substrate for the hydrolysis of β-lactam antibiotics, except for aztreonam. Moreover, MBLs are resistant to serine β-lactamase inhibitors [10]. Among the enzymes representing the MBLs is the New Delhi metallo-β-lactamase (NDM). NDM-1 is the most common variant among NDM isolates [11]. NDM-1 comprises a protein with 269-amino acid residues and a molecular mass of ~27.5 kDa [12]. The crystal structure of NDM-1 shows that the active site presents two zinc ions enclosed by loops L3 and L10 [13]. Moreover, the blaNDM-1 resistance gene encoded the NDM-1 enzyme and is found mainly in plasmids and also associated with mobile genetic structures, including insertion sequences, integrons, and transposons, which facilitates its dissemination [14].
In 2008, the first NDM-1 report in K. pneumoniae was investigated in a Swedish patient who traveled to New Delhi (India), and acquired a urinary tract infection [12]. The largest NDM-producer reservoir is on the Asian continent, mainly in China and India, with ~58.15% abundance of the NDM-1 variant [13]. Different species of producing Enterobacteriaceae were found carrying NDM and they are also endemic to the Indian subcontinent, but there are sporadic reports and outbreaks. Additionally, NDM-producing K. pneumoniae outbreaks have been increasing worldwide [15]. The American continent presents ~10.8% abundance of NDM-1-producers. In addition, Paraguay, Argentina, Uruguay, Ecuador, and the rest of Latin America have been considered as minor pools in comparison to Brazil, which is the largest reservoir [13].
In this context, here we detected and characterized the blaNDM-1 resistance gene from K. pneumoniae clinical isolates in the Midwest region of Brazil. The structural investigation of the NDM-1 enzyme from K. pneumoniae isolates binding to the carbapenem antibiotics used in our susceptibility assays was also carried out through molecular docking simulations.
Material and methods
Bacterial isolates
A total of 24 clinical isolates of K. pneumoniae were obtained from the Public Health Laboratory (LACEN-DF). Strains were collected between 2013 and 2014, at different hospitals in Brasília, Federal District (DF), Brazil. Duplicate samples were excluded from strains collection used in present study.
Antimicrobial susceptibility assays
The antimicrobial susceptibility was evaluated by the Microscan WalkAway (Siemens Healthcare Systems) automated system. The antimicrobial agents tested were imipinem (IMP), meropenem (MEM), and ertapenem (ETP). The susceptibility results were interpreted in accordance with the document M100-S22 “Clinical Laboratory Standards Institute” [16]. Bacterial species were identified using the same method cited above, following the manufacturer’s instructions.
Molecular typing
The genomic DNA extraction of the isolates was performed in accordance with Sambrook and Russel [17]. BOX-PCR with BOXA1 primer (5′-CTACGGCAAGGCGACGCTGAC-3′) [18] was used for molecular typing of all isolates. PCR reactions were performed in a volume of 25 μl, using 5 × Green GoTaq buffer, GoTaq DNA polymerase (5 U μl−1), MgCl2 (25 mM), and a dNTP mixture (2 mM) (Promega, USA). Conditions for amplification were as follows: one cycle at 95 °C (7 min), 30 cycles at 94 °C (1 min), 53 °C (1 min), 65 °C (8 min), and a final cycle at 65 °C (16 min). Analysis of the genetic fingerprinting patterns was performed with GelCompar II software (Applied Maths, Belgium). The Pearson correlation coefficient was applied, and cluster analysis was performed using the unweighted pair group method with arithmetic mean (UPGMA); algorithm BOX-PCR genetic profiles were analyzed on BioNumerics version 6.0 (Applied Maths, Belgium) using the band-based Dice coefficient, and the unweighted pair geometric-matched analysis dendrogram with a tolerance position of 1% for optimization and band comparison. The resulting dendrograms were analyzed in order to obtain groups of isolates with at least 85% similarity. Isolates with the same genetic profile were considered to belong to the same clonal group.
Detection of blaNDM-1 gene
Plasmid DNA was extracted using a “Wizard® Plus SV Minipreps DNA Purification System” (Promega), following the manufacturer’s protocol. Plasmid DNA was used for PCR amplification of the blaNDM-1 gene with primers designed by Perfect Invitrogen (Oligoperfect™ Designer), including NDM-1f (TCGATCCCAACGGTGATATT) and NDM-1r (TGGATCAAGCAGGAGATCAA), as well as primers already described in the literature, including NDM-F (GGTTTGGCGATCTGGTTTTC) and NDM-R (CGGAATGGCTCATCACGATC) [19]. Samples were sequenced in an ABI 3130 Genetic Analyzers—Applied Biosystems, using the Sanger method [20, 21]. The sequences were compared on BLASTn (Basic Local Alignment Search Tool—NCBI) [22] against the GenBank database [23]. The phylogenetic tree was constructed using Mega 6.0.
Full gene cloning
Plasmid DNA from the K. pneumoniae isolate (6334725) was the template to amplify the full blaNDM-1 gene. The primers designed based on a GenBank database sequence (gi: 609266902) were: blaNDM-1 F (5′-ATGCTGAATAAAAGGAAAAC-3′) and blaNDM-1 R (5′-TCAGCGCAGCTTGTCGGCCA-3′). The PCR products were analyzed by agarose gel electrophoresis (1%) and purified with QIAEX II® Gel Extraction Kit (QIAGEN), following the manufacturer’s instruction. The purified PCR product was ligated to the plasmid vector pGEM®-T Easy Vector Systems (Promega) and transformed in Escherichia coli DH5α cells by thermal shock. Colony PCR was used to screen for positive blaNDM-1 clones. Extraction and plasmid DNA purification of positive colonies was carried out by alkaline lysis. Presence of recombinant plasmids was further confirmed by PCR using the M13 universal primers, (M13 Fw: 5′-CACGACGTTGTAAAACGAC-3′ and M13 Rv: 5′-GGATAACAATTTCACACAGG-3′). Samples were sequenced in an ABI3730xl DNA Analyzers-Applied Biosystems using the Sanger method [20, 21]. The sequence was analyzed on BLASTn [22] against the GenBank database [23].
NDM-1 enzyme sequence analysis
The nucleotide sequence obtained was translated into amino acids (query sequence) using the ExPASy Translate server [24]. A total of six frames resulting from blaNDM-1 nucleotides sequences translation were obtained from this analysis, and the frame with the highest hit was then selected for further studies. Transmembrane topology and signal peptide prediction was performed using the Phobius server [25]. BLASTp [22] analysis was performed against the Protein Data Bank (PDB) using the protein–protein BLAST algorithm, as well as filtering by organism (K. pneumoniae (taxid: 573)). The identified proteins with high identity, coverage, and low score e-values were selected for further studies. Multiple sequence alignment was performed on ClustalO [26]. Three-dimensional structural visualization was done in PyMOL [27].
Molecular docking
Molecular docking simulations were carried out to predict the atomic interactions involved in the molecular complexes NDM-1/ETP, NDM-1/IMP, and NDM-1/MEM. The ETP, MEM, and IMP structures were obtained from DrugBank [28], parameterized on Maestro v.11 [29] and further used as ligands for docking simulation, whereas the crystal structure of NDM-1 in complex with hydrolyzed ampicillin (PDB entry: 3Q6X) [30] was used as receptor. Grid boxes of 20 × 15 × 15 points and 1 Å spacing were built using AutoDock Tools [31] and centered at the NDM-1 substrate-binding site. NDM-1/carbapenem atomic interactions were calculated. The lowest energy complex for each condition was then submitted to energy minimization (steepest descent) using the GROMOS96 43a1 force field from the GROMACS 5.0.4 computational package [32].
Results
Antimicrobial susceptibility assays
All the isolates studied here were resistant to all the carbapenems tested, including IMP and MEM, with minimum inhibitory concentration (MIC) > 8 µg ml−1 (Table 1), and ETP with MICs from 1 to 4 µg ml−1 (Table 1). All the isolates were identified by the Microscan WalkAway automated system as K. pneumoniae.
Molecular typing
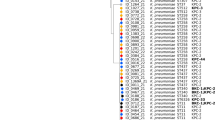
The dendrogram obtained from fingerprinting patterns analysis revealed seven clonal groups (Fig. 1). Three clonal groups, including V–VII, correspond to hospital “G”, whereas clonal group I corresponds to hospital “I”. These data indicated outbreaks in the hospitals from where they were isolated. Isolates constituting the clonal groups II–IV (Fig. 1) emerged from different hospitals, suggesting an inter-hospital spread of these isolates.
BOX-PCR analyses performed with 24 K. pneumoniae isolates. Dendrogram derived from computerized analysis of the BOX PCR-generated DNA fingerprints, as described in the Material and methods. Numbers in bold type represent the identification of K. pneumoniae isolates (6334725, 6418433, 6786412, 4455550, 5240651, 6175670, 6316043, 7027362, 7218678, 5596812, 6354251, 6806328, 6946869, 6946894, 7072558, 7091867, 7164572, 7307939, 4941726, 6381832, 6381868, 6714432, 6975285 and 6533645). Different hospitals were named as A–J
Detection of the blaNDM-1 gene
The blaNDM-1 gene was detected in the 24 K. pneumoniae isolates. The NDM primers designed in the present work resulted in PCR products of ~287 bp (Supplementary information 1A). The NDM-1 primers described in literature [19] resulted in amplicons of ~621 bp (Supplementary information 1B). These latter amplicons were sequenced, and further compared with those from the GenBank [23], which were identified as NDM-1. The phylogenetic tree containing the NDM-1 K. pneumoniae sequences is shown in Fig. 2. The phylogenetic tree presented a bootstrap value of 92%, in which isolates of NDM-1-producing K. pneumoniae identified in this study were clustered with an NDM-1-producing K. pneumoniae (609266902) sequence available at the GenBank [23]. Only the K. pneumoniae isolate (5596812) sequence showed a bootstrap value below 50%. It is worthy mentioning that, at the time this work was performed, only seven NDM-1-producing K. pneumoniae were known and used in these analyses. This fact, along with the bootstrap value obtained for K. pneumoniae isolate (5596812) may indicate an inaccurate classification of this specific NDM-1 isolate. We therefore discarded this isolate for further analyses.
Phylogenetic tree of NDM-1-producing K. pneumoniae isolates. The neighbor-joining and Jukes–Cantor model methods were used. Bootstrap values below 50% were considered inconsistent. Bold numbers: K. pneumoniae isolates from this study (6334725, 6418433, 6786412, 4455550, 5240651, 6175670, 6316043, 7027362, 7218678, 5596812, 6354251, 6806328, 6946869, 6946894, 7072558, 7091867, 7164572, 7307939, 4941726, 6381832, 6381868, 6714432, 6975285 and 6533645); blaNDM-1: blaNDM-1 gene from K. pneumoniae retrieved from the GenBank (access number: 609266902); blaIMP: outgroup (access number: S71932.1)
Cloning of blaNDM-1
The complete blaNDM-1 gene was amplified from plasmid DNA of a K. pneumoniae isolate (6334725) and cloned into E. coli DH5α to obtain the complete blaNDM-1 gene sequence for subsequent analysis at protein level. The cloned DNA sequence of 1122 bp included the inserted sequence with a predicted size of 836 bp. This sequence was compared with sequences from GenBank using BLASTn [22], confirming the identification of complete blaNDM-1 gene.
In silico studies
In order to obtain insights on the three-dimensional structure of the NDM-1 identified, the nucleotide sequence of the blaNDM-1 full gene was translated to amino acids using the ExPASy Translate server [24], resulting in a 270-amino acid residues protein. Six open-reading frames (ORF) were obtained, where 5′ 3′ Frame 3 presented the highest hit and was then selected for further analyses (Supplementary information 2). The N-terminal region of NDM-1 protein contained a signal peptide from residues 1 to 28, which was removed for subsequent studies. BLASTp [22] analyses were performed using the PDB, thus confirming the MBL domain characteristic of NDM-1 members. Moreover, high identities were observed between the query and target sequences. Among them, those associated with the following PDB entries: 4EXS, 4EY2 [33], 3Q6X [30], 4RL2 [34], 4U4L [35], and 5A5Z [36] presented 100% identity and coverage with the query sequence, as well as e-values equal to zero (0.0), indicating no random alignments. These sequences were further submitted to multiple alignments with the NDM-1 query sequence (Supplementary information 3), and it was found that NDM-1 protein (PDB entry: 3Q6X) presented a complete match with the query sequence, whereas other NDM-1 sequences from PDB showed some differences at the N-terminal and/or C-terminal regions due to signal peptides (1–28) and his-tag presence, respectively.
The structure of the NDM-1 protein (PDB entry: 3Q6X) was previously investigated by X-ray crystallography at 1.3 Å resolution [30] and, in our study, it was used as receptor for docking simulations with the β-lactams used in the susceptibility assays, including ETP, IMP, and MEM. The most important conserved residues between the query and 3Q6X sequences include H120, H122, and H189 representing the metal ion-binding site for Zn1; and D124, C208, and H250 representing the same site for Zn2. Residues located around the metal ion-binding sites (Q123, K211, and N220) represent the substrate-binding site [30].
Molecular docking studies were carried out to predict the affinities and atomic interactions for the complexes NDM-1/ETP, NDM-1/IMP, and NDM-1/MEM. As a result, we observed that the highest affinity values were obtained for the complex NDM-1/ETP (−7.6 kcal mol−1), followed by NDM-1/MEM (−5.8 kcal mol−1), and finally NDM-1/IMP (−5.5 kcal mol−1). It is worth highlighting that docking simulations consider atom–atom interactions for binding affinity calculations. We therefore avoided creating a direct parallel between our bacterial susceptibility results (MIC assays) and the docking simulations because of their huge difference in terms of biological complexity. The results observed in the MIC assays comprehend several factors related to K. pneumoniae resistance that were not simulated in silico. We therefore focused on predicting the binding sites and atomic interactions in the antibiotics/NDM-1 complex to shed some light over the mechanism of antibiotics hydrolysis. All the antibiotics evaluated attach to both the metal ion-binding sites and the substrate-binding site (Fig. 3a–c). Moreover, as observed in previous crystallography studies [33], zinc coordination bonds involving Zn1 and Zn2, as well as hydrogen bonds established by residues from the substrate-binding site (Q123, K211 and N220), could be predicted in all complexes (Fig. 3a–c; Table 2). Also in agreement with previous findings [33], all complexes herein studied reveal the role of zinc coordination bonds between NDM-1 metal ion-binding site residues and the oxygen atom from ETP, IMP, and MEM β-lactam rings (Fig. 3a–c), which is known as a crucial first step for β-lactams hydrolysis. Moreover, hydrogen bonds here predicted mainly involved residues from the substrate-binding site, which facilitates the positioning and stabilization of ETP, IMP, and MEM on NDM-1 hydrolysis core.
Discussion
The presence of the blaNDM-1 resistance gene in K. pneumoniae clinical isolates, and the possible dissemination of this gene, is of major concern for public health. Our study identified the blaNDM-1 gene in clinical isolates of K. pneumoniae from different hospitals, and the molecular characterization of these isolates showed the presence of clones among them. The structural studies of the NDM-1 enzyme encoded by the blaNDM-1 gene showed a conserved structure. In addition, molecular docking studies were carried out to predict the interactions between NDM-1 and the β-lactams studied in the susceptibility assays.
This study began with the evaluation of the resistance of K. pneumoniae isolates to carbapenems. Here, we show the MICs of ETP, IMP, and MEM against NDM-1-producing K. pneumoniae isolates, along with the profile of bacterial resistance. These findings corroborate previous data reporting the potential of ETP and IMP to inhibit growth of NDM-producing Enterobacteriaceae isolates with MIC values from 1 to >8 μg ml−1 [37]. Moreover, Wailan et al. [38] observed MICs > 32 μg ml−1 for ETP, IMP, and MEM against 12 NDM-producing Enterobacteriaceae clinical isolates in Australia. A clinical isolate of NDM-1-producing K. pneumoniae from the Pediatric Hospital in Mexico was also inhibited by the treatment with IMP and MEM at 32 and 64 μg ml−1, respectively [39]. In Iran, from 112 clinical isolates of K. pneumoniae, 49 were resistant to IMP and MEM, with MICs > 256 μg ml−1, and six of them were positive for the blaNDM-1 gene [40].
In this study, we also evaluated inter-hospital or intra-hospital dissemination of resistant K. pneumoniae isolates by BOX-PCR. The data here reported for the clonal groups I, V, VI, and VII suggest outbreaks within the hospital from where they were obtained. Comparatively, in Greece, a neonatal outbreak caused by 16 K. pneumoniae isolates was characterized by molecular typing using BOX-PCR, revealing 15 different profiles among the isolates from the different wards of the same hospital [41]. In addition, a study developed in Israeli hospitals suggests intra-institutional transmission of three OXA-48-producing K. pneumoniae isolates [42]. Furthermore, clonal groups II–IV suggest an inter-hospital dissemination. Similarly, Todorova et al. [43] performed the genetic characterization of NDM-1-producing K. pneumoniae clinical isolates from two hospitals in Bulgaria. The authors reported two different fingerprint patterns, which indicated a possible genetic difference between the strains. Accordingly, and considering the potential propagation of this resistance mechanism, they proposed the frequent identification and monitoring of those NDM-producing isolates. Our study has clones of NDM-1-producing K. pneumoniae spread within the same and between different hospitals, thus providing accurate information to encourage the inspection of this dissemination for the control of drug-resistant bacterial infections.
Reports have shown that NDM-1-producing K. pneumoniae infections are associated with high mortality rates [44, 45]. Here, the blaNDM-1 gene was detected in 24 K. pneumoniae isolates from different hospitals of the Midwest region in Brazil. In 2013, the first outbreak of NDM-1-producing K. pneumoniae in South America was reported [46]. A year later, NDM-1 occurrence in a K. pneumoniae isolate was reported in Rio de Janeiro state, Brazil [47]. In the American continent, NDM-producing bacteria were reported in the United States, Mexico, Jamaica, Guatemala, Honduras, Costa Rica, Nicaragua, Colombia, Paraguay, Brazil, Argentina, Uruguay, and Ecuador [13, 48]. NDM is, nowadays, endemic to the Indian subcontinent, Balkan States, North Africa, and Arabian Peninsula. A surveillance study from 2008 to 2012 showed a total of 135 isolates of NDM worldwide, including countries, such as India, Vietnam, Serbia, Egypt, Guatemala, Georgia, Saudi Arabia, Philippines, and the United States. In these countries the blaNDM gene was detected in nine species of Enterobacteriaceae, including 62 K. pneumoniae isolates [37].
The NDM-1 enzyme acts via the hydrolysis of the β-lactam ring in diverse antibiotics, leading to K. pneumoniae resistance. We therefore evaluated the possible structural complexes and atomic interactions between NDM-1 and different antibiotics. The blaNDM-1 gene sequence from K. pneumoniae identified was translated into the NDM-1 enzyme for structural characterization. We observed a complete match with a NDM-1 crystallographic structure deposited in the PDB (PDB entry: 3Q6X). Molecular docking studies were performed between NDM-1 and ETP, IMP and MEM, which are the same antimicrobials used in our susceptibility test. We demonstrated that all antibiotics bind to the hydrolysis pocket in NDM-1 in a similar way to ampicillin, and it might be related to the resistance events herein observed.
In addition, atomic interactions with the β-lactam antibiotic ring from all the antibiotics tested were also observed, corroborating other structural studies regarding NDM-1-producing K. pneumoniae [30, 33, 49]. The crystal structure used in our in silico studies (PDB entry: 3Q6X), was firstly reported by Zhang et al. [30]. In that work, ampicillin was used as a substrate for NDM-1. Similarly to our findings, the oxygen atom from the β-lactam carboxylate group was always involved in atomic interactions with residues from NDM-1 that are known to participate in the hydrolysis process [30].
In another study, molecular dynamics simulations were carried out to characterize the binding affinity between IMP and NDM-1 [49]. In accordance with our results, H120, H122, and H189 residues from NDM-1 were involved in Zn1 coordination bonds, whereas D124, C208, and H250 residues from this same enzyme contributed to IMP stabilization in NDM-1-binding site through Zn2 coordination bonds [49]. Thus, the substrate (IMP) recognition occurred through the carboxyl and carbonyl groups from the β-lactam ring, which has oxygen atoms interacting with NDM-1 zinc ions [49]. This bonding pattern was also observed in our study regarding the NDM-1/IMP complex. Moreover, the characterization of MEM hydrolysis by NDM-1 was previously observed. King et al. [33], for instance, observed that the oxygen atom (O71) from MEM formed a hydrogen bond with the NH2 nitrogen atom from the N220 of NDM-1, thus suggesting the potential role of this direct interaction for MEM inactivation [33]. Interestingly, the same interaction was also observed in our study.
Conclusions
Here, the blaNDM-1 resistance gene was found in 24 clinical isolates of K. pneumoniae yielding seven clonal groups from different hospitals in Brasília, Brazil. These data suggest a clear dissemination of K. pneumoniae bacteria, which is probably due to the spread of the blaNDM-1 gene within and among hospitals. The NDM-1 enzyme has a highly conserved structure, which hinders the action of different antimicrobials, as suggested by our molecular docking simulations, and compared to previous structural data. Detailed study of this structure may aid in the development of new NDM-1 inhibitors, which can be administered along with β-lactams. Therefore, the detection of NDM-1-producing K. pneumoniae in hospitals is of great importance for possible prevention of the dissemination of this gene, which is of huge concern worldwide.
References
Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis. 2008;197:1079.
Shon AS, Bajwa RP, Russo TA. Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: a new and dangerous breed. Virulence. 2013;4:107–18.
Janda JM. The Genus Klebsiella: an ever-expanding panorama of infections, disease-associated syndromes, and problems for clinical microbiologists. Clin Microbiol Case Rep. 2015;1:7.
Iraz M, Ozad Duzgun A, Sandalli C, Doymaz MZ, Akkoyunlu Y, et al. Distribution of β-lactamase genes among carbapenem-resistant Klebsiella pneumoniae strains isolated from patients in Turkey. Ann Lab Med. 2015;35:595–601.
Lutgring JD, Limbago BM. The problem of carbapenemase-producing-carbapenem-resistant-Enterobacteriaceae detection. J Clin Microbiol. 2016;54:529–34.
Livermore DM, Woodford N. The β-lactamase threat in Enterobacteriaceae, Pseudomonas and Acinetobacter. Trends Microbiol. 2006;14:413–20.
Livermore DM. β-lactamases in laboratory and clinical resistance. Clin Microbiol Rev. 1995;8:557–84.
Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39:1211–33.
Bush K, Jacoby GA. Updated functional classification of β-lactamases. Antimicrob Agents Chemother. 2010;54:969–76.
Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-β-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005;18:306–21.
Meini MR, Llarrull LI, Vila AJ. Evolution of metallo-β-lactamases: trends revealed by natural diversity and in vitro evolution. Antibiotics. 2014;3:285–316.
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, et al. Characterization of a new metallo-β-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–54.
Khan AU, Maryam L, Zarrilli R. Structure, genetics and worldwide spread of New Delhi metallo-β-lactamase (NDM): a threat to public health. BMC Microbiol. 2017;17:101.
Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med. 2012;18:263–72.
Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014;20:821–30.
CLSI. M100-S22Cd—Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement. Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2012.
Sambrook J, Russel DW. Molecular cloning: a Laboratory manual. 3rd ed. New York, NY:Cold Spring Harbor Laboratory Press; 2001.
Versalovic J, Schneider M, de Bruijin FJ, Lupski JR. Genomic fingerprinting of bacteria using repetitive sequence-based polymerase chain reaction. Methods Mol Cell Biol. 1994;5:25–40.
Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011;70:119–23.
Sanger F, Air GM, Barrell BG, Brown NL, Coulson AR, et al. Nucleotide sequence of bacteriophage phi X174 DNA. Nature. 1977;265:687–95.
Sanger F, Nicklen S, Coulson AR. DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA. 1977;74:5463–7.
Korf I, Yandell M, Bedell J. BLAST: an essential guide to the basic local alignment search tool. 2003.
Benson DA, Karsch-Mizrachi I, Lipman DJ, Ostell J, Wheeler DL. GenBank. Nucleic Acids Res. 2005;33:D34–D38.
Gasteiger E, Gattiker A, Hoogland C, Ivanyi I, Appel RD, et al. ExPASy: the proteomics server for in-depth protein knowledge and analysis. Nucleic Acids Res. 2003;31:3784–8.
Kall L, Krogh A, Sonnhammer EL. A combined transmembrane topology and signal peptide prediction method. J Mol Biol. 2004;338:1027–36.
Sievers F, Wilm A, Dineen D, Gibson TJ, Karplus K, et al. Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol Syst Biol. 2011;7:539.
Delano W. The PyMOL Molecular Graphics System, Version 2.0 Schrödinger, LLC. 2002.
Law V, Knox C, Djoumbou Y, Jewison T, Guo AC, et al. DrugBank 4.0: shedding new light on drug metabolism. Nucleic Acids Res. 2014;42:D1091–97.
Maestro. New York, NY: Schrödinger, LLC; 2017.
Zhang H, Hao Q. Crystal structure of NDM-1 reveals a common β-lactam hydrolysis mechanism. FASEB J. 2011;25:2574–82.
Morris GM, Huey R, Lindstrom W, Sanner MF, Belew RK, et al. AutoDock4 and AutoDockTools4: automated docking with selective receptor flexibility. J Comput Chem. 2009;30:2785–91.
Abraham MJ, Murtola T, Schulz R, Páll S, Smith JC, et al. GROMACS: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX. 2015;1:19–25.
King DT, Worrall LJ, Gruninger R, Strynadka NC. New Delhi metallo-β-lactamase: structural insights into β-lactam recognition and inhibition. J Am Chem Soc. 2012;134:11362–5.
Feng H, Ding J, Zhu D, Liu X, Xu X, et al. Structural and mechanistic insights into NDM-1 catalyzed hydrolysis of cephalosporins. J Am Chem Soc. 2014;136:14694–7.
Gonzalez MM, Kosmopoulou M, Mojica MF, Castillo V, Hinchliffe P, et al. Bisthiazolidines: A substrate-mimicking scaffold as an inhibitor of the NDM-1 carbapenemase. ACS Infect Dis. 2015;1:544–54.
Klingler FM, Wichelhaus TA, Frank D, Cuesta-Bernal J, El-Delik J, et al. Approved drugs containing thiols as inhibitors of metallo-β-lactamases: Strategy to combat multidrug-resistant bacteria. J Med Chem. 2015;58:3626–30.
Biedenbach D, Bouchillon S, Hackel M, Hoban D, Kazmierczak K, et al. Dissemination of NDM metallo-β-lactamase genes among clinical isolates of Enterobacteriaceae collected during the SMART global surveillance study from 2008 to 2012. Antimicrob Agents Chemother. 2015;59:826–30.
Wailan AM, Paterson DL, Kennedy K, Ingram PR, Bursle E, et al. Genomic characteristics of NDM-producing Enterobacteriaceae isolates in Australia and their blaNDM genetic contexts. Antimicrob Agents Chemother. 2016;60:136–41.
Barrios HS-SJ, Reyna-Flores F, Sanchez-Perez A. Detection of a NDM-1-producing Klebsiella pneumoniae (ST22) clinical isolate at a pediatric hospital in Mexico. Pediatr Infect Dis J. 2014;33:335.
Fazeli H, Norouzi-Barough M, Ahadi AM, Shokri D, Solgi H. Detection of New Delhi metallo-β-lactamase-1 (NDM-1) in carbapenem- resistant Klebsiella pneumoniae isolated from a university hospital in Iran. Hippokratia. 2015;19:205–9.
Mavroidi A, Liakopoulos A, Gounaris A, Goudesidou M, Gaitana K, et al. Successful control of a neonatal outbreak caused mainly by ST20 multidrug-resistant SHV-5-producing Klebsiella pneumoniae, Greece. BMC Pediatr. 2014;14:8.
Adler A, Hussein O, Ben-David D, Masarwa S, Navon-Venezia S, et al. Persistence of Klebsiella pneumoniae ST258 as the predominant clone of carbapenemase-producing Enterobacteriaceae in post-acute-care hospitals in Israel, 2008-13. J Antimicrob Chemother. 2015;70:89–92.
Todorova B, Sabtcheva S, Ivanov IN, Lesseva M, Chalashkanov T, et al. First clinical cases of NDM-1-producing Klebsiella pneumoniae from two hospitals in Bulgaria. J Infect Chemother. 2016;22:837–40.
Gamal D, Fernandez-Martinez M, Salem D, El-Defrawy I, Montes LA, et al. Carbapenem-resistant Klebsiella pneumoniae isolates from Egypt containing blaNDM-1 on IncR plasmids and its association with rmtF. Int J Infect Dis. 2016;43:17–20.
Khalil MA, Elgaml A, El-Mowafy M. Emergence of multidrug-resistant New Delhi metallo-β-lactamase-1-producing Klebsiella pneumoniae in Egypt. Microb Drug Resist 2016;23:480–7.
EN PérezJAE, Castro-Cardozo B, Márquez IAV, Aguilar MIG, de la Barrera LM, Barreto ERB, Marquez-Ortiz RA, Guayazán MVM, Gómeza NV. Outbreak of NDM-1-producing Klebsiella pneumoniae in a neonatal unit in Colombia. Antimicrob Agents Chemother. 2013;57:1957–60.
Pereira PS, Albano RM, Asensi MD, Carvalho-Assef AP. Draft genome sequences of three NDM-1-producing Enterobacteriaceae species isolated from Brazil. Mem Inst Oswaldo Cruz. 2015;110:580–2.
Seija V, Medina Presentado JC, Bado I, Papa Ezdra R, Batista N, et al. Sepsis caused by New Delhi metallo-β-Lactamase (blaNDM-1) and qnrD-producing Morganella morganii, treated successfully with fosfomycin and meropenem: case report and literature review. Int J Infect Dis. 2015;30:20–26.
Kim Y, Cunningham MA, Mire J, Tesar C, Sacchettini J, et al. NDM-1, the ultimate promiscuous enzyme: substrate recognition and catalytic mechanism. FASEB J. 2013;27:1917–27.
Acknowledgements
We thank the Laboratório Central de Saúde Pública (LACEN-DF) for providing the isolates, as well as the Laboratório S-Inova Biotech—Universidade Católica Dom Bosco (UCDB), where the research was carried out. Thanks are also due to CESAM (UID/AMB/50017—POCI-01-0145-FEDER-007638) by FCT/MEC through national funds, to the co-funding by FEDER, within the PT2020 Partnership Agreement and Compete 2020, which supports it. This work was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Fundação de Apoio ao Desenvolvimento do Ensino, Ciência e Tecnologia do Estado de Mato Grosso do Sul (FUNDECT), and Fundação de Apoio à Pesquisa do Distrito Federal (FAPDF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Melgarejo, J.L., Cardoso, M.H., Pinto, I.B. et al. Identification, molecular characterization, and structural analysis of the blaNDM-1 gene/enzyme from NDM-1-producing Klebsiella pneumoniae isolates. J Antibiot 72, 155–163 (2019). https://doi.org/10.1038/s41429-018-0126-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-018-0126-z